Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.17 no.51 Murcia jul. 2018 Epub 01-Jul-2018
https://dx.doi.org/10.6018/eglobal.17.3.286281
Originals
Effect of telephone monitoring on adherence to treatment in patients with heart failure
1 Profesora Asociada. Facultad de Enfermería, Pontificia Universidad Javeriana. Bogotá, Colombia. dachury@javeriana.edu.co
2Enfermera coordinadora. Clínica de Falla Cardiaca. Hospital Universitario San Ignacio. Bogotá, Colombia
3Enfermera. Unidad de Cuidado Intensivo, Hospital Universitario San Ignacio. Bogotá, Colombia
4 Cardióloga. Hospital Universitario Fundación Santa Fe de Bogotá. Hospital Universitario Mayor - Méderi. Bogotá, Colombia
Objective:
This work sought to determine the effect of telephone monitoring on levels of adherence to pharmacological and non-pharmacological treatment in patients attending a heart failure program in a tier IV health care institution.
Method:
Controlled clinical trial (n = 61) in which patients were randomized to telephone monitoring or to usual monitoring. To determine the effect of the intervention, three measurements were made of the adherence levels: prior to monitoring, at 12 months, and 6 months after finishing the monitoring. The Cochran-Armitage trend test was used, along with a multivariate analysis with a quantile mixed logistic model.
Results:
Patients with telephone monitoring tended to classify in levels of greater adherence than those from the control group (p < 0.0001). The multivariate model shows an association between the adherence scores and the telephone monitoring, which depend on time, percentiles studied, and the distribution. There was greater adherence with the intervention of the second visit in the distribution’s low quantiles (P10 and P25) and, in the third, in the highest quantiles (P50, P75, and P90). Variables, like male gender (P10 and P25), university schooling (P10 and P90), and presence of a caregiver (P90) were associated with higher adherence levels.
Conclusions:
Telephone monitoring becomes an effective intervention that promotes motivation, self-management, and assertive communication with patients, whenever it is carried out in standardized manner.
Keywords: monitoring studies; telenursing; heart failure; adherence
INTRODUCTION
Cardiovascular diseases are the principal cause of morbidity and mortality globally, with heart failure (HF) being the principal cause of hospitalization. The natural history of the disease is characterized by frequent decompensations that are usually more costly and prolonged, and occur in up to half the cases due to inadequate adherence to pharmacological and non-pharmacological management 1. The average cost of hospitalization for a patient with heart failure who has had decompensations was $6,427,887 COP (D. E. 9,663,176), representing the highest proportion of the annual cost of the disease (29.1%) 2. The principal cause of these decompensations was inadequate adherence 2.
The aforementioned shows the need to work hard in promoting adherence to treatment. For this reason, some strategies have been developed ranging from multidisciplinary care, promotion of education, home visits, and ambulatory monitoring in the short, mid, and long term, where the nursing professional plays a leading role and becomes a fundamental part to guarantee success in compliance with the treatment.
Some barriers exist in implementing these strategies, like difficulty to access programs, the absence of captive population, distances between the patient’s home and the institution assigned for controls, and deficit in the availability of nursing professionals for the implementation and monitoring of patients; making it necessary to start using novel, simple, low-cost strategies, which improve the quality of nursing care, such as telenursing. This is based on using technology and telecommunications in nursing to improve patient care 3. In telecommunications, telephone monitoring becomes a simple and economic tool that promotes the continuum of care and self-management of the disease, and helps individuals to better understand their health problem and treatment. Simultaneously, it improves therapeutic adherence, provides patients and caregivers the knowledge needed to live with their chronic condition, improves the quality of nurse-patient communication, permits establishing a therapeutic relationship with patients so they feel recognized and satisfied with the care provided, and optimizes prevention and early identification of complications. In the United States, nearly 46% of these nursing home visits could reasonably be substituted by telenursing services 4.
Upon reviewing the literature, international studies were found that have demonstrated that this strategy can diminish the number of un-programmed readmissions or even reduce mortality, becoming a cost-effective intervention led by nursing professionals 5,6. A review conducted by Cochrane Collaboration concludes that very little evidence exists on the effect this strategy could have in mid-term, and particularly the persistence of its action after finishing, which elucidates the need to carry out more studies that validate this strategy in promoting adherence to treatment 7. The aim of this study was to determine the effect of telephone monitoring on the levels of adherence to pharmacological and non-pharmacological treatment in patients attending a heart failure program in a tier IV health care institution during the period comprised between June 2014 and June 2016.
METHODS
Design, population, and sample size
A clinical experiment was performed in patients diagnosed with HF who attended outpatient consultation in the heart failure clinic in a tier IV Hospital. Inclusion criteria were: over 18 years of age with II and III functional class, who do not require more than one consultation per month and who were in optimal pharmacological treatment for at least two months; without cognitive deficit evaluated by a score above 24 points on the mini-mental scale; with access to a telephone line. The sample size corresponded to 61 subjects, with an alpha-type error of 5% and 15% loss adjustment, assigned randomly through simple probabilistic sampling (table of random numbers) to the intervention groups. The study excluded patients with functional class IV and who were in palliative treatment and on waiting list for cardiac transplant.
Interventions (intervention-control groups)
The intervention group, besides the usual management offered in the heart failure clinic - based on medical controls every three months and completion of five educational sessions - received telephone monitoring under the telenursing model by Larson Dahn 8, where the nursing professional established a therapeutic relationship with the patient based on trust and empathy, promoted motivation, recognized and reinforced adherence behaviors, facilitated reminders, and solved inquiries. Follow-up frequency was every 30 days until completing 12 months. The nurses who conducted the follow up were masked for the study’s principal outcome. To control co-intervention (reinforcement of telephone monitoring), the cardiologist was blinded. The control group received the usual management by the heart failure clinic.
Principal outcome
The principal outcome was the change in ranges to determine the adherence level.
Instrument
Levels of adherence to pharmacological and non-pharmacological treatments of patients with heart failure were evaluated with the instrument Evaluation of adherence behaviors to pharmacological and non-pharmacological treatment in patients with heart failure9. It has 10 domains: trust in the health professional, accessibility to health services, knowledge in managing the pharmacological treatment, acceptance of the disease, recognition of the warning signs and symptoms, social support, weight maintenance, knowledge of the adequate diet, engaging in physical activity, and mood.
The instrument has a Likert-type response scale with four answer options, where one (never or nothing) means the lowest value of adherence and four (much or always) the highest. The total minimum value a patient could obtain was 30 points and the maximum was 120 points. Patients were considered non-adherent when they scored between 30 and 55; poor adherence, between 56 and 80; frequently adherent, between 81 and 105; and adhered between 106 and 120. The instrument has a reliability index of 0.7213, which is considered adequate 9. In addition, a complementary file was used containing the sociodemographic variables (age, gender, marital status, schooling, occupation, and caregiver) and relevant and pertinent clinical variables of the adherence to treatment (etiology, comorbidity, ejection fraction, time of the diagnosis, and permanence in the heart failure clinic).
Procedure
Prior to performing these interventions object of study, the informed consent was signed voluntarily. The nurses who conducted the telephone monitoring were experts in caring for patients with HF and received training on therapeutic communication and motivation to standardize the Larson model 8. To carry out the monitoring, an electronic application was designed containing the behaviors of adherence to the pharmacological and non-pharmacological treatment patients had to display. The tool had a system of warnings to detect decompensations and, together with the cardiologist, timely decisions were made to avoid complications. In the intervention group three measurements were made of the adherence levels: before monitoring, at 12 months, and six months after ending the monitoring. The control group had three measurements with the same time interval as in the intervention group with habitual management.
Analysis plan
Quantitative variables were summarized with medians, minimums, maximums, and quartiles. Qualitative variables were summarized with absolute and relative frequencies. Quantile-quantile plots were used to determine if the variables followed a Gaussian distribution 10. Domain distributions were presented with box and whisker plots. Both were stratified by the assignation. Association between telephone monitoring and levels of adherence of the scale was conducted with the Cochran-Armitage trend test (20,000 Monte Carlo iterations). In addition, a multivariate analysis was performed with a quantile mixed logistic model through the method by Bottai 11. This model is useful when the outcome has specific minimums and maximums; in the case of the scale, 30 and 120. Furthermore, it permits analyzing the associations in different sectors of the distribution. For this regression, percentiles 10, 25, 50, 75, and 90 were evaluated. Variables, like age (continuum), gender, schooling, presence of a caregiver, number of comorbidities and BNP (logarithm) were included in the model to increase their statistical power, given that they have a known association with the score on the adherence scale. A random intercept was included to adjust for the correlation among measurements in the same subject, with a composite symmetry covariance matrix. The interaction between the assignation and time of these visits was also included in the model. Confidence intervals at 95% (95%CI) were obtained of the odds ratios (OR), through 500 bootstrap iterations. The Akaike information criterion and the log-likelihood were used to evaluate the fit of the model. Patients were analyzed in the groups to which they were randomized. The analysis was run with the R statistical program (version 3.3.2) and the coin and lqmm packages 12-14.
Ethical aspects
The study protocol and design was approved by the Ethics Committee of the Faculty of Nursing at Pontificia Universidad Javeriana (Bogotá) with Resolution 003 2014. Likewise, this research was approved by the research committee of the tier IV health care institution where the participants were recruited. Participation of the individuals in the research was voluntary. To enter the study, written informed consent was requested from the patients. All the procedures were conducted according to International Ethical Guidelines for Biomedical Research on Human Beings and the Scientific, Technical, and Administrative Norms for Health Research of Resolution 008430 by the Ministry of Health of the Republic of Colombia.
RESULTS
Between November 2014 and January 2015, the study evaluated 120 outpatients diagnosed with HF in a tier IV health care institution. Of the patients evaluated, 63 (52.5%) fulfilled the inclusion criteria; 57 (47.5%) of the eligible patients were excluded due to hypoacusis, not having land or mobile telephone lines, being in pre-transplant study, and not accepting participation in the study. In total, 63 patients were randomized: 29 in the intervention group and 34 in the control group. Two patients from the control group perished one month before starting the intervention.
Sociodemographic and clinical variables of the participants
The sociodemographic and clinical variables of the participants in the intervention and control groups are shown in Table 1. The continuous variables did not have a Gaussian distribution and were summarized with the median.
Table 1 Characteristics (Sociodemographic and Clinical) (n = 63)
| Characteristic | Intervention | Control | Total |
|---|---|---|---|
| (n = 29) | (n = 34) | ||
| Age - years | |||
| Median (min. - max.) | 68 (24 - 84) | 58 (40 - 86) | 59 (24 - 86) |
| Distribution - n (%) | |||
| 20-44 | 5 (17.2) | 14 (41.2) | 19 (30.2) |
| 45-64 | 9 (31.0) | 7 (20.6) | 16 (25.4) |
| >65 | 15 (51.7) | 13 (38.2) | 28 (44.4) |
| Gender - n (%) | |||
| Female | 13 (44.8) | 20 (58.8) | 33 (52.4) |
| Male | 16 (55.2) | 14 (41.2) | 30 (47.6) |
| Marital status - n (%) | |||
| Married | 19 (65.5) | 20 (58.8) | 39 (61.9) |
| Common-law | 2 (6.9) | 2 (5.9) | 4 (6.3) |
| Separated | 3 (10.3) | 0 | 3 (4.8) |
| Single | 3 (10.3) | 6 (17.6) | 9 (14.3) |
| Widowed | 2 (6.9) | 4 (11.8) | 6 (9.5) |
| Not observed | 0 | 2 (5.9) | 2 (3.2) |
| Schooling - n (%) | |||
| Primary | 13 (44.8) | 13 (38.2) | 26 (41.3) |
| Secondary | 10 (34.5) | 14 (41.2) | 24 (38.1) |
| University | 5 (17.2) | 5 (14.7) | 10 (15.9) |
| None | 1 (3.4) | 0 | 1 (1.6) |
| Not observed | 0 | 2 (5.9) | 2 (3.2) |
| Occupation - n (%) | |||
| Employed | 6 (20.7) | 6 (17.6) | 12 (19.0) |
| Independent | 7 (24.1) | 5 (14.7) | 12 (19.0) |
| Homemaker | 4 (13.8) | 10 (29. 4) | 14 (22.2) |
| Pensioned | 11 (37.9) | 6 (17.6) | 17 (27.0) |
| Unemployed | 1 (3.4) | 0 | 1 (1.6) |
| Other | 0 | 5 (14.7) | 5 (7.9) |
| Not observed | 0 | 2 (5.9) | 2 (3.2) |
| Caregiver - n (%) | |||
| Spouse | 14 (48.3) | 15 (44.1) | 29 (46.0) |
| Offspring | 5 (17.2) | 4 (11.8) | 9 (14.3) |
| Others | 6 (20.7) | 3 (8.8) | 9 (14.3) |
| None | 4 (13.8) | 12 (35.3) | 16 (25.4) |
| Etiology - n (%) | |||
| Ischemic | 11 (37.9) | 13 (38.2) | 24 (38.1) |
| Valvular | 4 (13.8) | 4 (11.8) | 8 (12.7) |
| Hypertensive | 1 (3.4) | 2 (8.8) | 4 (6.3) |
| Chagasic | 3 (10.3) | 5 (14.7) | 8 (12.7) |
| Congenital | 1 (3.4) | 0 | 1 (1.6) |
| Cardiotoxicity | 1 (3.4) | 2 (5.9) | 3 (4.8) |
| Multifactorial | 4 (13.8) | 0 | 4 (6.3) |
| Idiopathic | 3 (10.3) | 3 (8.8) | 6 (9.5) |
| Other | 0 | 1 (2.9) | 1 (1.6) |
| Not observed | 1 (3.4) | 3 (8.8) | 4 (6.3) |
| Comorbidities - n (%) | |||
| Arterial hypertension | 12 (41.4) | 14 (41.2) | 26 (41.3) |
| Dyslipidemia | 14 (48.3) | 13 (38.2) | 27 (42.9) |
| Cerebrovascular Disease | 4 (13.8) | 6 (17.6) | 10 (15.9) |
| Diabetes Mellitus | 3 (10.3) | 5 (14.7) | 8 (12.7) |
| Hypothyroidism | 12 (41.4) | 13 (38.2) | 25 (39.7) |
| Renal insufficiency in dialysis | 5 (17.2) | 2 (5.9) | 7 (11.1) |
| COPD | 3 (10.3) | 7 (20.6) | 10 (15.9) |
| Chagas Disease | 3 (10.3) | 1 (2.9) | 4 (6.3) |
| Dementia | 13 (44.8) | 11 (32.4) | 24 (38.1) |
| Ejection Fraction* - % | 35 (15 - 65) | 40.5 (15.0 - 60.0) | 36.0 (15.0 - 65.0) |
| Time of Diagnosis - years | 6.0 (2.0 - 21.0) | 6.0 (2.0 - 21.0) | 6.0 (2.0 - 21.0) |
| Time in the Clinic - years | 4.0 (1.0 - 15.0) | 3.0 (0.2 - 12.0) | 4.0 (0.2 - 15.0) |
Source: data derived from the investigation
Among these sociodemographic variables, it is highlighted that the prevalent age in the control and intervention groups was those over 65 years of age, married, and primary level schooling, followed by secondary and university levels. Regarding gender in the intervention group, there were slightly more males than in the control group. In terms of occupation in the intervention group, most were pensioned and in the control group these were dedicated to home activities. In the intervention group, most of the participants had a caregiver, unlike the case for the control group. The most prevalent clinical variables in the control and intervention groups were ischemic etiology, functional class II, comorbidities like arterial hypertension, dyslipidemia, dementia and hypothyroidism. The ejection fraction was between 35% and 40%, and the time of diagnosis of the disease was of six years, with a length of permanence in the heart failure clinic between 3 and 4 years. The characteristics of the two patients in the control group who passed away are presented because they were included, although they died before monitoring started.
Primary outcome: effect of telephone monitoring on the level of adherence in the control and intervention groups
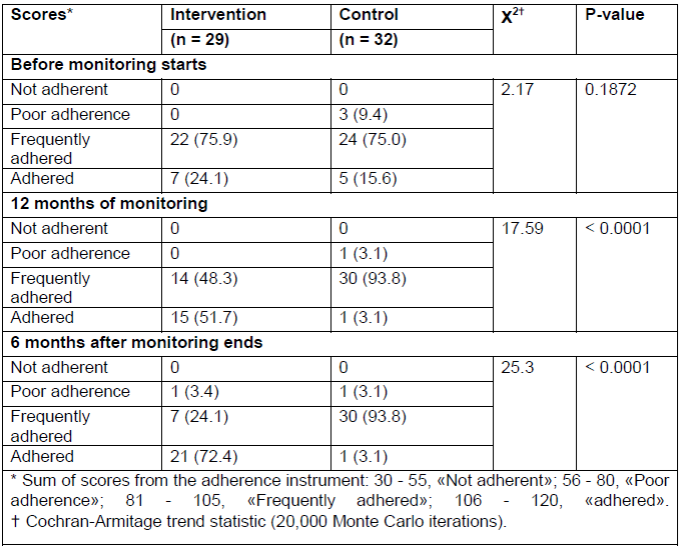
Table 2 shows that patients in the control group remain on the «frequently adhered» level at 12 months of monitoring and six months after ending such. On the contrary, the intervention group evidences an increase in the classification of patients in the «adhered» level, six months after ending the intervention (p < 0.0001).
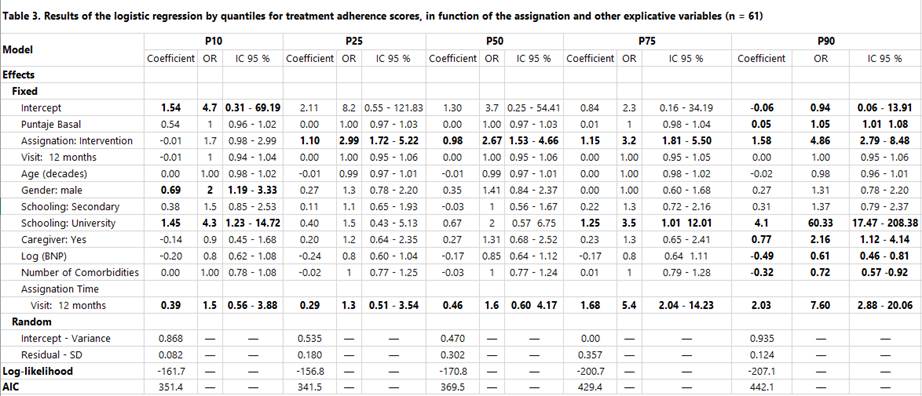
To improve the statistical power, a quantile mixed logistic model was carried out for levels of adherence to treatment in function of the assignation (intervention) and other explicative variables (age, gender, schooling, caregiver, comorbidities, BNP, time). See Table 3.
Table 3 Results of the logistic regression by quantiles for treatment adherence scores, in function of the assignation and other explicative variables (n = 61)
Source: Created by the authors
The multivariate analysis found an interaction between the time of the measurement and the telephone monitoring. Patients in the low percentiles of the distribution (P10 - P25) had an association between the intervention and higher adherence score at 12 months of monitoring (P10: OR 1.97 95%CI 1.27 - 3.04; P25: 1.68 95%CI 1.10 - 2.58). A similar trend is noted at six months after ending the monitoring, but it does not reach statistical significance (P10: OR 2.04 95%CI 0.61 - 6.80; P25: 1.93 95%CI 0.59 - 6.35). In the middle of the distribution (P50 - P75), there was association between the intervention and higher adherence scores at 12 months (P50: OR 2.23 95%CI 1.45 - 3.42; P75: OR 1.81 95%CI 1.18 - 2.78) and six months after ending (P50: OR 3.47 95%CI 1.01 - 11.88; P75: OR 7.84 95%CI 2.96 -27.24). In the 90th percentile, there is a strong association between the intervention and the adherence scores six months after the telephone monitoring (OR 15.43 95%CI 4.27 - 55.75).
The model also shows that variables, like male gender (P10 and P25), university schooling (P10 and P90), and presence of a caregiver (P90) were associated with higher levels of adherence.
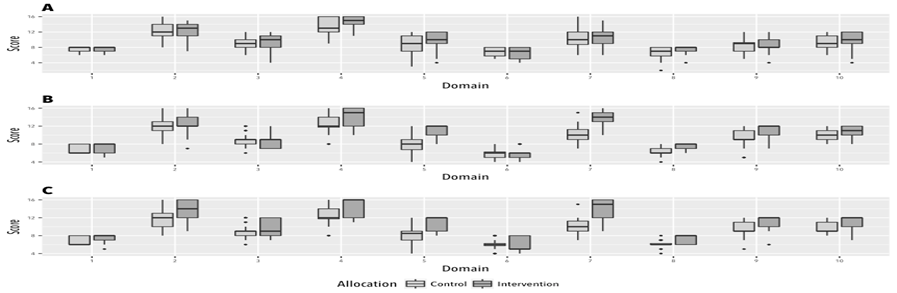
Box and whisker plot of the distribution of scores by domains of the adherence scale among patients with telephone monitoring and controls. A. Prior to the intervention. B. Twelve months of monitoring. C. Six months after monitoring. Domain 1: trust in the professional (range: 2-8); domain 2: knowledge of the pharmacological treatment (range: 4-16); domain 3: accessibility to health services (range: 3-12); domain 4: accepts the diagnosis (4-16); domain 5: recognizes warning signs (3-12); domain 6: seeks external reinforcement to comply with behaviors (2-8); domain 7: maintains weight within the adequate range (4-6); domain 8: knows the recommended diet (4-8); domain 9: engages in physical activity (3-12); domain: mood (3-12).
It should be highlighted that the domains in the intervention group, which showed a positive improvement trend during the second and third measurements, were those related with maintaining weight within the recommended range, engaging in daily exercise, recognizing warning signs, and knowing the recommended diet. The behavior of the prior domains mentioned in the control group evidences that, over time, the tendency is to diminish the level of adherence in essential conducts to reduce the probability of decompensations.
DISCUSSION
Prior to beginning the telephone monitoring, it was determined that most of the patients from the control and intervention groups were frequently adhered. This result may have been because the level of adherence was measured during a very short period of time after having received the educational sessions, yielding as a result informed patients to modify temporarily some conducts. This temporary modification of conducts is not sufficient, given that HF is a disease that occupies the patient’s whole life and requires an active person and responsible for their care, capable and trained to remain totally adhered to their pharmacological and non-pharmacological treatment to reduce complications and improve their quality of life, thus, requiring mid- and long-term monitoring. Continuous clinical monitoring of patients with HF is considered a 1A recommendation in the European guide on the treatment of heart failure, 2016 15.
At 12 months of ending telephone monitoring, it is evident that the intervention group achieved statistical and clinical significance in the adherence levels of patients with heart failure. This result coincides with that found by Comin 16, Riegel 17, Hernández 18, Domingo 19, and Cañón 20, which consider structured monitoring among these strategies of tele-monitoring that promote a successful transition; improve self-care, adherence, quality of life, and reduce hospital readmissions. Likewise, they highlight that tele-monitoring must be aimed at the population at higher risk, like patients with reduced ejection fraction or who have had more than one readmission per year.
Furthermore, a multicenter randomized telephone intervention study (DIAL study) demonstrated that a telephone intervention during a 12-month period was able to significantly reduce the primary end point (internment and/or death) because of adequate adherence and self-care, a result that agrees with that found in our study where, upon ending the 12-month follow up, over 50% of the patients from the intervention group managed to be at an adhered level, compared with the control group, and reached an important improvement prior to the intervention 21. In the DIAL study, after ending the follow up, patients were monitored for 1 and 3 years, finding that the hospitalization rate was lower in the intervention group. The benefit observed during the intervention period persisted and remained. This effect may be explained by the impact of the educational intervention upon behavior and the adaptation to changes of patients’ habits and lifestyles 22. Said result agrees with the findings in our study, which observed that six months after ending the follow up, over 72.4% of the patients from the intervention group achieved complete adherence through empowerment, motivation, security, and their active role in managing their disease. To keep patients adhered over time, it is fundamental to consider essential recommendations, like those stated by Latimmer and Curell, where the time established to make the telephone calls is subject to the patient’s condition and evolution. These calls are initially recommended at least every 15 days during the first two months and then every month 23,24. Additionally, the authors recommend for nursing professionals to enhance their communication skills and their knowledge on managing the disease, and highlight that monitoring cannot be carried out spontaneously and heterogeneously, given that it would no longer be an effective intervention due to the vast variability that would result. These recommendations were considered in our study, favoring the results reached.
An essential aspect that allows patients to be adherent over time is determined because they have positively valued the reinforcement of knowledge, peacefulness, and security generated by nursing professionals during telephone monitoring 25. Broadened knowledge of their disease, which patients developed during monitoring, recognition of decompensation signs, their timely management, and the relationship of trust with the professional permitted increasing their intrinsic motivation and, thus, achieve adherence.
The regression model showed the existence of an association of the intervention (telephone monitoring) and that maintenance of adherence behaviors depend on time, being stronger in patients who enter the follow up with levels of adherence within the 50th percentile. This result may be because these patients had endured their disease for much longer, had much lower ejection fractions, unlike patients in lower adherence percentiles, propitiating that their prior experiences of risk due to decompensations reached protection behaviors aimed at improving their self-care. This agrees with that described by Boisvert, which highlights that to achieve a high level of adherence and maintain such, patients must have perceived their severity and developed patterns of behavioral change 26.
Another aspect in our study that must be highlighted are the domains of the adherence instrument that achieved significant improvement, thus, managing for patients to completely adhere and over time these involved engaging in exercise, weight control, diet, and warning signs, a result that coincides with the study by Lupon et al.,27. The study elucidates an 80% rate of adherence in these same domains upon ending the tele-monitoring. Some studies have indicated that weight control and the warning signs are monitoring behaviors, and hydro-saline restriction a maintenance behavior that contributes to the stability of the clinical profile 28.
The dimension evaluating mood improved throughout the follow up, becoming an aspect that favors adherence. If adequate management of the disease exists, patients develop motivation, participation, and commitment in their daily lives, increasing self-esteem and interest, which permits confronting and coping with changes in their lifestyles 29.
Literature indicates that sociodemographic variables, like age, support network, occupation, and schooling can influence on the level of adherence. The regression model permitted identifying that the male gender, university schooling, and the caregiver have a positive association with adherence. Regarding gender, our findings contradict that described by some authors 30,18. It is attributed to male patients having improved their adherence because they were retired and had more time to concentrate on their care and self-monitoring. With respect to university schooling, it may be related to adherence to treatments, hence, it is expected that greater schooling facilitates understanding, appropriation, and compliance of these activities 31. Caregivers become the support to maintain health and help buffer the negative effects of the disease. Having a structured family, spouse or children is a factor that facilitates adherence between 40% and 60% 32. To end, the clinical evolution of patients with HF can improve substantially if simple low-cost tools are incorporated to their care, like structured telephone monitoring, which permits offering timely support in real time and generating a sustainable effect over time.
Limitations
Assignations should be concealed, given that the researchers knew previously about the intervention to which the subjects would be assigned
CONCLUSION
The results from this research suggest that structured telephone monitoring had a beneficial effect in achieving and maintaining adherence over time. It is necessary to monitor during 12 months to maintain the conducts over time. Variables, like gender (male), schooling (university), and caregiver, become factors that can favor adherence in patients with heart failure. Telephone monitoring during 12 months becomes a more effective intervention in patients who are in levels of adherence within the 50th percentile, and for patients with percentiles < 50 greater follow up time is required.
REFERENCIAS BIBLIOGRÁFICAS
1. Miró O. Evaluación de los conocimientos y la percepción de soporte a la enfermedad en los pacientes con insuficiencia cardiaca. Estudio SOPICA en España. Rev. clín. esp. 2016; 216(5): 237-247. [ Links ]
2. Tamayo D. Costos ambulatorios y hospitalarios de la falla cardiaca en dos hospitales de Bogotá. Acta méd. colomb. 2013; 38(4): 208-212. [ Links ]
3. Clark RA, Inglis SC, McAlister FA, Cleland JG, Stewart S. Telemonitoring or structured telephone support programmes for patients with chronic heart failure: systematic review and meta-analysis. BMJ. 201; 334(7600), 942. [ Links ]
4. Ramachandran K, Husain N, Maikhuri R, Seth S, Vij A, Kumar M, et al. Impact of a comprehensive telephone-based disease management programme on quality-of-life in patients with heart failure. The National Medical Journal of India. 2007;20(2):67-73. [ Links ]
5. Padilla M. Seguimiento telefónico a pacientes con insuficiencia cardiaca. Metas de Enferm. 2011; 14(3): 22-26 [ Links ]
6. Dunagan C, Littenberg B, Ewald GA, Jones CA, Emery VB, Waterman BM, et al. Randomised trial of a nurse-administered, telephone-based diseased management program for patients with heart failure. J. card. fail. 2005;11(5):358-65. [ Links ]
7. Grancelli H. Programas de tratamiento en la insuficiencia cardiaca. Experiencias del Estudio DIAL. Rev Esp Cardiol. 2007; 60(suppl 3): 15-22. [ Links ]
8. Larson-Dahn M. Telephone nursing practice model framework for role expansion across the continuum of care. JONA. 2000; 30(11): 519-523. [ Links ]
9. Achury D. Validez y confiabilidad de un instrumento evaluativo de adherencia en los pacientes con falla cardiaca. Enferm. glob. 2012; 11(2):1-7. [ Links ]
10. Pértegas Díaz S, Pita Fernández S. La distribución normal. Cad Aten Primaria. 2001; 8: 268-274. [ Links ]
11. Bottai M, Cai B, McKeown RE. Logistic quantile regression for bounded outcomes. Stat Med. 2010; 29(2): 309-17. [ Links ]
12. R Core Team (2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing. Retrieved from: https://www.R-project.org/ [ Links ]
13. Torsten H, Kurt H, Mark VW, Achim Z. Implementing a Class of Permutation Tests: The coin Package. Journal of Statistical Software. 2008; 28(8), 1-23. Retrieved from: http://www.jstatsoft.org/v28/i08/ [ Links ]
14. Geraci M. Linear Quantile Mixed Models: The lqmm Package for Laplace Quantile Regression. Journal of Statistical Software. 2014; 57(13), 1-29. Retrieved from: http://www.jstatsoft.org/v57/i13/.8 [ Links ]
15. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats A, et al. Guía ESC 2016 sobre el diagnóstico y tratamiento de la insuficiencia cardiaca aguda y crónica. Rev. esp. cardiol. 2016; 69(12), 1167-e1. [ Links ]
16. Comín J. Transiciones de cuidados entre insuficiencia cardiaca aguda y crónica: pasos críticos en el diseño de un modelo de atención multidisciplinaria para la prevención de la hospitalización recurrente. Rev. esp. cardiol. 2016; 69: 951-61. [ Links ]
17. Riegel B, Beverly C, Zoe K, LePetri B, Glaser D, Unger A. Effect of a standardized nurse case-management telephone intervention on resource use in patients with chronic heart failure. Archives of internal medicine. 2002; 162(6): 705-712. [ Links ]
18. Hernández-Pinzón C, Flórez-Flórez ML. Adherencia al tratamiento en la insuficiencia cardiaca y las tecnologías de la información y la comunicación. Rev. colomb. cardiol. 2016. [ Links ]
19. Domingo M. Telemonitorización no invasiva en pacientes ambulatorios con insuficiencia cardiaca: efecto en el número de hospitalizaciones, días de ingreso y calidad de vida. Estudio CARME (CAtalan Remote Management Evaluation). Rev. esp. cardiol. 2011; 64(4): 277-285. [ Links ]
20. Cañón Montañez W, Oróstegui Arenas M. Intervenciones educativas de enfermería en pacientes ambulatorios con falla cardiaca. Enferm. glob. 2013; 12(31): 52-67. [ Links ]
21. Ferrante D, Maccia A, et al. Long-term results after a telephone intervention in chronic heart failure: DIAL (Randomized Trial of Phone Intervention in Chronic Heart Failure) follow-up. J Am Coll Cardiol. 2010; 56(5): 372-378. [ Links ]
22. Juillière Y, Jourdain P, Suty-Selton C, Béard T, Berder V, Maître B, et al. Therapeutic patient education and all-cause mortality in patients with chronic heart failure: a propensity analysis. Int J Cardiol. 2013; 168. 388-395. [ Links ]
23. Lattimer V, Sassi F, George S, et al.: Cost analysis of nurse telephone consultation in out of hours primary care: evidence from a randomised controlled trial. BMJ. 2000; 320:1053-1057. [ Links ]
24. Currell R, Urquart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on profesional practice and health care outcomes (Cochrane review). London: The Cochrane Library; 2001. [ Links ]
25. Lange I, et al. Efecto de un modelo de apoyo telefónico en el auto-manejo y control metabólico de la Diabetes tipo 2, en un Centro de Atención Primaria, Santiago, Chile. Rev. méd. Chile [online]. 2010; 138(6): 729-737 [ Links ]
26. Boisvert S, et al. Revisão integrativa sobre intervenções de enfermagem voltadas para a promoção do auto-cuidado entre pacientes portadores de insuficiência Cardíaca. Revista Latino-Americana de Enfermagem. 2015; 23(4): 753-768. [ Links ]
27. Lupón J, et al. Implicación pronóstica de la fragilidad y los síntomas depresivos en una población ambulatoria con insuficiencia cardiaca. Rev. esp. cardiol. 2008; 61(8): 835-842. [ Links ]
28. Del Socorro Arredondo-Holguín E, De Los Ángeles Rodríguez-Gázquez M, Higuita-Urrego LM. Dificultades con la adherencia al tratamiento no farmacológico de pacientes con falla cardiaca detectados a través de seguimiento telefónico. Investig. enferm. 2014; 16(2): 133-147. [ Links ]
29. Bayés R. Aspectos psicológicos de la adherencia terapéutica. Revista de Cardiología. La Mancha: Ediciones de la Universidad de Castilla-La Mancha; 2000; 95-103. [ Links ]
30. Rojas Sánchez LZ, Echeverría Correa LE, Camargo Figuera FA. Adherencia al tratamiento farmacológico y no farmacológico en pacientes con falla cardiaca. Enferm. glob. 2014; 13(36): 1-19. [ Links ]
31. Zambrano R, et al. Percepción de la adherencia a tratamientos en pacientes con factores de riesgo cardiovascular. Rev. Fac. Nac. Salud Pública. 2012; 30(2): 163-174. [ Links ]
32. Pattenden JF, Roberts H, Lewin RJP. Living with heart failure: patient and carer perspectives. Eur. j. cardiovasc. nurs. 2007; 6(4): 273-279. [ Links ]
Received: March 06, 2017; Accepted: May 27, 2017











 texto en
texto en