Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.19 no.57 Murcia ene. 2020 Epub 16-Mar-2020
https://dx.doi.org/eglobal.19.1.368611
Originals
Prevalence and factors associated with urinary incontinence in the east area of health of Valladolid
1Physiotherapist. Rehabilitation Service. Universitary Clinical Hospital. East Health Area in Valladolid. Spain. crismartu@gmail.com
2Principal Midwife of Primary Care Team. Gamazo Health Center. East Health Area in Valladolid. Spain.
Introduction
Urinary incontinence (UI) is the involuntary loss of urine that is a major social or hygienic problem and is objectively provable. It is a common symptom that appears in many diseases, affecting all age groups and both sexes. In Spain it is estimated a prevalence of 24% in women and 7% in men, increasing with age up to 50% and 29% respectively. Despite its impact on quality of life, it is under-diagnosed for various reasons.
Material and method
In this retrospective longitudinal epidemiological study data were collected from the medical histories of patients with UI belonging to the Pelvic Floor Unit of the East Health Area in Valladolid.
Results
The most frequent types of incontinence were: effort (43,13%) and mixed (39,21%). The most important risk factors and associated diseases were episiotomy (57.1%) and cystocele (32.6%) in women and adenocarcinoma of prostate (60%) in men. Responses in the questionnaires of urinary incontinence (ICIQ-SF) improved after 2-3 months of rehabilitation treatment.
Conclusions
The collected data are consistent with studies reviewed, and seeing the progress in prevention and treatment of UI, multidisciplinary approach is coherent.
Key words: Prevalence; Urinary incontinence; Prevention; Treatment
INTRODUCTION
Urinary incontinence (UI) is the involuntary loss of urine that is a major social or hygienic problem and is objectively provable.
The UI is a common symptom that appears in many diseases, affecting all ages and sexes, and in elderly groups it is considered one of the geriatric syndromes 1. Global prevalence of UI in women is around stimated 24% in Spain, increasing to 30-40% in middle age, and up to 50% in geriatric age. The prevalence of UI in male is around 7%, reaching 14-29% in men over 65 years, and up to 50% in people over 85 years and institutionalized 2.
In short, around 15.8% of the Spanish population could present UI, affecting 6.510.000 people approximately. UI has a major negative impact on the quality of life, from the social environment, to the physical, sexual, psychological, employment and domestic environments 3)(4. In addition, UI involves a high cost for health, at least 2% of the health budget in developed countries 5)(6. About 90% of this budget is due to accessories (absorbent diapers, probes, and so on), about 2% diagnosis and treatment and 8% to hospital stays and basic care 7. (Table 1)
Table 1. Impact of incontinence.
| Esfera | Repercusiones |
|---|---|
| Physical | Irritation and skin infections Pressure ulcers Urinary tract infections It predisposes to the falls |
| Psychic | Depression Anxiety Sleep disorders Loss of self-esteem Negative feelings: hopelessness, loneliness, shame, fear of smelling bad, and so on.. |
| Social | Social activity restriction Alteration of marital relationship Intercourse disorder Insulation Increased need for family support Increased need for social health resources Predisposes to institutionalization |
| Economic | Global UI cost: 2% health budget Absorbents: more than 3% of the pharmaceutical expenditure of the National Health System Burden on the personal and family economy |
| Daily life | Restriction of activities of daily life Limitation of physical activity Change of clothing type (darker) Giving up recreational and leisure activities Being aware of the bathroom location Having to go to the service frequently Frequent change of underwear Feeling wet |
UI, despite being a very common condition, is underdiagnosed for various reasons, sometimes by the patient himself (stigmatization)8, the search for help to solve her problem ranges from 9-69% among incontinent women, commonly with a long delay; others because of the low awareness of health professionals towards this disease, which is not serious, but which limits significantly the lives of those who present it 8)(9.
The risk factors associated with incontinence are numerous, as summarized in Table 2.
Table 2. Risk factors associated with urinary incontinence.
| Pregnancy/Vaginal labour/Episiotomy Estrogen depletion Pelvic muscle weakness High-impact physical activity Morbid obesity Stroke Cognitive impairment Low fluid intake | Drugs Diabetes Night enuresis in childhood Race Faecal impaction Immobility/Degenerative chronic disease Dellirium Environmental barriers |
Pelvic floor lesions related to vaginal labour in adult women stand out as the most important. As age increases, estrogenic deficit, chronic diseases (diabetes and degenerative diseases of the locomotor system) and neurological problems take on greater prominence. In elderly women the aetiology of UI is often multifactorial, as a result of the interrelationship of multiple processes.
Factors such as drugs, environmental restrictions, delirium, urinary tract infections, polyuria, faecal impaction... can produce acute transitory urinary incontinence, in which there is usually no structural lesions of the lower urinary tract and continence is recovered once the responsible factor is corrected. However, transient reversible factors of UI can also contribute to established, chronic, or persistent forms of UI. The temporal limit around four weeks distinguishes between transient or acute and persistent or established incontinence.
The established UI is not related to an acute disease or process and persists over time. Clinically it is classified into several types: Stress UI (SUI), Urgency UI (UUI), Mixed (MUI), and Emptying Dysfunction.
Causes of persistent or established incontinence may be urological (cistocele), gynecological and obstetric (labour, menopause, pre- and post-surgery, prolapses, painful scars), proctological (terminal constipation, rectocele), neurological, psychological, environmental, pharmacological, functional, so a multidisciplinary approach is needed for proper assessment and treatment 10)(11.
As the prevalence of UI is very high and in many cases is underdiagnosed, for detecting UI the opportunistic screening are recommended at least once in asymptomatic women over 40 years of age and in asymptomatic males over 55 years of age, by health workers of Primary Health Care (PHC). If there are UI risk factors, it will be performed annually, in both asymptomatic males and women, from the ages referred to above. Screening will consist of asking about 3 questions:
The occasional presence of unintentional loss of urine.
In the event of unintentional losses, if they are frequent and abundant.
If the leaks or losses represent any problem at this time in her life.
If the answers to these 3 questions are affirmative a diagnostic evaluation must be performed to know the type of incontinence and its impact on the quality of life 9)(10)(11)(12)(13)(14
The pathology of the pelvic floor can be evaluated through clinical diagnosis, based on the clinical history of the patient. However other researchers argue that this diagnosis can vary depending on the doctor who evaluates the patient. Likewise, it should take into account that patients are reluctant to ask the clinician about a delicate issue such as urinary or anal incontinence. Therefore, a more valid way of measuring the presence and severity of pathology of pelvic floor would consist of the use of an instrument in the form of self-tested, simple to use and formally validated questionnaire 15)(16. Lukacz et al, developed and validated the questionnaire "Epidemiology of Prolapse and Incontinence Questionnaire-EPIQ" in the United States17.
The Spanish version is semantically equivalent to the original in English. The EPIQ questionnaire, in the context of women with pathology of the pelvic floor, is not a diagnostic tool, but a tool that allows a global screening of all diseases of the pelvic floor as a whole. Expected aims are to make the doctor aware of PHC and help him/her in the diagnostic evaluation, classification and treatment of the UI, and define what the criteria for referral are and improve the flow of the patient in a surveillance shared between PHC and Urology.
The Spanish version of the EPIQ questionnaire shows suiTable feasibility, validity, and reliability to be used in clinical practice as a tool for screening of the pathology of pelvic floor 16)(17)(18.
Once different diseases are detected, the diagnostic confirmation should be carried out, either by clinical diagnosis or by complementary tests. In clinical practice if the aim is only to know if there is a specific problem or not, the EPIQ may be enough. Researching results, specific questionnaires of each pathology should complete, to evaluate not only the existence or not of the problem, but they can be used as scales to analyze the results of the applied treatments 16,17.
Although there are questionnaires of symptoms and quality of life for patients with UI, as the King´s Health questionnaire 19, properly validated in our country, their usefulness as instruments for the detection of the UI in general clinical practice is limited due to its extension and the required time for its completion; nevertheless, they are very useful in research.
According to the type of UI diagnosed, the different treatments are established: conservative (exercises of Kegel, perineometer, vaginal cones, absorbents, bladder catheterization); pharmacological (urinary continence facilitators: anticholinergic, alpha-adrenergic, muscle relaxant, spasmolytic drugs, hormone replacement therapy (HRT) or facilitators of urination: cholinergic beta-blockers and alfa-bloqueantes) and/or surgical treatment (transvaginal TVT mesh) 20.
The objectives of this study are:
MATERIAL AND METHOD
Retrospective observational epidemiological study of local sphere, in which the registered data in Gynecology and Urology services were consulted, and in the Unit of Pelvic Floor in the University Clinical Hospital in Valladolid (UCHV), during the period 1st of January of 2014 to 30th of June of 2015 (time that Unit of Pelvic Floor has been in operation)). Data of admitted patients in UCHV were selected, with a secondary diagnosis of UI, requiring surgical intervention by their main pathology. Likewise data from the subjects in the Pelvic Floor Unit was obtained in order to perform conservative treatments to improve their diagnosed UI symptoms.
The data was collected from the Encoding Unit and Rehabilitation Service of the UCHV, through access to the clinical history of the registered patients, respecting Data Protection Act of a Personal nature (Organic Law 15/1999, of 13 of December) and Law 41/2002, of 14 November, basic, regulator of the autonomy of the patient and rights and obligations in terms of information and clinical documentation. Also the approval of the Ethics Committee of the UCHV was obtained.
The following variables have been considered to exhibit their frequency distribution: age; sex; risk factors (triggers, contributors and partners), and type of treatment.
RESULTS
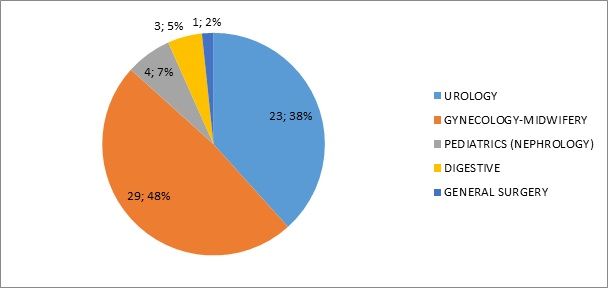
Fifty-nine patients have been recorded (48 women and 11 men) who were referred to Pelvic Floor Unit mainly by services of Urology and Gynecology, and in Pediatrics by Pediatric Nephrology (Figure 1). The average age was 54 years and there were 6 subjects under 18 years of age.
The SUI and mixed were the most common UI types in this sample of subjects (Table 3).
Table 3. Types of incontinence.
| TYPE OF INCONTINENCE | 59 (100%) |
| Mixed UI | 20 (34%) |
| Stress UI | 22 (37%) |
| Urgency UI | 9 (15%) |
| FECAL INCONTINENCE | 8 (14%) |
Among patients with UUI, only one had sensory UUI, the rest of UUI was motor-type. Four patients had both a diagnosis of UI and fecal incontinence. A male patient with chronic pelvic pain (two years of evolution) was diagnosed with Pudendal nerve neuropathy. A patient, despite her urine leaks, denied her symptoms and diagnosis of UI. From the studied patients, 2 pediatric and 2 adult patients did not attend their appointment at the Pelvic Floor Unit.
Table 4 sets out the main risk factors and associated pathologies.
Table 4. Risk factors and associated pathology.
| Macrosomico fetus♀ |
|---|
| Instrumental labour♀ |
| Episiotomy♀ |
| Cystocele♀ |
| Urethrocele♀ |
| Rectocele♀ |
| Prolapse♀ |
| Colonic Neoplasms♀ ♂ |
| Hysterectomy♀ |
| Prostate adenocarcinoma ♂ |
| Overweight -Obesity ♀ |
| Dificult to defecate ♂ ♀ |
| Previous surgery♂ ♀ |
| Childish enuresis |
| Arterial hypertension♂ ♀ |
♂:hombre.
♀:mujer
In addition, 25.42% of the subjects were diagnosed with nervous depression (33.3% were men, 66.6% women), and 20.4% of the women had thyroid pathology. One patient had a previous diagnosis of acute transverse spinal cord syndrome, and there were two cases of pelvic fracture.
Table 5 refers to the treatments given, including in physiotherapy the following pelvic floor protocol of an average duration of one month: 4 sessions of Kegel and hypopressive exercises, 8 sessions of electrostimulation or biofeedback (BFB) or electrostimulation with BFB, and in certain cases, neuromodulation of the posterior tibial nerve and dry needling of trigger points, in addition to behavioral techniques and guidelines for home.
Table 5. Types of urinary incontinence treatment.
| TYPE OF TREATMENT | |
|---|---|
| Physiotherapic | 59 (100%) |
| Electrotherapy (BFB-EMG, electrostimulation) | 24 (40,6%) |
| Pharmacological | 16 (27,1%) |
EMG: electromyography
Depending on to the urinary loss, frequency and quantity increase the number of sessions and physiotherapy techniques are personalized. In our study 3 patients repeated treatment by reactivation of their incontinence, and the rest were discharged due to resolution or improvement of their symptoms.
The more used pharmacological treatments with the patients were Vesicare, Toviaz, Detrusitol and Betmiga 50, as well as drugs scheduled for their general pathology (hypertension, diabetes, thyroid disease, depression, etc.).
In this Unit of Pelvic Floor the effect on quality of life was assessed by means of the questionnaire for urinary incontinence (ICIQ-SF). After rehabilitation treatment in an interval of 2-3 months, the results of the ICIQ-SF improved or were negative, decreasing significantly the number of times of leaking of urine per day, even from several times per day to leaks of two or three times per week.
DISCUSSION
Although the studied population was small, the results of our work are in line with different articles consulted about the disease under study.
Loss of control of faeces as well as the urinary one have a physical, psychological and social impact on the person who suffers them.
The prevalence of fecal incontinence in the general population is 0, 5-1, 5%, increasing to 13 per thousand in women older than 65 years.
In general it is supported that the stress urinary incontinence predominantly affects women between 20 and 50 years of age and that the symptoms of urgency incontinence are more frequent as the patients’ age increases, especially from 65 years. About 60% of UUI ends being mixed.
Mixed and SUI occur more frequently in women with more number of children 14. The incidence of UI is clearly greater in the female sex. Obstetric history is decisive. About 13% of patients have some form of incontinence after the first labour. The average prevalence of UI in women in Spain, whereas any type and severity, is estimated in 40.6%. Of them, only between 15 and 40% seek medical help for this problem 15.
The World Health Organization (WHO) estimated that in 2003 the number of patients with UI in Spain was more than three million two hundred thousand people. The cost involved in this disease is not easily quantifiable, but it is estimated that spending on absorbent for our national health system comes to be 3.2% of the total of the pharmaceutical benefit (about 210 million euros in 2001). To this amount, it should be added the expenditure on medicines, consultations and treatments due to pathologies derived by these disorders like depression, injuries for falls, urinary tract infections, etc... 13.
Variations in prevalence Figures are mainly due, to the different methods used for diagnosis, among others, no formally validated questionnaires; to the different definitions used and the characteristics of the sample of the studied population 17.
Any strategy, that seeks to improve the attention to this health problem, has to consider firstly to increase its detection. Health professionals have a vital role in this task, but they require useful tools which do not pose a significant overload in the daily activities 14. Once the patient is referred to the Pelvic Floor Unit in our study, the first session included a detailed assessment through some questionnaires and physical examination. The ICIQ-SF is a questionnaire that is aimed at the detection of the UI in any fields of healthcare.
The therapeutic approach to pathologies of pelvic floor has had "bad press" from immemorial time due to bad functional outcomes that the surgeries offered to these patients. According to urology professionals from the Hospital Rio Hortega in Valladolid, this can be due to several causes:
Inadequate surgical indication caused by misdiagnosis.
Poorly reviewed treatments (biased retrospective studies).
"Sporadic" surgeries performed by professionals with little experience on the issue since they did not have enough case.
Absence of a basic and experimental research.
Because of this, it is estimated that 33% of surgical interventions for pelvic floor dysfunctions are repeat interventions by poor results of previous surgical procedures21
Drug treatment is mainly focused on the alterations of bladder emptying and the UUI. There is currently no ideal medication that can solve all the dysfunction of pelvic floor. It is relevant to highlight that the importance of these drugs is subject to side effects that, in the majority of cases, tend to be frequent and intense 9
For all these reasons, Pelvic Floor Units have been created in some hospitals of our country. Their main objective is the comprehensive approach to the dysfunctions of the pelvic floor. In order to do that, in addition to medical personnel (urologists, gynecologists, proctologists/surgeons, physiatrists, anesthesiologists and radiologists) there is need of nurses, midwives, physiotherapists and psychologists/sexologists.
The activities in these units include medical consultations, urodynamic studies, surgical procedures, avant-garde techniques as sacral neuromodulation, consultations of catheterization (nursing), treatments such as physiotherapy (procedures such as Neuromodulation of the tibial nerve, administration of drugs using electric current, etc.). In the Pelvic Floor Unit of the University Clinical Hospital in Valladolid, the rehabilitation physician prescribe the appropriate treatment, and the pelvic floor physical therapist performs a first assessment session with questionnaires (that includes the ICIQ-SF) and physical examination, after signing an informed consent by the patient, since maneuvers and techniques intracavitary are carried out. Furthermore the patient is informed about the importance of elaborating its voiding diary and is given a questionnaire to complete for 3 days.
The goals of physiotherapeutic treatment are: to eliminate or decrease pain, achieve balanced pelvic statics, normalize anal-rectal function, achieve a non-painful and satisfactory sexuality and improve quality of life.
But not only the care work is important, but it must be complemented by training actions for other health facilities (resident doctors, nursing students and midwives, among others) and health education and prevention of the general population. Last but not least, retrospective studies and prospective trials should be carried out within the unit in order to improve health care and increase the quality standard of the unit. The benefit to society is clear in terms of economic and morbidity 21
CONCLUSIONS
Urinary, faecal or gas incontinence have an important impact on people's daily lives by decreasing their quality of life, especially in emotional aspects. The latter may be one of the reasons for the low rate of urinary incontinence consultation.
Pelvic floor dysfunctions have a significant increase in menopausal women and progress with older age above age 60.
Among urinary incontinence the most common is SUI.
The most common associated pathologies are: obesity, nervous depressions, infancy enuresis, thyroid disease and hypertension.
It is highlighted the number of patients who need pelvic floor rehabilitation after surgery such as: prostate, colon in neoplasms and prolapses.
It is important to note that women patients in pelvic floor rehabilitation have labours with large large foetus, eutocic labours with episiotomies or instrumental labours (clinical evidence of proven pelvic floor damage).
Among the analyzed stories in our study there are patients who are still on treatment and others who have not yet started treatment (on waiting list).
There is a low percentage of relapses or people who return to the unit due to worsening of their incontinence and a minority who do not have any favorable result.
Despite the small population observed during the period of our study, we consider, based on the proven articles, that as a preventive measure it would be useful to conduct health education from childhood in schools, and informational talk directed towards the general population to discover this little-known and as a consequence often mistreated zone of the body.
REFERENCIAS
1. Salinas J, Díaz A, Brenes F, Cancelo MJ, Cuenllas A, Verdejo C. Prevalencia de la incontinencia urinaria en España. Uro A. 2010; 23: 52-66. [ Links ]
2. Damián J, Brenes F, Pastor-Barriuso R, Salinas JI. Estimación de la prevalencia de incontinencia urinaria en España a partir de estudios publicados recientes. Póster presentado en el LXXIII Congreso Nacional de Urología. Barcelona, 13 al 16 de Jun de 2008. [ Links ]
3. Kelleher C. Quality of life and urinary incontinence. En: Cardozo L, Staskin D. Textebook of female urology and urogynecology, Isis Medical Media Ltd., United Kingdom. 2001: 47-58. [ Links ]
4. Espuña M. Incontinencia de orina en la mujer. Med Clin. 2003; 120: 464-472. [ Links ]
5. Hu TW. Impact of urinary incontinence on health-care costs. J Am Geriatr Soc. 1990; 38: 292-295. [ Links ]
6. Ekelund P, Grimby A, Milsom I. Urinary incontinence. Social and financial costs high. BMJ, 1993; 306: 1344. [ Links ]
7. Torre EJ, Montilla M, Higuera F, Sierra M, Jaramillo I, Aguado C. Características de la población que precisa el uso de accesorios para la incontinencia urinaria en un centro de salud urbano. Medicina de Familia. 2002; 1: 15-23. [ Links ]
8. Wallner LP, Porten S, Meenan RT, O'Keefe MC, Calhoun EA, Sarma AV. Prevalence and severity of undiagnosed urinary incontinence in women. Am J Med. 2009; 122: 1037-1042. [ Links ]
9. Brenes FJ, Cozar JM, Esteban M, Fernández-Pro A y Molero JM. Criterios de derivación en incontinencia urinaria para atención primaria Aten Primaria. 2013; 45(5): 263-273. [ Links ]
10. Brescó P. Suelo Pélvico e Incontinencia. Pulso Ediciones. Arbora & Ausonia. Ed. 2011. [ Links ]
11. Monz B, Chartier-Kastler E, Hampel C, Samsioe G, Hunskaar S et al. Patient Characteristics Associated with Quality of Life in European Women Seeking Treatment for Urinary Incontinence: Results from PURE. Eur Urol. 2007; 51(4):1073-81. [ Links ]
12. Papanicolau S, Hunskaar S, Lose G and Sykes D. Assessment of bothersomeness and impact on quality of life of urinary incontinence in women in France, Germany, Spain and the UK. BJU Int. 2005; 96(6):831-8. [ Links ]
13. Martínez E, Ruiz JL, Gómez L, Ramírez M, Delgado M, Rebollo P, González-Segura D, Arumi D. Prevalencia de incontinencia urinaria y vejiga hiperactiva en la población española: Resultados del estudio EPICC. Actas Urol Esp. 2009; 33 (2): 159-166. [ Links ]
14. Modroño MJ, Sánchez MJ, Gayoso P, Valero M, Blanco M, Cuña FO. Estudio de prevalencia de incontinencia urinaria en mujeres de 18 a 65 años y su influencia en la calidad de vida. Aten Primaria 2004; 34(3):134-9. [ Links ]
15. Espuña M, Rebollo P, Puig M. Validación de la versión española de International Consultation on Incontinence Questionnaire-Short Form. Un cuestionario para evaluar la incontinencia urinaria. Med Clin (Barc) 2004; 122(8):288-92 [ Links ]
16. Espuña M, Fillol M, Pascual MA, Rebollo P, Prieto M. Validación de la versión en español del cuestionario Epidemiology of Prolapse and Incontinence Questionnaire-EPIQ. Actas Urol Esp. 2009; 33(6):646-653. [ Links ]
17. Lukacz ES, Lawrence JM, Buckwalter JG, Burchette RJ, Nager CW, Luber KM. Epidemiology of prolapse and incontinence questionnaire: validation of a new epidemiologic survey. Int Urogynecol J. 2005; 16(4):272-284. [ Links ]
18. Barber MD. Questionnaires for women with pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2007; 18(4):461-465. [ Links ]
19. Badia X, Castro D, Conejero J. Validez del cuestionario King's Health para la evaluación de la calidad de vida en pacientes con incontinencia urinaria. Med clín. 2000; 114 (17): 641-680. [ Links ]
20. Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ et al. Guías EAU sobre incontinencia urinaria. Actas Urol Esp. 2011; 35(7): 373-388. [ Links ]
21. Martínez-Sagarra JM, Rodríguez LA. ¿Por qué una unidad del suelo pélvico? Arch Esp Urol. 2010; 63 (9): 752-754. [ Links ]
Received: March 14, 2019; Accepted: July 04, 2019











 texto en
texto en