Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.61 Murcia ene. 2021 Epub 01-Feb-2021
https://dx.doi.org/10.6018/eglobal.412831
Originals
Degree of Therapeutic Adherence of Patients in Intensive Care Units
1Adult Care Professor, Faculty of Nursing, Universidad de los Llanos at San Antonio, Villavicencio Meta Colombia, Calle 37#41-02 Barzal. Colombia.
2Associate Professor. GESI research group leader, Faculty of Nursing, Universidad de los Llanos at San Antonio, Villavicencio Meta Colombia, Calle 37#41-02 Barzal. Colombia.
Introduction.
Adherence to treatment in the scenario of patients with cardiovascular risk factors in intensive care units is fundamental and of interest in health systems.
Objective.
The work sought to analyze factors influencing on therapeutic adherence to treatment by patients with cardiovascular risk admitted to three intensive care units.
Materials and Method.
Descriptive study with quantitative variables with discretional non-probabilistic design, with a sample of 38 patients during a six-month period. Instrument used: “Factors influencing on adherence to pharmacological and non-pharmacological treatments in patients with risk factors for cardiovascular disease”.
Results.
The most prevalent age range was 61 - 70 years (28.8%); 55.3% were men; the degree of adherence to pharmacological and non-pharmacological treatment showed 61% advantage for adherence, and with family support to meet basic needs, 26% with situation of risk for not adhering, 39.4% reported “difficulties in changes of diet due to high costs of foods recommended” and 13% in situation of not adhering to the treatment.
Conclusions.
The work highlights the importance of the provider-patient relation on the degree of adherence from three health provider institutions, evidencing first-level intervention with individual self-care actions. However, a significant percentage of risk and non-adherence are found due to factors related with the patient and the provider, which impacts on readmissions to the intensive care unit.
Key words: Pharmacological treatment; Cardiovascular diseases; Therapeutics; Compliance with Medication; Patient treatment refusal
INTRODUCTION
Some individuals have a high risk of cardiovascular morbidity and mortality because they have high levels of some risk factor of cardiovascular disease established. In 2015, 17.7-million people died due to this cause, which represents 31% of the deaths registered globally. Cardiovascular diseases will be responsible for 60% of the damage (morbidity) and for 73% of all deaths occurring globally for 2020, a relative 30% increase with respect to that observed currently 1.
In chronic diseases, especially those of cardiovascular origin, intervene environmental, social, and lifestyle factors, among others 2. Cardiovascular risk factors are those biological signs and acquired habits identified in the general population 3. Currently, cardiovascular disease is recognized as a relevant public health problem, which demands intervention from health professionals, given increased mortality rates and prevalence of risk factors 4. Identifying and evaluating cardiovascular risk factors acquires special importance in certain clinical contexts that increase said risk and the complexity of their control 5, particularly, when the user is diagnosed and under treatment; thus, estimating vascular risk and marking the therapeutic objectives to control the risk factors in synergic and adequate manner 6, while also thinking of the therapeutic and non-therapeutic adherence, the family support network, and of course, aperture of health services.
The World Health Organization (WHO) defines therapeutic adherence as “the degree in which a person's behavior: taking medications, following an eating regime, and executing lifestyle changes, correspond with the recommendations agreed with a health care provider” 7. The importance of adherence to treatments as determinant of successful results in medical treatments, better health conditions and - with it - improved quality of life of those affected 8.
Adherence to treatment implies, above all, that the patient and family be aware of the cardiovascular disease, the capacity and management individuals have of being agents of their own care through prevention of risk factors. Orem 9, denominated it as the agency capacity of self-care, which implies a process of dynamic participation by people in the care of their health, a process through which the individuals discern and decide what they can and should do with respect to this regulation, evaluate and reflect on their specific capacities to commit -implicit here the responsibility- with the care of their own health. The principal objective of these reflected decisions and actions is to satisfy the needs of self-care over time and/or in situations of altered health status.
Thus, not adhering to treatment implies, in the long term, one of the principal clinical problems 10 in cardiovascular patients and continues being an obstacle to improving their health and quality of life 11,12; however, education and therapeutic drug monitoring programs promote acquisition of knowledge, which has the direct consequence of increasing the percentage de patients with cardiovascular risk who meet the therapeutic objectives 7.
Various methods exist to measure adherence to pharmacological and non-pharmacological treatment. This study established the instrument “factors that influence on adherence to pharmacological and non-pharmacological treatments in patients with cardiovascular disease risk factors”, which permits integrally measuring the therapeutic regime in patients suffering from chronic non-transmissible diseases. The purpose of the research was to analyze the factors that influence on the therapeutic adherence to the pharmacological and non-pharmacological treatment of patients with cardiovascular risk factors admitted due to a cardiovascular event to intensive care units in the city of Villavicencio, Meta - Colombia.
METHODS
Design, population and sample size
The research was a quantitative, descriptive and cross-sectional study with a non-probabilistic, discretional design, which selected all the patients admitted to three intensive care units in Villavicencio, Meta, during a six-month period, with daily collection, initially revising the clinical history and then recognizing patients with the following inclusion criteria: patients with cardiovascular risk factors admitted to intensive care unit due to a cardiovascular event, being registered and active in the first level health promotion program for over one year, accepting the informed consent, and having an acceptable mental health status through the MINI-MENTA evaluation13; patients were under sedation and daily monitoring was conducted until gathering the inclusion criteria to obtain a sample of 38 patients.
Statistically, these patients have a prolonged stay (5 to 30 days) and the three Health Provider Institutions (IPS, for the term in Spanish) have a capacity of 7 to 8 beds for management of different specialties. The instrument used was version 4 of “Factors that influence on adherence to pharmacological and non-pharmacological treatments in patients with cardiovascular disease risk factors”, which has face, content, and internal consistency validity and reliability according to Cronbach's alpha of 0.84, initial design by Bonilla and Gutiérrez 8,14,16, indicating an instrument with good correlation of reagents and homogeneity to evaluate adherence 8. It has four dimensions: dimension I: Sociodemographic factors; dimension II: Factors related with the health provider system and staff; dimension III: Factors related with the therapy; and dimension IV: Factors related with the patient. The items were answered through a Likert-type scale of never = 0, sometimes = 1, and always = 2, whose result permits identifying three situations of adherence taken by the authors: individuals with adherence to treatment, behaviors that indicate that their adherence is good or perform an important number of actions that indicate they follow the recommendations of the treatment 80%-100% (38-48); individuals with risk of not adhering to the treatment or of not performing or carrying out actions to follow their treatment 60%-79% (29-37); and individuals who are not adhered to the treatment, which indicates that they do not follow the instructions of the treatment 60% (<29) 15,16.
The results were analyzed under the descriptive statistical technique and measure of central tendency and position. Information was processed via SPSS® version 20.0.
Ethical considerations adhered to Resolution 008430 of 1993 by the Ministry of Health15: authorizations bioethical endorsement and informed consent of the participants, guaranteeing absolute reliability of the information and anonymous treatment of the informant. The research followed the international principles established in the 1975 Helsinki declaration by the World Medical Association and had bioethical approval by Universidad de los Llanos.
RESULTS
Sociodemographic and clinical variables of the participants
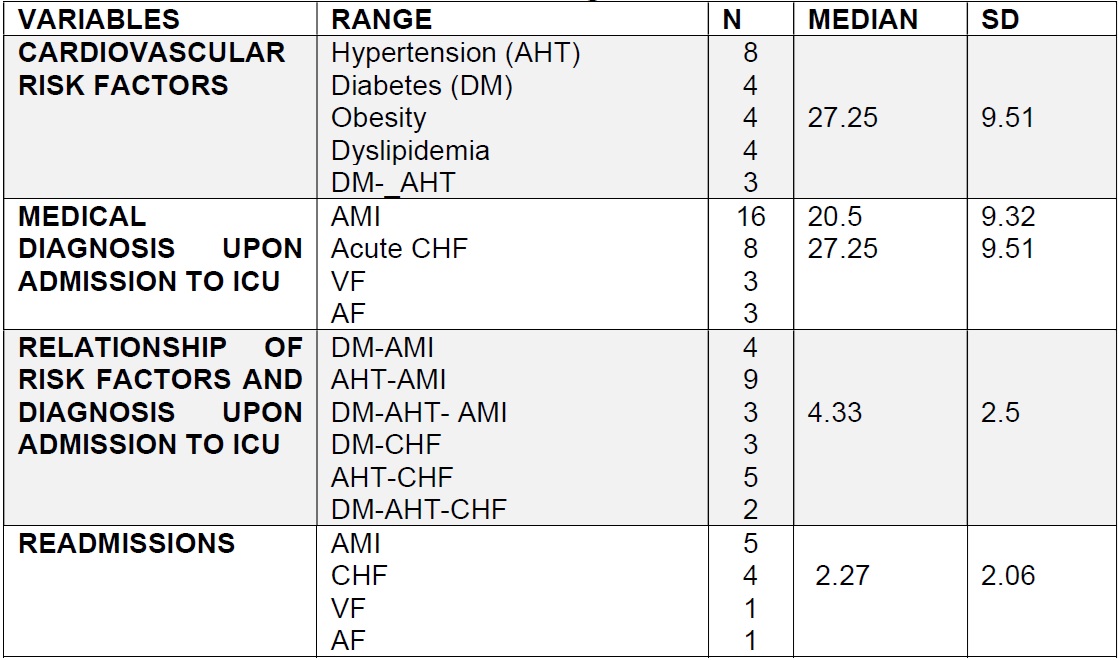
The most predominant age range were 61 - 70 years (28.8%) and 71 - 80 years (26.3%) and with a lower age range 30 to 50 years (5.2%); 55.3% were men. With regards to marital status, 31.5% were married and 29.9% were common law. With respect to economic level, 36.8% were in socioeconomic level one and 34.2% in level three; 13.1% were illiterate or only had incomplete primary (36.8%), 52.6% correspond to the subsidized regime, patients with higher degree of cardiovascular risk had hypertension followed by diabetes (Table 1).
Degree of adherence to the pharmacological and non-pharmacological treatment by the cardiovascular patient
The group of patients with advantage to adhere to treatments is at 61%, in Dimension I, Socioeconomic factors, the vast majority indicated always “having economic availability and family support to meet basic needs, complying with their treatment, affording medications, possibility to travel to the place of consultation, and able to read written information on the management of the disease”. However, an important percentage (39.46%) manifest sometimes and never 21%.
Dimension II, Factors related with the provider. When inquiring about the health system and staff, 63.15% stated that the people providing care always answer their questions about their treatment and provide follow up, as well as guide them on how to adjust the schedules of the medications according to their daily activities. Within the Influencing factors, these never (7.89%) responded to their concerns and received guidance.
In Dimension III, Factors related with the therapy, 76.31% state that “diverse occupations in and out of the home never hinder following the treatment, and 52.63% state that the distance from their home to the doctor's office hinders their complying with the appointments, 60.62% never have doubts about how to take the medications, 76.31% interrupts the treatment when their symptoms improve”, and 63.15% and 47.35% believe there are customs on foods and exercise that are difficult to change.
In Dimension IV, Factors related with the patient, 84.21% are always “convinced the treatment is beneficial and that is why they continue taking it to improve their health”, 78.94% are always “interested in knowing about their health condition and how to care for themselves”, and 81.57% always wish “to continue caring for their health”, 26% sometimes and 5.26% never, unfavorable responses for adherence and their self-care.
The dimension “factors related with the health system provider and staff” ( = 34.62; SD = 6.61), indicates that a group of patients felt supported by the physician and the nurse, followed by the “factors related with the therapy” (
= 34.62; SD = 6.61), indicates that a group of patients felt supported by the physician and the nurse, followed by the “factors related with the therapy” ( = 24.09; SD = 5.01) with benefits in complying with the medical appointments, clarity in how to take the medications and continuity with these even if they feel improvement; while the lowest are “factors related with the patient” (
= 24.09; SD = 5.01) with benefits in complying with the medical appointments, clarity in how to take the medications and continuity with these even if they feel improvement; while the lowest are “factors related with the patient” ( = 20.216; SD = 5.25) (Table 2).
= 20.216; SD = 5.25) (Table 2).
DISCUSSION
The sociodemographic characteristics indicate that 70.7% of the population studied is classified as elderly adult (> 60 years of age), similar to studies conducted in Colombia 8,17,18,19, and in America (17); increased age is related with the presence of CNTD; 55.3% were of male sex, in coherence with studies 8,20,19, indicating that men have a higher risk of cardiovascular disease 21 than women and are affected at early ages20.
In the educational level, it was found that 13.1% of the patients have no level of studies and 63.1% have incomplete or complete primary. Studies report that individuals with a basic level of primary studies or who are illiterate have a medium risk of not adhering to pharmacological treatment, besides not generating protective behaviors against the health situation they are encountering 9.
The socioeconomic level of the population is 1 and 2, with 60.4% and 52.6% in the subsidized health regime; similar investigations show that the low economic level of the people is a risk factor for adherence to pharmacological and non-pharmacological treatment 8,20. Regarding the marital status, 61.4% are married or in common-law union, in keeping with Colombian studies 20, where the support network is a protection factor in adherence.
In relation to cardiovascular risk factors, the study found hypertension (21%), diabetes (10.5%), obesity and dyslipidemia (10.5%) and the cardiovascular event with the highest rate of readmission was AMI (13.1%), followed by CHF (10.5%), with readmissions at 28.1%.
Degree of adherence. It was found that 61% of the patients are in situation of advantage for adherence; 26% of them are in situation of risk of non-adherence, and 13% in situation of non-adherence, coherent with other research 19,20,22,23 at national level where the advantage for adherence was the highest. The group of patients in advantage for adherence to treatment generate actions to respond with behaviors that favor adherence to treatment. However, the socioeconomic factors report difficulties in changes in diet due to the high cost of the foods recommended, in spite of manifesting economic availability and family support. This indicates the importance of education in patients and their families on themes of nutrition, agreeing with national research 8,20, and highlighting the importance of nursing professionals placing greater emphasis on educating patients on adequate diets, bearing in mind the treatment, customs, and foods typical of the region 20.
In factors related with the health system provider and staff, which evaluates the degree of assertive communication between patients and health staff, it was found that the majority feel the physician and nurse give them clear explanations on the benefits, results and on how to adjust medication schedules according to their activities, coherent with other research 8,20,23, where scores are high in this dimension; however, recognizing the need for the medical and nursing staff to emphasize on processes of two-way communication, adjusting processes to the educational needs of the patients, through assertive communication, so that it permits listening to their concerns, motivations, and expectations.
Factors related with the therapy indicate better pharmacological and non-pharmacological adherence behavior, agreeing with other studies 8,19, where therapeutic adherence increases when providing education about the importance of the treatment and its compliance is evaluated constantly. Factors related with el patient indicate they know, guarantee continuity and responsibility with their treatment and their disease, in coherence with other studies 8,20,23, with this being one of the highest-scored dimensions, indicating that when patients know the disease and its treatment, there is higher degree of adherence, an opportunity the health staff must avail of to generate self-care actions in the family and patient.
The group of patients at risk of not adhering to the treatments (26%) evidenced that socioeconomic factors affect notably the patients and place in danger the capacity to generate or maintain adherence behaviors; similar to other research 8,20,23,24, with low perception in adherence with this group of patients. The factors related with the health system provider and staff is a factor that increases the risk of non-adherence in this group of patients, implying that often the health staff becomes a barrier rather than support for adherence. Research 19 indicates the influence of this factor on adherence to pharmacological and non-pharmacological treatment. The factor related with the therapy indicates that lack of knowledge of the disease and its treatment lead patients to make decisions, like that of interrupting the treatment, agreeing with studies by Ortega and Vargas 20. Finally, the factors related with the patient indicate a level of discouragement in this group to continue with the treatment, similar to research with Colombian population 20, which mention that this group requires greater support, monitoring, and information by the health staff. Nevertheless, it is highlighted in another study 23, where patients recognize that one of the principal motives for the low adherence to treatment is personal irresponsibility regarding the treatment.
The group of patients in situation of non-adherence to treatments (13%), in relation to socioeconomic factors, indicates lack of economic capacity by this group of patients to obtain the medications, follow an adequate diet, and lack of support networks. Similar studies coincide with the results exposed 8,20,23, which state that level of schooling, lack of support networks and economic support in this group are risk factors that intervene in non-adherence. The factors related with the provider and influencing factors indicate greater accompaniment by the health staff and assertive communication with this group, indicating 20 that nursing professionals play an important role in providing support and education as a form of intervention for self-care actions.
Factors related with the therapy evidence greater lack of knowledge for the disease treatment and management, much of this related with the level of schooling 8,20, motivation and cultural aspects, and family support 23. Factors related with the patient is level of lack of knowledge this group has regarding the disease and treatment. Under this circumstance, nurses play an important role, with actions of identifying educational needs that permit grasping self-care actions to maintain a better quality of life. Similar studies 23 indicate the importance of a cognitive behavioral model where knowledge and conduct play an important role in adherence by the patients.
Correlation of adherence according to gender, age, and schooling. No significance was found between adherence with variables of gender, age and schooling (Table 3). Regarding gender, similar studies found no significant difference in the dimensions of adherence to treatment 23. However, research with relation to the association between age and adherence warn that when age is over 75 years and comorbidity exists related with cardiovascular disease 8, risk of non-adherence is high, as well as treatment interruption 23. Statistically significant difference was noted, indicating that increased schooling leads to greater adherence to treatment 23,25.
CONCLUSIONS
During the research, it is shown that socioeconomic factors and services offered by the health system, regarding education and providing services, are determinant of adherence.
Likewise, self-care is evident in behaviors, like attendance to medical appointments and continuity of pharmacological treatment, a protective factor that contributes to patients not being readmitted to ICU; however, this population shows increased readmissions and prolonged hospital stay, results of great impact for this type of population, calling for priority intervention. On this particular issue, it would be important to conduct research to delve into other possible causes that somehow affect adherence to pharmacological and non-pharmacological treatment and, consequently, non-improvement of their health situation.
These results are quite important for the study population and further studies are required to broaden the sample from the whole cardiovascular population from the health provider institutions, taking in patients from different stages of their disease, not only in critical state, thus, intervening in therapeutic adherence according to the dimension altered, in early manner to avoid progression of the disease and reaching the critical state, like the population in this study.
From the primary care, it is quite clear that the intervention in this population is key since the moment patients are aware of their disease, like hypertension and diabetes among others, controlling these in timely and effective manner so patients do not develop cardiovascular diseases, which the major cause of hospitalizations in ICU, increased readmissions, prolonged stay, and hospital costs. Finally, it must be mentioned that adherence to treatment must be an important component in health systems and must be coordinated integrally and in interdisciplinary manner involving the health staff, families, and patients.
REFERENCES
1. Benítez G, Paiva T, Ortellado J, González G, Sánchez CManual de Manejo de Enfermedades Crónicas No Transmisibles, desde la Atención Primaria de Salud. Dirección General de Vigilancia de la Salud. Asunción: Primera Edición; 2015. [ Links ]
2. Mayoral JM et al. Las enfermedades crónicas como prioridad de la vigilancia de la salud pública en España. Gaceta Sanitaria. 2016;(30)2:154-157. Disponible en: https://doi.org/10.1016/j.gaceta.2015.12.008 [ Links ]
3. Cruz-Sánchez E et al. Factores de riesgo cardiovascular en estudiantes de enfermería de una universidad pública. Revista Enfermería Universitaria [Internet]. 2016:13(4):226-232. Disponible en: https://doi.org/10.1016/j.reu.2016.09.004 [ Links ]
4. Areiza M et al. Conocimiento y factores de riesgo cardiovascular en pacientes ambulatorios. Rev Colomb Cardiol. 2017; xxx(xx):1-7. Disponible en: http://dx.doi.org/10.1016/j.rccar.2017.07.011 [ Links ]
5. Martín-Portugués IA, Sánchez Mesa B, Sánchez Lora FJ Factores de riesgo cardiovascular en situaciones clínicas específicas: diabetes mellitus, insuficiencia renal, enfermedades inflamatorias crónicas, infecciones crónicas, VIH, edad y sexo. Medicine-Programa de Formación Médica Continuada Acreditado. 2017;12(42):2503-2508. Disponible en: https://doi.org/10.1016/j.med.2017.10.004 [ Links ]
6. Salgado Ordóñez F, Sanz Cánovas J, Pacheco Yepes R. Riesgo cardiovascular. Medicine - Programa de Formación Médica Continuada Acreditado. 2017;12(42):2477-2484. Disponible en: https://doi.org/10.1016/j.med.2017.10.001 [ Links ]
7. López Romero LA, Romero Guevara SL, Parra DI, Rojas Sánchez LZ. Adherencia al tratamiento: Concepto y medición. Hacia promoc salud. 2016;21(1):117-137. Disponible en: https://doi.org/10.17151/hpsal.2016.21.1.10 [ Links ]
8. Salcedo Barajas A, Gómez Ochoa AM. Grados de riesgo para la adherencia terapéutica en personas con hipertensión arterial. Avances en Enfermería. 2014;32(1):33-43. Disponible en: http://dx.doi.org/10.15446/av.enfermv32n1.46033 [ Links ]
9. Raile Alligood, M. Modelos y teorías de enfermería. 2011. 7 ed. España: ELSEVIER. [ Links ]
10. Sandoval D, Chacón J, Muñoz R, Henríquez Ó, Koch E, Romero T. Influencia de factores psicosociales en la adherencia al tratamiento farmacológico antihipertensivo. Resultados de una cohorte del Programa de Salud Cardiovascular de la Región Metropolitana, Chile. Revista Médica de Chile. 2014;142(10):1245-1252. Disponible en: https://doi.org/10.4067/S0034-98872014001000003 [ Links ]
11. Conthe P et al. Pinto, Adherencia terapéutica en la enfermedad crónica: estado de la situación y perspectiva de futuro. Revista Clínica Española. 2014;(214)6:336-344. Disponible en: https://doi.org/10.1016/j.rce.2014.03.008 [ Links ]
12. Bonilla Ibáñez CP. Adherencia y factores que influyen en la adherencia a tratamientos farmacológicos y no farmacológicos en personas que presentan factores de riesgo de enfermedad cardiovascular. Una revisión de literatura. Bogotá D.C. Colombia: Editorial Universidad Nacional de Colombia. [ Links ]
13. Minimental escala psicométrica breve para evaluar el estado cognitivo de las personas disponible en: http://www.ome.es/media/docs/Novedad_Test_Minimental.pdf [ Links ]
14. Bonilla C, Gutiérrez E. Desarrollo y características psicométricas del instrumento para evaluar los factores que influyen en la adherencia a tratamientos farmacológicos y no farmacológicos en personas con factores de riesgo de enfermedad cardiovascular. Avances de Enfermería. 2014;32(1):53-62. Disponible en: http://dx.doi.org/10.15446/av.enfermv32n1.46035 [ Links ]
15. Republica de Colombia. Ministerio de salud. Resolución Numero 8430 de 1993. Disponible en: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/DIJ/RESOLUCION-8430-DE-1993.PDF [ Links ]
16. Ortiz Suarez, C. Instrumento para evaluar la Adherencia a tratamientos en pacientes con factores de riesgo cardiovascular. Avances de Enfermería. 2010;28(2):73-87. [ Links ]
17. Mozaffarian D et al. Heart Disease And Stroke Statistics. A report from de American Heart Association. Circulation. 2016;133(8):e38-360. Available from: https://doi.org/10.1161/CIR.0000000000000350 [ Links ]
18. Salgado Ordóñez F, Sanz Cánovas J, Pacheco Yepes F. Riesgo cardiovascular. Medicine - Programa de Formación Médica Continuada Acreditado. 2017;12(42):2477-2484. Disponible en: https://doi.org/10.1016/j.med.2017.10.001 [ Links ]
19. Hernández DY. Relación entre estados de salud y riesgos de no adherencia al tratamiento en pacientes en rehabilitación cardiaca. Avances en Enfermería. 2015;33(1):114-123. Disponible en: http://dx.doi.org/10.15446/av.enfermv33n1.41825 [ Links ]
20. Ortega Oviedo SI, Vargas Rosero E. Grado de adherencia a tratamientos en personas con riesgo cardiovascular. Avances en Enfermería. 2014;32(1):1-25. Disponible en: http://dx.doi.org/10.15446/av.enfermv32n1.46032 [ Links ]
21. Rojas-Reyes J, Florez-Florez ML. Adherencia al tratamiento y calidad de vida en personas con infarto agudo de miocardio. Aquichan. 2016;16(3):328-339. Disponible en: Doi: 10.5294/aqui.2016.16.3.5 [ Links ]
22. Bonilla C. Diseño de un instrumento para evaluar los factores que influyen en la adherencia al tratamiento farmacológico y no farmacológico en personas con factores de riesgo de enfermedad cardiovascular: validez de contenido y validez aparente del mismo [tesis magistral]. Bogotá: Facultad de Enfermería, Universidad Nacional de Colombia; 2006. [ Links ]
23. Zanbrano CR, Duitama JF, Posada VJ, Florez JF. Percepción de la adherencia a tratamientos en pacientes con factores de riesgo cardiovascular. Rev Fac Nac Salud Pública. 2012; (30)2:163-174. [ Links ]
24. Herrera Guerra E. Adherencia al tratamiento en personas con hipertensión arterial. Rev Av enferm 2012;(30)2:67-75. [ Links ]
25. Rodríguez-Abt JC, Solís-Visscher RJ, Rogic-Valencia SJ, Román Y, Reyes-Rocha M. Association between hypertension awareness and treatment adherence in hypertensive patients at hospital nacional edgardo rebagliati martins in Lima, Perú, 2015. Revista Facultad de Medicina. 2017;65(1):55-60. Disponible en: http://dx.doi.org/10.15446/revfacmed.v65n1.56773 [ Links ]
Received: February 02, 2020; Accepted: July 16, 2020











 texto en
texto en