Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.18 no.55 Murcia jul. 2019 Epub 21-Oct-2019
https://dx.doi.org/10.6018/eglobal.18.3.346711
Reviews
Depression as a risk factor for Alzheimer's disease: evidence and role of Nursing
1Nurse, Complejo Hospitalario Universitario de Santiago de Compostela, Servizo Galego de Saúde, Santiago de Compostela, Spain. rebecamontoiro6@gmail.com
2Hired predoctoral, Nurse, Department of Pedagogy and Didactics, Faculty of Education Sciences, University of Santiago de Compostela, Santiago de Compostela, Spain.
3PhD, Assistant Professor Doctor, Department of Psychiatry, Radiology, Public Health, Nursing and Medicine, School of Nursing, University of Santiago de Compostela, Santiago de Compostela, Spain.
Introduction
Depression and dementia are two diseases with a high prevalence worldwide and many features in common. Dementia is a progressive disorder being Alzheimer's Disease the most frequent type. On the other hand, depression represents the first worldwide cause of disability. The objective of this review is to analyze depression as a risk factor in the development of Alzheimer's Disease and to highlight the role of nurses regarding prevention in this field.
Methods
A bibliographic systematic search in diverse data bases was done. It is necessary to highlight PubMed as the main data base from which the majority of articles included were obtained.
Results and discussion
There are mainly three hypotheses about the relationship between depression and dementia: depression as a risk factor, depression as a prodrome or depression and dementia as two independent pathologies. Moreover, there are a lot of aspects that must be taken into account in each case adding more complexity to the investigations. At the neurobiological level there is also evidence of common pathological mechanisms for both diseases. In addition, prevention has to be emphasized as a key point in the treatment of these disorders and nurses play a crucial role in early diagnosis and health education.
Conclusions
Depression as a risk factor to Alzheimer's Disease has been demonstrated in many studies. However, there is not a conclusive agreement and, therefore, it is crucial to continue investigating the relation between depression and dementia.
Keywords: Nursing care; depression; Alzheimer Disease; risk factors; disease prevention; evidence-based nursing
INTRODUCTION
Dementia, especially Alzheimer's Disease (AD), and depression, are two of the most prevalent pathologies worldwide. Both of them are closely linked and affect, mainly, to the elderly. The relationship between this two diseases is complex and, in spite of all the studies made about the central topic of this bibliographic review, the number of hypotheses are still very numerous and there is not a clear conclusion. Firstly, it is necessary to highlight dementia as a chronic and progressive disorder characterised by damages on memory, intellectual skills, behaviour and the ability to carry out daily life activities. It represents one of the first causes of disability and dependence in the elderly who are the most affected by this pathology although dementia is not a normal consequence of the aging1.
In particular AD represents between the 60-70% of the dementia cases, in Spain there are around half a million persons that suffer from this pathology2. Its principally risk factor (RF) is the age, being 65 years old the main age of diagnosis. Other important RF are the genotype apolipoprotein E (APOE) e4, the use of no-steroidal anti-inflammatory drugs, diabetes mellitus, traumatic brain damage, family history of AD, different cardiovascular diseases, a low educational level or depression2,3.
Regarding to physiopathology, AD causes damage on neurons, reducing the number of synapses and, as consequence, the global cerebral activity. It happens due to protein accumulation inside the neurons, in form of β-amyloid plaques, and outside in form of neurofibrillary tangles formed by a specific type of protein called tau. In addition to the APOE-e4 genotype, before mentioned, it is important to highlight the genetic damage that takes place in AD as consequence of mutations in three different genes: amyloid precursor protein, presenilin 1 and presenilin 23.
On the clinic progression of AD we can stand out three different phases. During the first one the damage affects to the recent memory with symptoms as depressed mood, indifference, personality changes, among others. In the intermediate phase remote memory is also affected, starting to emerge difficulties to realise daily life activities. Finally, in the third phase, the patient is completely dependent2.
Depression is one of the most important RF for AD. It is a mental disorder with a high morbidity that affects more than 300 million people and that represents the first worldwide cause of disability. It is more frequent on women than men and, on its worst stage, can trigger on suicide. It is characterised by sadness, loss of interest or pleasure, guilty feelings or lack of self-esteem, sleep or appetite disorders, tiredness and lack of concentration4.
Depression is a multifactorial pathology and, as consequence, RF involved on its appearance can be very diverse. It can be personal-social, cognitive and/or family or genetic factors5. Regarding to biological factors, there are many studies that demonstrate a clear relation between depression and changes on the structure and functions of the brain. Structurally, it stands out the affectation on three different areas: hippocampus, amygdala and cerebral cortex. In particular it is noticed a reduction on the volume of the hippocampus that plays an important role on the development of depression6.
Among the neurobiological mechanisms that take part on the development of depression it is necessary to highlight: the dysfunction of the hypothalamic-pituitary-adrenal axis, the lack of monoamines (serotonin, norepinephrine and dopamine), changes at the neuronal plasticity and neuroinflammation7.
Having in mind all the exposed characteristics, the central issue of this bibliographic review is to explain the connection between this two disorders, depression and dementia, and to highlight the importance of knowing the mechanisms of that relation.
Nowadays for AD, despite all the efforts made to find an efficient treatment, it is not any that stop definitely the progression of the disorder. Because of this the prevention of the RF is one of the most important ways that nurses have to fight against this pathology and against all the consequences that it represents to the patients and their families.
Therefore, the principal objective of this review is to analyze depression as a risk factor in the development of AD, explaining the different hypothesis and analyzing the possible neurobiological relation between them. Likewise, to identify the nurse role in the prevention area for both diseases, AD and depression.
MATERIAL AND METHODOLOGY
This project consisted in a rigorous and reproducible systematic bibliographic review about the phenomenon of study. The Descriptors in Health Sciences (DeCS) and Medical Subject Headings (MeSH) were used as well as different keywords to search for studies related to the subject under review. This search has been done using different sources of information detailed below.
Search Engines
Google (http://www.google.com): firstly it was used to read general information with the objective of getting a global vision of the topic and, afterwards, for searching concepts and manuals.
Scholar Google (https://scholar.google.es/): different searches were done using these keywords"Depression; Risk factor; Alzheimer's disease; Dementia" [MeSH].
Databases
-
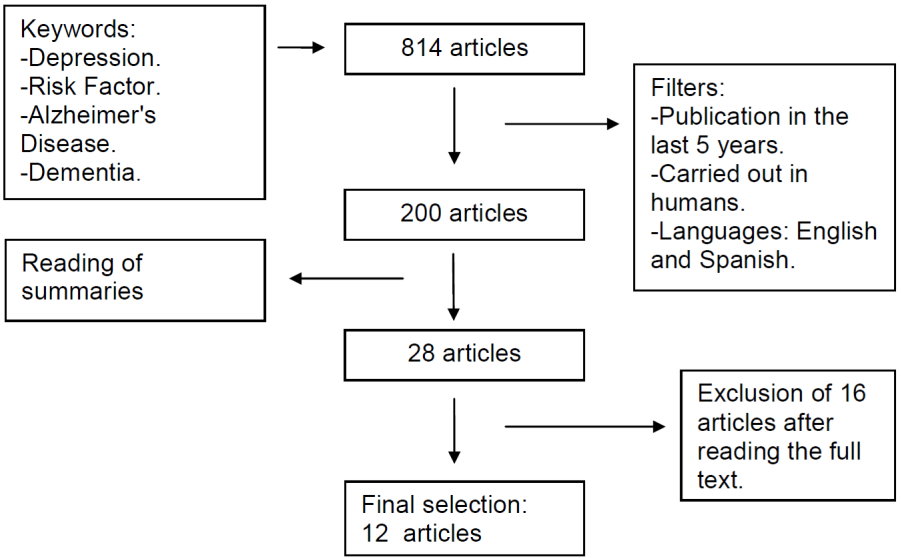
Pubmed (https://www.ncbi.nlm.nih.gov/pubmed/ ): different searches were done using the next keywords:Alzheimer's Disease; Depression; Risk Factor; Dementia [MeSH]. The final results and the method employed is specifically detailed in figure 1.
Dialnet (https://dialnet.unirioja.es/): the following keywords combination was used: "Depresión AND Enfermedad de Alzheimer" [DeCS] and it was obtained a total of 107 articles. After the use of the next filters: full text, Dialnet subject: health science and date of publication: 2012-2017, the number of articles drop until 26. Finally, 1 article was included in the review.
Cinahl(https://www.ebscohost.com/nursing/products/cinahl-databases/cinahl-complete): using the next keywords combination: "DepressionANDRisk factorANDAlzheimer's disease" [MeSH] it was obtained a total of 300 articles. Next, the following filters were applied: date of publication 2012-2017 and full text, reducing the results to a total of 19 articles.
Specialized web pages
Specialized web pages were used to search concepts, classifications and epidemiological data. It stands out:
Fisterra: https://www.fisterra.com/
World Health Organization (WHO): http://www.who.int/es/
With the aim of reducing the results in order to adapt perfectly the search to the objectives of this review, the following inclusion-exclusion criteria were used:
- Inclusion criteria: all articles in English or Spanish were taken into account. Because of all the technological and health advantages that are continually made, the search was limited to the last five years. This temporal limitation was not considered in some exceptional cases because of the relevance of some articles to the matter. Moreover, the aim was to filter the articles in order to obtain a varied, non-repetitive and complete final selection that provide a detailed view of the subject and that allow to point out controversies. Also, other articles and documents were taken from the bibliography of the selected ones.
- Exclusion criteria: all the articles published in a different language from English or Spanish, those which do not focus on the main topic of this review or without relevant information were dismissed.
Despite of realising a meticulous search on all the cited sources of information, the principal database that sustained this review was Pubmed because of the high quality and utility of its studies.
RESULTS AND DISCUSSION
Most part of the selected studies examine dementia and AD jointly, because of that the term "dementia" will be used, especially in the title of the sections, but in principal reference to AD, specifying when it has been reflected in the study.
Relationship between depression and dementia:
The AD is related to several RF that can be classified in modifiable (low educational level, depression, vascular RF and physical inactivity) and not modifiable (age, ethnic group, genetic factors)8,9,10.
Depression is included in the group of the modifiable RF in reference to numerous studies that demonstrated it. With all, as mentioned before, because of the current debate about the role of depression on the development of AD and other dementia types, we have to differentiate three different hypothesis11,12:
1. Depression: risk factor for dementia:
First of all, it is necessary to clarify the concept of RF, that is any circumstance that increase the probability of develop a pathology13. Therefore, when it is mentioned depression as RF, it means that suffering from depression increases the probability of suffering, afterwards, AD or other type of dementia.
Memory problems are one of the most common symptoms on depressed people, being present in 40% of the cases14; those memory problems are objective confirmed by the realization of cognitive tests. Additionally, it is also proved that depression accelerates the cognitive deterioration when it occurs in patients that suffered, previously, from dementia11.
In spite of all the explained before, in practice, the similarity between the symptoms of both pathologies makes the differential diagnosis very difficult. Therefore, when depression is analyzed as a RF, it is necessary to bear in mind several aspects that have influence in that relationship:
A. The nature of the depressive disorder:
It is necessary to differentiate, principally, between chronic depression or isolated depressive attacks; and between a first depressive attack or a recurring depression.
Several studies have proved that people with chronic depression show higher risk of developing any type of dementia (in particular AD) than those with only one isolated attack during their lives11,15. In addition, the severity of the disorder has also a proportional influence, the higher it is the higher would be the risk14.
Specifically, a longitudinal study realised in Zaragoza in 2015 analyzed the relationship between AD and severe depression, persistent depression, first depressive attack and not treated depression. The results of that investigation proved an increase on the risk of developing AD in those individuals with severe depression or not treated depression. It was also found an increase on the risk,
even not as clear, in individuals with a first depressive attack, however it was not found association between persistent depression and AD9.
B. Symptomatology of depressive disorder:
In relation to the previous point it is the symptomatology, changing the relation between depression and dementia according to the pattern of depressive symptoms.
A prospective cohort study done in different cities of the United States between 2014 and 2015 concluded that high and raised symptoms of depression meant an independent RF for dementia, while moderate and raised symptoms were consequence of a dementia disorder already in progress16.
The studies focussed on the two previous sections stand out the importance of knowing the characteristics of the depressive disorder and the progression of its symptoms. However, this is the weak point of many studies that use, as diagnostic method for depression, uniform scales without making a difference between chronic depression, first attack, severity of the disorder, etc. In addition, these studies make the diagnosis in just one point of the study period without having in mind the changes that take place over time. The consequence of these is a greater variety on the results and less validity12,13.
C-Onset / development moment of depression:
Several studies highlight the onset / development moment of the depressive disorder as a crucial point on the determination, or not, of depression as a RF. Based on this, it is necessary to make a difference between early depression (if it takes place before the old age) or late depression (if it takes place, for the first time, after 50-60 years old). Many studies conclude that early depression is a RF for dementia, while late depression, that takes place closer to the diagnosis of dementia, could be a prodrome of it11.
Nevertheless, there is not consensus in this point. A study carried out with the objective of evaluating the relation between dementia and various modifiable RF, stood out depression as a RF on the development of all types of dementia and, in particular, late depression as a RF to AD8. In agreement with the previous one, Diniz and Cols. (2013)15, concluded that late depression is related with a higher risk of developing AD and vascular dementia. In contrast, Burke and Cols. (2016)17, found risk association regardless of the moment of development of depression.
2. Depression: prodrome of dementia:
In the same way as in the case of the concept of RF, it is important to clarify the definition of prodrome in order to analyze depression as one. A prodrome is an early manifestation of a pathological process, it means, a symptom that precede the onset of the pathology13.
The temporal aspect, explained in the previous section, is the base of the studies that affirm that depression is not an independent RF, if not a prodrome of dementia.
Several studies affirm that depression as a prodrome is the result of the self-assessment of the individual that, conscious of his own loose of cognitive functions, develop, as an answer, a depressive disorder. The difficulty in this point is that the prodrome period of dementia is not well delimited and could spread throughout ten, or more, years before the diagnosis11,16. As a consequence, it is very difficult to differentiate which depressive symptoms are in that prodome period and could be a result of a dementia disorder in progress and which not.
In a cohort study, realised by Singh-Manoux and Cols. (2017)12, about the progression of the depressive symptoms previous to the diagnosis of dementia, it was done a retrospective analysis of the results throughout 28 years. Those results did not support the hypothesis of depression as a RF, concluding that depression is a consequence of the preclinical phase of dementia. This happens because it was only found relation between dementia and depression, regardless of the depressive characteristics (chronic, recurrent etc.), when the symptoms appeared in the previous decade of the dementia diagnosis.
In agreement with the results of the previous study, another investigation, focussed on AD, concluded that if depression is a prodrome of AD it has to be temporal proximity between the onset of depression and the onset of dementia instead of depressive symptoms that remit and reappear later. Based on this, late depression has to be a prodrome of AD13.
Therefore, to establish depression as a consequence of the dementia development and not as a RF, it is necessary to have in mind that the disorder could not be detected at its beginning. It means, to accept that the temporally proximity between the onset of both pathologies define the relationship between them do not have to be correct if the diagnosis is done late13.
In relationship with the previous, Ownby and Cols. (2006)18 set out as one of their objectives to study the importance of the temporally period between the diagnosis of both pathologies. Their hypothesis established that if the association was negative, it means, the smaller the temporal period between diagnosis of both disorders was, the biggest would be the risk of AD, then depression would be a prodrome. In contrast, if the relationship was positive and, therefore, the bigger the temporal period between them was, the bigger would be the risk, so depression would be an independent risk factor to AD. After the realisation of their investigation, they concluded that the relation was positive and, therefore, depression would be an independent RF to AD.
3. Depression and dementia independent pathologies:
The third hypothesis is based on the fact that depression and dementia are two pathologies of the old age and, therefore, simultaneous.
To this is necessary to add that these pathologies have common risk factors and symptomatology. Some of these common symptoms are memory problems and sleep disturbances; while among the common risk factors stood out the low economic level, social isolation and vascular RF, among others.
On the other hand, both pathologies also share neurobiological characteristics: inflammation, neurodegeneration, variations in the hypothalamic-pituitary-adrenal axis, etc.11,12. Those common characteristics could cause errors on the diagnosis. Because of that, a depressive person could be mistakenly diagnosed from dementia or, on the contrary, it could be associated the symptoms to a depressive disorder being, in fact, a dementia process13.
Despite the previous, it does not exist enough evidences that support this third hypothesis. Several studies that had had in mind, in the moment of analyzing the results, the common RF for both pathologies, still concluding that depression is an independent RF11.
Neurobiological explanation:
All the explained before has a neurobiological basis. The development of both pathologies, depression and AD, is related with some genetic aspects and pathological processes that provide consistency to the hypothesis that relates them.
Genetic aspects:
First of all, it is necessary to mention the genetic role in the appearance of both disorders, especially in AD as in its development is crucial the genetic transmission17.
The way in which individuals answer to the ambient factors would depend, partially, of their genetic information. Like this, the existence or not of different genotypes could determine a higher risk of development a pathology. In the case of AD a gene implicated on its development is APOE17. It is, therefore, a not modifiable RF, but it is important to bear in mind the risk that mean its presence in combination with other modifiable RF as depression.
There are three variants of the genotype APOE: e2, e3, e4. The presence of e2 is considered neuroprotector and, even, has been pointed out that could delay the onset of AD. However it is demonstrated that e3 and, above all, e4 increase the risk of its development17. In addition, it is estimated that 40-65% of the people who suffer from AD have one or two copies of the genotype APOE-e43.
A study carried out with the aim of determining the association between depression, sleep disturbances, APOE and dementia, concluded that even there was not found a direct relation between depression and the genotype APOE, the risk of developing AD is higher in people who have the genotype APOE-e4 and depression jointly than in those who only have one of the variables17.
The importance of this is that, despite there are some RF not modifiable, like the genotype APOE, it is possible to act against other modifiable that increase the effect of the not modifiable, like depression.
Neuropathology mechanisms:
Several investigations connect depression and dementia by different pathological mechanisms at the neurological level. The principal ones are explained in table 1.
Table 1. Pathological mechanisms implicated in depression and dementia.
| PATHOLOGICAL MECHANISM | SCIENTIFIC EVIDENCES |
| Accumulation of β-amyloid plaques and tau protein in form of neurofibrillary tangles. | Several studies have proved that the accumulation is higher in patients with AD and depression than in those with AD and without depression. This accumulation causes neuronal death reducing the number of nervous synapses. |
| Reduction of nerve growth factors. | Both in AD and depression it is proved that take place a reduction in the number of nerve growth factors. Among them it is necessary to highlight the BDNF (brain-derived neurotrophic factor). |
| Hyperactivity of the hypothalamic-pituitary-adrenal axis. | During depression it takes place an overstimulation of the hypothalamic-pituitary-adrenal axis that, in answer to the stress, increases the liberation of glucocorticoids (cortisol). This causes atrophy in the hippocampus that is related with loss of neurons, having harmful effects on memory and could cause the onset of dementia. |
| Increase of vascular disorders | The proper cerebral functioning depends, directly, on the vascular system. Vascular alterations, related in many occasions with depressive processes and habits (smoking, inactivity etc.), cause variations on the brain that contribute to the development of AD. |
| Neuroinflammation | During depression it takes place, principally by the activation of the microglia, an increase in the release of proinflammatory cytokines. This increase causes brain damage and leads to the development of AD. |
Own elaboration using the reference bibliography11,14,19,20.
Alzheimer's Disease (AD).
These pathological processes are not mutually exclusive, that is, they are connected and usually happen simultaneously. Because of this, the investigation at neurobiological level is really diverse and varied, taking place, again, controversies11.
Particularly, a study realised by Wilson and Cols. (2016)21, with the aim of determining if depression is related with the dementia pathological processes, concluded negatively. They studied the possible relation between depression and six dementia pathological marks: neurofibrillary tangles of protein tau, β-amyloid plaques, Lewy bodies, sclerosis of the hippocampus and microscopic infarcts. However, after the investigation, they only found relation between depression and the formation of β-amyloid plaques21.
In contrast, another investigation, which principal objective was to study the relation between synapsis degeneration, depression and AD, found a positive association and also stood out other common processes between the disorders such as neuroinflammation7.
Prevention and nurse role:
As it was mentioned before, with a pathology as Alzheimer’s Disease the prevention of its RF is crucial.
There are many studies that try to emphasize on this point. In particularly, one published on the Lancet Neurology journal and realised with the objective of reflecting the importance of prevention in AD, concluded that one third of AD cases can be attributed to modifiable RF. Throughout the mentioned investigation, it was calculated the attributable risk (proportion of AD cases attributable to a RF) of seven modifiable RF which association with the disease is scientific proved: diabetes, hypertension, obesity, physical inactivity, depression, smoking and low educational level. The results determined that a decrease, per decade, of the 10% in the prevalence of each RF, would reduce in a 8.3% the worldwide prevalence of AD estimated to the year 2050, which is estimated around 106.2 million cases. While a reduction in the 20% would reduce the AD prevalence in a 15.3%10. See figure 2.
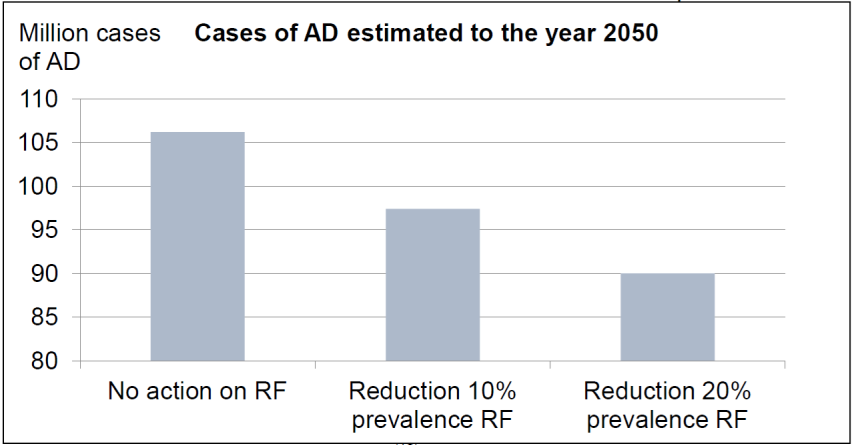
Figure 2. Number of cases of AD estimated to the year 2050 if there is no action on RF versus if there is a reduction in a 10% or in a 20% on the prevalence of those RF.
Modified from Norton and Cols. (2014)10. Alzheimer’s Disease (AD) Risk Factor (RF).
Despite the strength of the investigation results, at the moment of assessing them, it is necessary to have in mind certain limitations of the study. On one hand, the relation between AD and the studied RF could be altered by some unknown or not evaluated RF. And, on the other hand, the calculations were done in specific moments, without analyzing the variation that could happen throughout time and through the different generations. For example, the changes that could be carried out in the following years to improve the educational level would affect people younger than those who are really going to be in risk of developing AD in 2050, which is the year taken as a reference to calculate the results10.
Specifically, depression, RF of higher interest in this review, is defined as a pathology that could be prevented and, therefore, its early treatment could delay, at the same time, the development of dementia15. One point in which the investigations that study prevention agree is the importance of the role played by the health staff and, in particularly, the role of nurses17,19.
In particularly, a study published in the Journal of Nursing Scholarship journal, (one of the journal edited by the Sigma Theta Tau International Honor Society of Nursing -Sigma- which is the second biggest nurse organization worldwide) about depression as a RF for different pathologies, among them AD, stood out the nurse function in the preventive area. It pointed out that, in the first place, it is necessary to know the nature and the principal signs and symptoms of depression to be able to detect it early or even be able to anticipate its development by adopting the most optimal preventive measures. In the same way, it is necessary to know the relation between depression and other pathologies, in this case AD, and its possible role as RF to be able to act directly on the depressive disorder and, at the same time, indirectly preventing the development of other pathology. For this it is crucial a good nurse-patient relationship19.
Another basic aspect on the preventive level is the health education17. An optimal educational level, the practice of physical activity, and good social relationships increase the cognitive reserves of the individuals14. In this point, primary attention is so important and nurses must assume their responsibility on the education of patients. This responsibility does not only consist on giving patients information about the adverse effects of theirs bad acts, but also on trying to help them to, gradually, change those bad habits for healthier ones that remain throughout time15.
Bearing in mind the nurse work, that does not only consist on take care of the person affected by the disease, but also of the family, we have to know the current characteristics of the caregivers and family; adapting our job to the emerge needs. Health education and prevention, therefore, has to focus not only in the patient but on the community where he/she lives. Relatives are, in many cases, the informal caregivers at home, which is a field that is gaining higher importance in the last years. The principal caregiver is represented, in most part of the cases, by a female figure, motivated by the gender role and its implications at home. In relation with this, the role of nurses gains, if it is possible, a higher importance on the context of the current care scene; it is still an activity that involves the binomial caregiver/patient and that is prolonged throughout time, being necessary to get used to it22,23,24.
In conclusion, the strategies of prevention, early diagnosis and correct treatment of depression have a great importance to fight against AD. But also, they have a great general effect on the health system, because depression is a RF to many pathologies15. Because of this, being this another point in which most part of the examined studies are agree, it is very important to continue with the investigations about depression as a RF to AD in order to be able to also determinate the impact of the work on the preventive area8,15-17.
Limitations and considerations:
- Continuous reference to dementia in general, despite being AD the main objective of this review, due to the shortage of studies focus exclusively on AD.
- This review has been based principally in observational studies and bibliographic reviews due to the small number of clinical trials about the topic. In addition, the lack of studies realised at national level made it difficult to include investigations developed, particularly, in Spain.
CONCLUSIONS
After an exhaustive analyze of the different studies included in this review the following conclusions were drawn:
It was found support, among the science community, to establish depression as a RF for the development of AD.
There are, nowadays, three hypothesis that try to explain the role of depression on the development of dementia: (a) depression as a RF for the development of dementia, (b) as a prodrome for dementia, and (c) depression and dementia two independent pathologies but coincident in their development.
Nowadays, the hypothesis that establishes depression as a RF is the most accepted one, but the one that establishes depression as a prodrome has also a lot of support so, both of them have to be analyzed in future investigations.
Depression is closely related, not only with AD but, with dementia in general.
At the neurobiological level exists coincidence in the pathological processes that take place in both disorders being, moreover, a crucial point to explain the relation between them.
Prevention and early diagnosis are two of the most important points in the treatment of this two priority diseases to the public health. The work of the nursing staff, who have a huge responsibility in this area, must be focus in the patient but also in the families. In this way, they must provide quality care based on the biggest possible evidence both to the person who is affected by the disease and to his main care caregiver, that in most part of the cases is a woman.
Depression and AD are two pathologies with many features in common and the nature of their relation is submitted to multiple controversies and scientific gaps. As a result, it is crucial to continue investigating with the objective of achieve a final conclusion and to be able to establish preventive and therapeutic measures in order to reduce the morbidity and mortality associated to both disorders.
REFERENCIAS
1. Organización Mundial de la Salud (OMS) [Internet]. Demencia [Actualizado 12 Dic 2017; consultado 16 Dic 2017]. Disponible en: http://www.who.int/es/news-room/factsheets/detail/dementia [ Links ]
2. Fisterra [Internet].Demencia tipo Alzheimer [Actualizada 5 Feb 2013; consultado 11 Dic 2017]. Disponible en: https://www.fisterra.com/guias-clinicas/demencia-tipo-alzheimer/ [ Links ]
3. Alzheimer's Association. 2015 Alzheimer's Disease Facts and Figures. Alzheimer's & Dementia [Internet]. 2015; 11 (3): 332. Disponible en: https://www.alz.org/facts/downloads/facts_figures_2015.pdf [ Links ]
4. Organización Mundial de la Salud (OMS) [Internet]. Depresión [Actualizado 22 Mar 2018; consultado 16 Dic 2017]. Disponible en: http://www.who.int/es/news-room/factsheets/detail/depression [ Links ]
5. Fisterra [Internet]. Depresión mayor en el adulto: factores de riesgo y diagnóstico [Actualizado 4 Agosto 2014; consultado 11 Dic 2017]. Disponible en: https://www.fisterra.com/guias-clinicas/depresion-adulto/ [ Links ]
6. Díaz Villa BA, González González C. Actualidades en neurobiología de la depresión. Rev Latinoam Psiquiatría. 2012; 11 (3): 106-15. Disponible en:http://www.medigraphic.com/pdfs/psiquiatria/rp-2012/rp123i.pdf [ Links ]
7. Wuwongse S, Cheng SS, Wong GT, Hung CH, Zhang NQ, Ho YS, et al. Effects of corticosterone and amyloid-beta on proteins essential for synaptic function: implications for depression and Alzheimer's disease. Biochim Biophys Acta. 2013; 1832 (12): 2245-56. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/23928361 [ Links ]
8. Bellou V, Belbasis L, Tzoulaki I, Middlenton LT, Ioannidis JPA, Evangelou E. Systematic evaluation of the associations between environmental risk factors and dementia: An umbrella review of systematic reviews and meta-analyses. Alheimers Dement. 2017; 13 (4): 406-18. Disponible en:https://www.ncbi.nlm.nih.gov/pubmed/27599208 [ Links ]
9. Gracia-García P, de-la-Cámara C, Santabárbara J, Lopez-Anton R, Quintanilla MA, Ventura T, et al. Depression and incident Alzheimer disease: the impact of disease severity. Am J Geriatr Psychiatry. 2015; 23 (2): 119-29. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/23791538 [ Links ]
10. Norton S,Matthews FE, Barnes DE, Yaffe K, Brayne C. Potencial for primary prevention of Alzheimer's disease: an analysis of population-based data. Lancet Neurol. 2014; 13 (8): 788-94. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/25030513 [ Links ]
11. Bennett S, Thomas AJ. Depression and dementia: cause, consequence or coincidence?. Maturitas. 2014; 79 (2): 184-90. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/24931304 [ Links ]
12. Singh-Manoux A, Dugravot A, Fournier A, Abell J, Ebmeier K, Kivimäki M, et al. Trajectories of Depressive Symptoms Before Diagnosis of Dementia: A 28- Year Follow- up Study. JAMA Psychiatry. 2017; 74 (7): 712-8. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/28514478 [ Links ]
13. Heser K, Tebarth F, Wiese B, Eisele M, Bickel H, Köhler M, et al. Age of major depression onset, depressive symptoms, and risk for subsequent dementia: results of the German study on Ageing, Cognition, and Dementia in Primary Care Patients (AgeCoDe). Psychol Med. 2013; 43 (8): 1597-610. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/23137390 [ Links ]
14. Deví Bastida J, Puig Pomés N, Jofre Font S, Fetscher Eickhoff A. La depresión: un predictor de demencia. Revista española de geriatría y gerontología: Órgano oficial de la Sociedad Española de Geriatría y Gerontología. 2016; 51 (2): 112-8. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=5661369 [ Links ]
15. Diniz BS, Butters MA, Albert SM, Dew MA, Reynolds CF. Late-life depression and risk of vascular dementia and Alzzheimer's disease: systematic review and meta-analysis of communitybased cohort studies. Br J Psychiatry. 2013; 202 (5): 329-35. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/23637108 [ Links ]
16. Kaup AR, Byers AL, Falvey C, Simonsick EM, Satterfield S, Ayonayon HN, et al. Trajectories of Depressive Symptoms in Older Adults and Risk of Dementia. JAMA psychiatry . 2016; 73 (5): 525-31. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/26982217 [ Links ]
17. Burke SL, Maramaldi P, Cadet T, Kukull W. Associations between depression, sleep disturbance, and apolipoprotein E in the development of Alzheimer's disease: dementia. Int Psychogeriatr. 2016; 28 (9): 1409-24. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/27020605 [ Links ]
18. Ownby RL, Crocco E, Acevedo A, John V, Loewenstein D. Depression and risk for Alzheimer disease: systematic review, meta-analysis, and metaregression analysis. Arch Gen Psychiatry. 2006; 63 (5): 530-8. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/16651510 [ Links ]
19. Bica T, Castelló R, Toussaint LL, Montesó-Curto P. Depression as a Risk Factor of Organic Diseases: An International Integrative Review. J Nurs Scholarsh. 2017; 49 (4): 389-99. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/28692781 [ Links ]
20. Byers AL, Yaffe K. Depression and risk of developing dementia. Nat Rev Neurol. 2011; 7 (6): 323-31. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/21537355 [ Links ]
21. Wilson RS, Boyle PA, Capuano AW, Shah RC, Hoganson GM, Nag S, et al. Late-life depression is not associated with dementia-related pathology. Neuropsychology. 2016; 30 (2): 135-42. Disponible en: https://www.ncbi.nlm.nih.gov/pubmed/26237627 [ Links ]
22. Jimenez Ruiz I, Moya Nicolás M. La cuidadora familiar: sentimiento de obligación naturalizado de la mujer a la hora de cuidar. Enfermería Global. 2018; 49: 420-33. Disponible en: http://scielo.isciii.es/pdf/eg/v17n49/1695-6141-eg-17-49-00420.pdf [ Links ]
23. Eterovic Diaz C, Mendoza Parra S, Saez Carrillo, K. Habilidad de cuidado y nivel de sobrecarga en cuidadoras/es informales de personas dependientes. Enfermería Global. 2015; 38: 235-48. Disponible en: http://revistas.um.es/eglobal/article/view/198121/174111 [ Links ]
24. Cantillo M, Lleopart T, Ezquerra S. El cuidado informal en tiempos de crisis. Análisis desde la perspectiva enfermera. Enfermería Global. 2018; 50: 515-28. Disponible en: http://revistas.um.es/eglobal/article/view/297211/226661 [ Links ]
Received: October 19, 2018; Accepted: January 21, 2019











 texto en
texto en