Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.61 Murcia ene. 2021 Epub 01-Feb-2021
https://dx.doi.org/10.6018/eglobal.430221
Reviews
Body temperature and heating temperature in major burns patients care
1Master Science Research in Nursing. Critical Care Nurse. Hospital Universitario Rio Hortega. Valladolid. Spain.
2Teacher in Master's degree Science Research in Nursing. Universitat Rovira i Virgili. Tarragona. Spain.
Objectives:
To describe the heating methods and their application to maintain body temperature in majors burn patients.
Methodology:
Bibliographic review carried out between September 2019 and February 2020 about the thermoregulation and heating of the burn patient in the CINHAL, CUIDEN, PUBMED, MEDES and WOS databases in Spanish and English, documents from the last 10 years, from which 26 were analyzed.
Results:
Hypermetabolic response and hypothalamic reprogramming cause an increase in basal temperature in burn patients between 37 and 38.5ºC without infectious origin. To decrease the energy expenditure at rest and the hypermetabolic response, it is possible to act through a high ambient temperature between 28 and 32ºC as passive external heating.
Discussion:
Other external heating methods can achieve this goal such as convective air blankets, heating plates, or surface systems.
Conclusions:
The recommendation of warming by means of high ambient temperature, which creates hostile environments for workers and patients, should be reviewed through the study of the inclusion of active external warming methods.
Key words: Burn patient; Body Temperature Regulation; Heating; Energy metabolism; Nursing Care
INTRODUCTION
The skin is the largest organ of the body, performs functions of homeostasis maintenance and thermal regulation. Loss of skin from a burn will require temporary replacement of these functions until recovery. WHO defines burns as a global health problem, with a prevalence 7 times higher in developing countries, mainly occurring domestically, with prevention being the intervention that can most reduce mortality (1.
In Spain, there were 1,757 deaths from accidents of fire, smoke and hot substances, in the last decade, 1996-2016, with an upward trend since 2011. In 2017, 9,186 burn income was recorded with an incidence was 7 cases per 100,000 inhabitants and a total of 39,170 hospital stays. The European Burns Association (EBA) describes that 14 out of 100,000 people will need hospital care for burns per year 2.
These patients usually develop hypothermia after burning and when transferred to a burn unit they receive more specialized care (3. Burns with an extension greater than 20% Total Burn Surface Area (TBSA), advanced age, and other morbidities increase your risk of hypothermia.
Between 40-80 % of patients suffering severe burns have hypothermia during the acute phase (3,5,6, directly related to the extent of the burn. Hypothermia has higher prevalence in older age, burns greater than 40% TBSA and female (5,6,7. In addition, the presence of hypothermia is described as an independent factor that can increase the mortality of these patients by up to 5% 5.
Since the accident that causes the burn, begins the process of care of major burn patient. The nurse has the competence to issue the hypothermia diagnosis or risk of hypothermia, establishing a care plan, and defines normothermia as its target. The heating mechanisms must be adjusted to achieve the target temperature, achieving a balance between production, gain and heat loss.
The aim is to describe the heating methods and their application for maintaining body temperature in major burn patient.
MATERIAL AND METHODS
A bibliographic review was conducted between September 2019 and February 2020, about thermal regulation, warming in hypothermia and metabolic control in burns patients with search terms, DeCS and MeSH: Burns - Burns, Burns, Burns - Burns patient, Hypothermia - Hypothermia, Body Temperature, Body Temperature, Body Temperature Regulation- Body Temperature Regulation, Heating - Heating, Heaters-Heaters, Energy Metabolism - Energy Metabolism , Energy Consumption - Energy Consumption, Basal Metabolism - Basal Metabolism, Physiological Stress - Stress,Physiological, Ambient Temperature Temperature Temperature, Body Temperature - Body Temperature, Nursing Care - Nursing Care, , Nurse - Nurses, Nursing - Nursing, Burn units-Burn Units, Thermal Comfort- Thermal Comfort, in databases: CINHAL, CUIDEN, PUBMED, MEDES, the Web Of Sciencie Metasearcher (WOS), in the secondary databases: Cochrane library, Joanna Briggs Connect, UptoDate, GuiaHealth; and on the referral pages of international patient care societies with ISBI, ABA and EBA burns. Also included was the search for grey literature, doctoral theses in TESEO and other related reference documents. Articles in Spanish and English, published since 2009, were included, a range necessary for the proper definition of the concepts that are reviewed of adult patients with thermal burns, and content related to patient care with burns, heating, thermoregulation or metabolism. Documents of small burns, chemical or electrical burns, inhalation injury, out-of-hospital care or post-acute phase were excluded.
RESULTS
3536 articles were found, according to the databases and search engines consulted, applying search filters with the terms defined above were obtained 199, after screening and selection for further evaluation and analysis resulted in 24 documents. The background and review of the research topic below are set out as categorized by sections.
Body temperature in major burn patient
The loss of the surface of the skin by a burn leads directly to the loss of its functions resulting in an alteration in thermoregulation, alteration of sweat regulation (heat losses by evaporation) and alteration of the regulation of blood flow (heat losses by radiation and convection) 8.
Heat losses of the burn patient are presented by conduction, convection, radiation and evaporation (9. Control of driving losses shall be carried out by acting on the surface that is positioned to the patient either the transport table, bed or surgical table. Treatment on convection losses shall be performed by monitoring environmental temperature and humidity and protecting from air currents. Radiation losses will be losses to the environment, so the patient's body exposure should be limited. And in the face of evaporation losses, contact with wet dressings and sweat control (9. Heating and temperature maintenance measures will be applied to alleviate these losses.
The loss of heat and water through the burn causes an increase in central temperature, reprogramming the hypothalamic regulation, so patients are expected to have a higher temperature of up to 2ºC without infectious focus being around 38,5ºC 10. A body temperature of less than 35ºC 11 should be avoided because of its unwanted effects and despite not knowing the optimal target temperature, it should be greater than 37,5ºC (4.
Hypothermia in burn patients may increase vasoconstriction lesions, cause clotting disturbances, decreased enzymatic activity, impaired breathing, may cause arrhythmias and death 11,12,13. The centralized care offered in a large burn unit provides a controlled and standardized environment indispensable for the survival of these critical and immunocompromised patients 14.
Pre-hospital action and implementation of established recommendations for burn cooling, monitoring the risk of hypothermia and applying heat loss control measures, will determine the progression of hypothermia and the need for faster warming of patients with extensive burns 3,6.
Once stabilized and for the first few hours after the injury, the patient will need to be covered with clean, dry blankets to prevent or limit hypothermia. Measures to maintain body temperature include occlusive dressing to prevent heat loss, local infection and promote healing. The barrier effect of dressings ensures thermal insulation and moisture maintenance, allowing gas exchange. Along with the limitation and control of body exposure, they are relevant factors to avoid decreased body temperature 12.
It is called critical temperature, at the temperature that triggers a thermogenic cell response. As the severity of the burn increases, the critical temperature decreases. While the critical temperature and time to reach it may vary between patients, hypermetabolic response can be controlled by high ambient temperature, minimizing heat losses, improving coagulation and reducing morbidity and mortality 4.
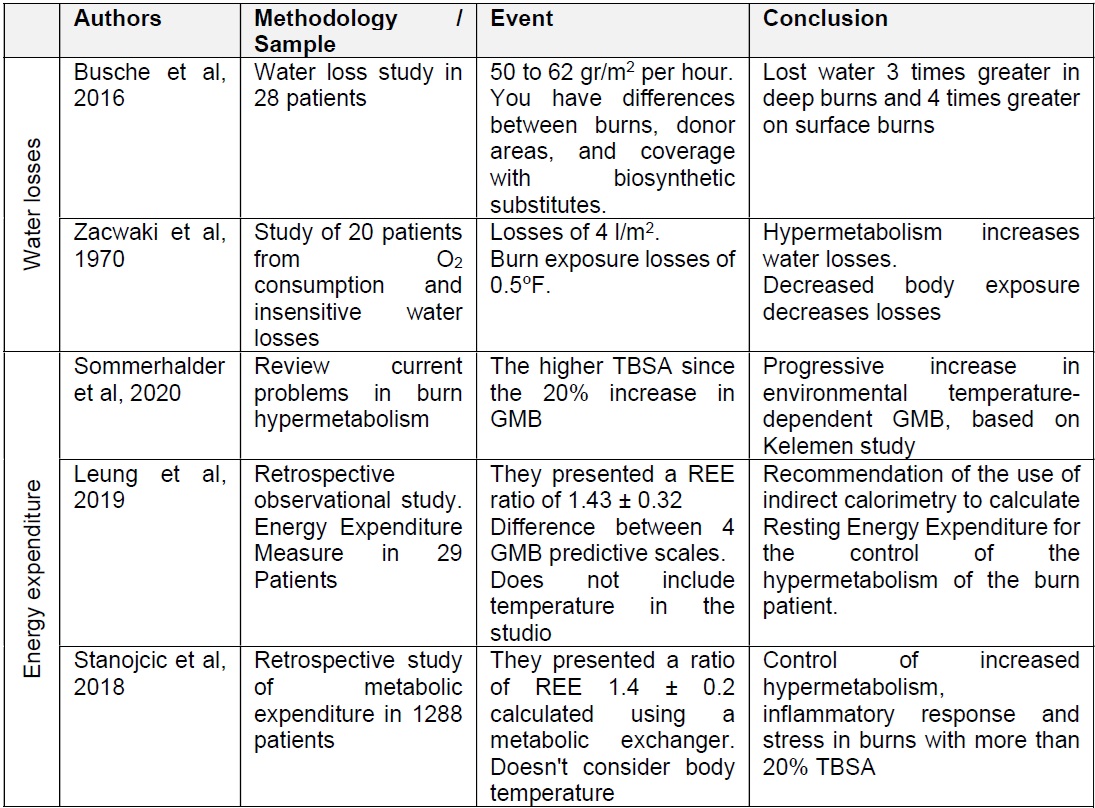
The target temperature range of patients in a study in US burn units was between 36 - 38ºC (15. Despite the absence of a clear definition of the target temperature, there is a relationship between higher body temperature and lower metabolic expenditure. shall be considered in the burn patient (Table 1).
Table 1. Body temperature in major burn patients
*REE Resting Energy Expenditure
**TBSA Total Burn Surface Area
In the care of the burn patient, it should be noted that the baseline temperature of these patients is 38.5ºC, and that a temperature below 37ºC can be considered as relatively hypothermia (16.
Energy metabolism in burn patients
Two phases are considered in the metabolic response of the burn patient, the acute phase ranging from the accident to 72 hours, and the hypermetabolic phase. The hypermetabolic state developed by the burn patient after the acute phase increases energy consumption. Several actions are needed to decrease the effects of hypermetabolism to reduce caloric expenditure, at least so that there is no increase in metabolism (17.
Burns greater than 20% TBSA will develop a hypermetabolic, inflammatory and stress response in a similar way to that developed with burns greater than 40% TBSA 18. It`s recommended to act on hypermetabolism, as its decrease will improve the healing of burns. The early and appropriate nutritional contribution to the patient will intervene on the catabolic state by decreasing energy demand 19.
During the acute phase after burning, the patient has a severe loss of lean body mass, free radical imbalance in relation to antioxidant defense mechanisms and impaired immune function. Intervention through adequate nutritional support and early onset of enteral nutrition will meet the energy demands of proteins, fats, lipids and micronutrients. In addition, the supplement of micronutrients such as glutamine, will contribute to the recovery of lean mass (20.
The metabolic expenditure of burned patients in the study of Stanojcic et al 18 was 1,4 ± 0,2 times the basal metabolic expenditure, while in the study of Leung et al (21 was 1,43 ± 0,32 times the BMR in patients with burns less than 40%.
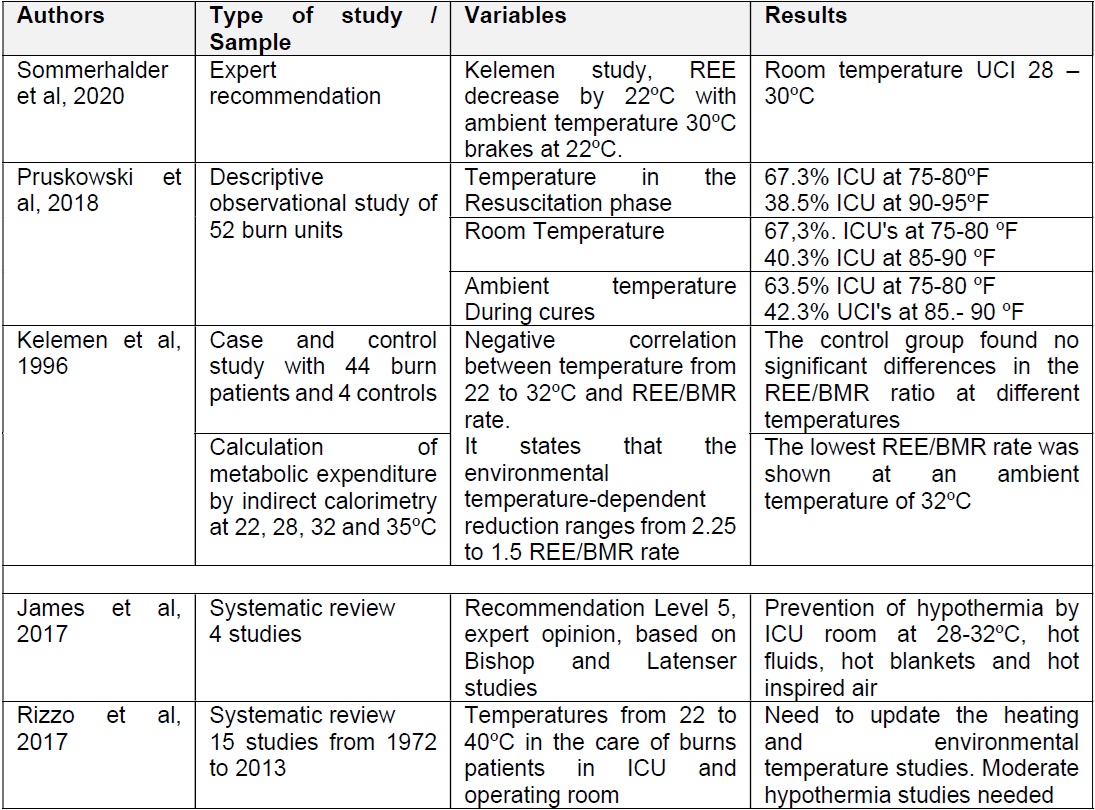
Water losses of up to 4 l/m2 of burn surface area per day are found (22. The evaporation body fluid losses quantified are 3 to 4 times greater than in healthy skin depending on deep second-degree and third-degree burns. It can be assessed by the Trans Epidermal Water Loss index (TEWL), measuring the amount of water in grams that passes through the skin to the surrounding atmosphere, per hour and skin area, being according to the depth of the burn from 50 to 62 gr/m2 per hour (23 (Table 2).
Heating methods
Measures to alleviate heat losses should act in heating and maintaining the patient's body temperature through active internal heating methods such as intravenous hot liquid administration and other heating and extern methods that will be passive and/or active.
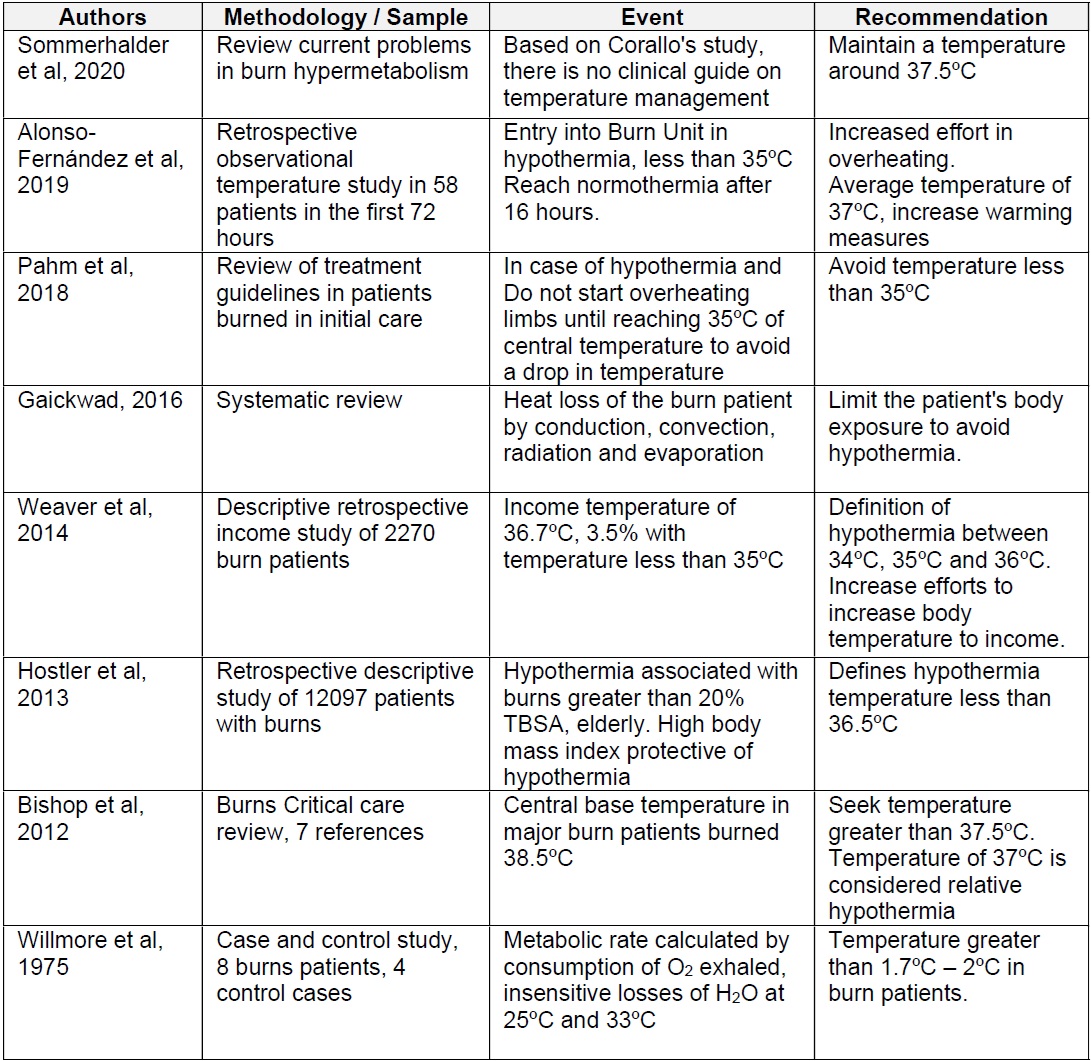
An analysis of the use of heating methods, in US burn units, declared in relation to total cases: 94.2% increase in ambient temperature, followed by 88.5% forced air appliances, 82.7% tempered intravenous liquids, 38.5% conductive heating pads and temperature-regulated intravascular catheter 21.6%15 (Table 3).
Passive external heating: Ambient temperature
As a passive external heating method a high ambient temperature is used, the recommendations place it between 28 and 33º 11). This increase in ambient temperature can reduce Resting Energy Expenditure from 2.0 times to 1.4 times in patients with burns greater than 40% TBSA.
This measure serves to minimize the increase in basal metabolic rate caused by heat generation and water loss by evaporation. It is a Grade B recommendation of evidence by Joanna Briggs Institute (24 providing a warm room with an ambient temperature of 28-32ºC, to prevent hypothermia.
Pruskowski et al (15 observed that the increase in ambient temperature was the most commonly used heating in burn units, using a wide temperature arc of 24 to 35ºC.
To decrease hypermetabolic response, such as non-pharmacological measures, it can be acted by raising the ambient temperature. Kelemen et al (25 found that the ambient temperature range from 30ºC to 32ºC would reduce hypermetabolism in patients with burns from 20% TBSA, reaching a 22% decrease in energy demand compared to an ambient temperature of 22ºC. Environmental temperatures above 32ºC would no longer provide this benefit. There is a relationship between higher burn body surface area and higher temperature demand (25.
Active external heating
Active external heating is obtained by directly applying heat to the surface of the body. The use of convective air as an active external heating method has been studied mainly in the surgical and care field of critical patients (26. This application is effective to achieve normothermia starting from a body temperature of 32ºC. The application of convective air achieves a higher rate of 1ºC of heating compared to other methods (27.
DISCUSSION
The burn patient needs to maintain a higher body temperature due to increased energy expenditure. Maintaining a high ambient temperature decreases hyper-metabolic response and therefore energy consumption. The current recommendations are based on Wilmore's research, which studied the metabolic impact of high ambient temperature applied as a passive external overheating method.
As shown in Table 1, there is a temperature range considered safe, but there is no exact delimitation of an optimal reference temperature for the burn patient. At the same time, in secondary assessment, it is necessary to estimate the effects of external warming in relation to factors such as anxiety, pain or disconfort.
It was observed in a Burn Unit that the average temperature of patients at the end of the acute phase was around 37ºC, when temperatures close to 38ºC are expected, a fact that makes it necessary to reflect on warming measures, and whether the body temperature of non-infectious origin is the best reference value for the maintenance of such measures (5 .In contrast, it has been observed that in patients of pediatric age, this hyperthermal response does not develop as in adults28)..
High ambient temperature has unfavorable effects, such as increased proliferation and growth of microorganisms (29 or heat stress. Maintaining normothermia only by passive external overheating at high temperatures creates harsh working environments. Intervention would be required through the combination of passive external heating methods that could lower the room's ambient temperature and decrease the patient and workers' disconfort.
Several authors and guides recommend the joint use of heating measures such as inspired hot air or hot blankets (9,12,16,27 but there are not precise specifications on the use of an active external heating type, plus there is variability in terms of the time of application and its availability. This method is of limited use in burn patients, as while skin care actions are performed, it cannot be applied comfortably or effectively.
There are experiences with active internal heating methods such as the use of an intravascular catheter intended for thermoregulation as it produces a rapid response in both patient warming and cooling against other methods. Its use is limited in time due to the risk of intravascular thrombosis (30, so treatment cannot be extended more than 72 hours.
An active external heating method that employs heating and cooling rates and range by applying skin gel patches such as Articsun 5000®, the application of which is contraindicated on skin with ulcers, wounds or burns, which prevents its use in the case of patients with extensive burns.
Active external heating methods can improve temperature maintenance and heat loss without creating adverse environments for healthcare professionals during care, further optimizing the thermal regulation of the burn patient. The adequacy of the heating methods could achieve an improvement of the thermal comfort of the patient and the workers in the Burn Unit reaching a decrease in the high ambient temperature.
CONCLUSIONS
The major burn patient needs a body temperature greater than 37 - 37.5ºC reached 38.5ºC, to avoid critical temperature and decrease energy expenditure, controlling hypercatablic state.
The recommended ambient temperature in large burn units is between 28 and 33ºC. The application of high environmental temperatures creates severe environments for workers and patients, so their effective application in these units is variable and requires an adaptation and balance between the needs of the patient and the conditions of the workers.
The recommendation of high ambient temperature heating should be reviewed through the study of the inclusion of active external heating methods in burn patients.
REFERENCIAS
1. OMS. Quemaduras. 2018. Quemaduras. https://www.who.int/es/news-room/fact-sheets/detail/burns. Accedido diciembre 30, 2019. [ Links ]
2. European-Burn-Association. European Practice Guidelines for Burn Care. Minimum level of Burn Care Provision in Europe. Barcelona; 2017. www.eba2019.org. Accedido enero 4, 2020. [ Links ]
3. Weaver MD, Rittenberger JC, Patterson PD, et al. Risk factors for hypothermia in ems-treated burn patients. Prehospital Emerg Care. 2014;18(3):335-341. doi:10.3109/10903127.2013.864354 [ Links ]
4. Sommerhalder C, Blears E, Murton AJ, Porter C, Finnerty C, Herndon DN. Current problems in burn hypermetabolism. Curr Probl Surg. 2020;57(1):100709. doi: 10.1016/j.cpsurg.2019.100709 [ Links ]
5. Alonso-Fernández JM, Lorente-González P, Pérez-Munguía L, Cartón-Manrique AM, Peñas-Raigoso MC, Martín-Ferreira T. Analysis of hypothermia through the acute phase in major burns patients: Nursing care. Enferm Intensiva. 2019. doi: 10.1016/j.enfi.2019.05.002 [ Links ]
6. Hostler D, Weaver MD, Ziembicki JA, et al. Admission temperature and survival in patients admitted to burn centers. J Burn Care Res. 2013;34(5):498-6. doi:10.1097/BCR.0b013e3182a231fb [ Links ]
7. Singer AJ, Taira BR, Thode HC, et al. The association between hypothermia, prehospital cooling, and mortality in burn victims. Acad Emerg Med 2010;17(4):456-459. doi:10.1111/j.1553-2712.2010.00702.x [ Links ]
8. Lang TC, Zhao R, Kim A, et al. A Critical Update of the Assessment and Acute Management of Patients with Severe Burns. Adv Wound Care. 2019;8(12):607-633. doi:10.1089/wound.2019.0963 [ Links ]
9. Gaikwad M. Evidence Summary. Burns Units (Hypothermia): Prevention and Managemen Treatment. Joanna Briggs Inst EBP Database, JBI@Ovid. 2016; JBI15718. [ Links ]
10. Wilmore DW, Mason AD, Johnson DW, Pruitt BA. Effect of ambient temperature on heat production and heat loss in burn patients. J Appl Physiol. 1975;38(4):593-597. doi:10.1152/jappl.1975.38.4.593 [ Links ]
11. Pham TN, Bettencourt AP, Bozinko GM, et al. Advanved Burn Life Support Course. Provider manual. 2018 Update. ChicGO; 2018. [ Links ]
12. Icaza I. Guía Práctica Clínica Sociedad De Quemaduras. Burns. 2016;42(Xxxx):1-76. doi: 10.1016/j.burns.2016.05.013 [ Links ]
13. Cancio LC. Initial Assessment and Fluid Resuscitation of Burn Patients. Surg Clin North Am. 2014;94(4):741-754. doi: 10.1016/j.suc.2014.05.003 [ Links ]
14. Al-Mousawi AM, Mecott-Rivera GA, Jeschke MG, Herndon DN. Burn Teams and Burn Centers: The Importance of a Comprehensive Team Approach to Burn Care. Clin Plast Surg. 2009;36(4):547-554. doi: 10.1016/j.cps.2009.05.015 [ Links ]
15. Pruskowski KA, Rizzo JA, Shields BA, et al. A Survey of Temperature Management Practices among Burn Centers in North America. J Burn Care Res. 2018;39(4):612-617. doi:10.1093/jbcr/irx034 [ Links ]
16. Bishop S, Maguire S. Anaesthesia and intensive care for major burns. Contin Educ Anaesthesia, Crit Care Pain. 2012;12(3):118-122. doi:10.1093/bjaceaccp/mks001 [ Links ]
17. Fagan SP, Bilodeau M-L, Goverman J Burn Intensive Care. Surg Clin North Am. 2014;94(4):765-779. doi: 10.1016/j.suc.2014.05.004 [ Links ]
18. Stanojcic M, Abdullahi A, Rehou S, Parousis A, Jeschke MG. Pathophysiological Response to Burn Injury in Adults. Ann Surg. 2018;267(3):576-584. doi:10.1097/SLA.0000000000002097 [ Links ]
19. Lowe JM, Brody RA. Nutrition Management of Major Burn Injuries. Top Clin Nutr. 2019;34(2):161-171. doi:10.1097/TIN.0000000000000171 [ Links ]
20. Prins A. Review: Nutritional management of the burn patient. S Afr J Clin Nutr. 2009;22(1):9-15. [ Links ]
21. Leung J, Ridley EJ, Cleland H, Ihle JF, Paul E, King SJ Predictive energy equations are inaccurate for determining energy expenditure in adult burn injury: a retrospective observational study. ANZ J Surg. 2019;89(5):578-583. doi:10.1111/ans.15119 [ Links ]
22. Zawacki BE, Spitzer KW, Mason AD, Johns LA. Does increased evaporative water loss cause hypermetabolism in burned patients? Ann Surg. 1970;171(2):236-240. doi:10.1097/00000658-197002000-00011 [ Links ]
23. Busche MN, Roettger A, Herold C, Vogt PM, Rennekampff H-O. Evaporative Water Loss in Superficial to Full Thickness Burns. Ann Plast Surg. 2016;77(4):401-405. doi:10.1097/SAP.0000000000000845 [ Links ]
24. James S, Campbell J Temperature Management (Burns): Intensive Care Unit. Joanna Briggs Inst EBP Database, JBI@Ovid 2019; 2017; JBI13577. [ Links ]
25. Kelemen JJ, Cioffi WG, Mason AD, Mozingo DW, Mcmanus WF, Pruitt BA. Effect of Ambient Temperature on Metabolic Rate After Thermal Injury. Ann Surg. 1996;223(4):406-412. doi: 10.1097/00000658-199604000-00009 [ Links ]
26. Steele JE, Atkins JL, Vizcaychipi MP. Factors at scene in transfer related to the develoment of hypothermia in major burns. Ann Burns Fire Disasters. 2016;29(2):103-107. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5286989/pdf/Ann-Burns-and-Fire-Disasters-29-103.pdf. Accedido marzo 8, 2019. [ Links ]
27. Latenser BA. Critical care of the burn patient: The first 48 hours. Crit Care Med 2009;37(10):2819-2826. doi:10.1097/CCM.0b013e3181b3a08f [ Links ]
28. McEntire SJ, Chinkes DL, Herndon DN, Suman OE. Temperature Responses in Severely Burned Children During Exercise in a Hot Environment. J Burn Care Res. 2010;31(4):624-630. doi:10.1097/BCR.0b013e3181e4ca14 [ Links ]
29. Rizzo JA, Rowan MP, Driscoll IR, Chan RK, Chung KK. Perioperative Temperature Management during Burn Care. J Burn Care Res. 2017;38(1):e277-e283. doi:10.1097/BCR.0000000000000371 [ Links ]
30. Davis JS, Rodriguez LI, Quintana OD, et al. Use of a Warming Catheter to Achieve Normothermia in Large Burns. J Burn Care Res. 2013;34(1):191-195. doi:10.1097/BCR.0b013e31826c32a2 [ Links ]
Received: May 31, 2020; Accepted: September 25, 2020











 texto en
texto en