Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.20 no.64 Murcia oct. 2021 Epub 25-Oct-2021
https://dx.doi.org/10.6018/eglobal.442371
Reviews
Analysis of the programs for the presence of family members in the extrahospital cardiorrespiratory stop in adult patient
1 Gerencia de Emergencias Sanitarias SACYL. Facultad de Enfermería de Valladolid. España.
2 Complejo Asistencial de Segovia. España. inescardaba@gmail.com
Objective:
Explore programs aimed at the participation of family members in situations of CRP in adults in the out-of-hospital setting.
Method:
Narrative review of the scientific literature, in primary databases (Scielo, PubMed, Cuiden and Cochrane Plus and CINAHL), using DeCS and MeSH structured language, from 2005 to 2020, in Spanish and English. 23 studies are obtained.
Results:
Studies show that mourning for family members of a cardiorespiratory arrest in the out-of-hospital setting is less traumatic if they are allowed to be present. Staying with the victim must be ensured unless the professional considers that it is harmful. The advantages of the presence of family members are as much for the family member as for the healthcare team. Despite the existence of a social and ethical need in accordance with the principle of patient autonomy for the implementation of these programs, they hardly exist and this is usually due to the resistance generated by the professionals or managers themselves.
Conclusions:
In the case of cardiorespiratory arrest in adults in the out-of-hospital setting, the main international scientific societies recommend the implementation of programs for the presence of family members, which makes it a necessity. The scientific literature demonstrates more advantages than disadvantages, fundamentally in terms of better grief in family members and greater satisfaction and less possibility of legal claims in health professionals, promoting the humanization of care that would translate into lower healthcare costs in the prevalence of grief pathological.
Keywords: out-of-Hospital cardiac arrest; cardiopulmonary resuscitation; family
INTRODUCTION
Cardiorespiratory arrest (CRA) involves the sudden and unexpected cessation of blood circulation and spontaneous breathing and, therefore, the cessation of oxygen supply to vital organs, with the brain being particularly affected 1)(2)(3. When the brain stops receiving oxygen for 6-8 minutes its cells die, creating an irreversible situation.
In Europe, cardiovascular diseases account for around 40% of all deaths in children under 75. Sudden cardiac arrest is responsible for more than 60% of adult deaths from coronary disease 1)(2)(4. Survival in Europe is about 10% at 30 days 5,6.
The idea of offering relatives their presence in the event of the need for resuscitation manoeuvres in the case of CRA is not new, in fact it has been around for more than 20 years 7.
The European Resuscitation Council (ERC), as an expert international organisation in the field of resuscitation, recommends the presence of family members in RCP and warns in its latest recommendations of 2015 that only half of European countries allow the presence of family members in these situations 8. Also the American Heart Association (AHA), another important international association in the field of resuscitation, in its latest recommendations of 2015, insists on allowing the presence of relatives 9.
The European Resuscitation Council (ERC), as an international expert organisation in the field of resuscitation, recommends the presence of family members in the RCP and warns in its latest recommendations of 2015 that only half of the European countries allow the presence of family members in these situations 8. Also the American Heart Association (AHA), another important international association in the field of resuscitation, in its latest recommendations of 2015, insists on allowing the presence of relatives 9.
In general, the scientific literature considers that it is a fundamental right to be able to accompany a family member until the end of their life 2,7,8,10. In Spain, Law 41/2002, of 14th November, which is the basic law regulating patient autonomy and rights and obligations in terms of clinical information and documentation, emphasises the right to patient autonomy and decision making by means of the document of prior instructions, which must be taken into account by healthcare professionals in these circumstances. However, in our country we do not have regulations regarding the presence of family members in the case of CRP 11.
A study was carried out that explored programmes oriented towards the participation of relatives in situations of CRA in adults in out-of-hospital settings in order to specify what the mourning of relatives of those who have died from CRA is like, in which cases the presence of relatives should be proposed, what difficulties exist for the implementation of these programmes, what advantages their development has, what are the barriers that professionals contribute to the implementation of these programmes and why these barriers arise.
METHOD
A narrative review of the scientific literature is carried out. The following databases are consulted: Scielo, PubMed, Cuiden and Cochrane Plus and CINAHL. Articles are selected that are 5 years old, in Spanish or English. All those that refer to cardiopulmonary resuscitation (CPR) programmes in the adult population in the out-of-hospital environment are included in the aspects defined in the objective of the study and which define the categories of analysis (The mourning of relatives of people who have died by CPR; Situations in which the presence of relatives can be proposed; Difficulties which exist for the implementation of these programmes; Advantages of programmes with the presence of relatives in out-of-hospital CRA; Barriers which professionals contribute to the implementation of the programmes and Motivation of professionals to present barriers to the programmes); and take into account the presence of relatives. Articles that do not meet the inclusion criteria and grey literature are excluded.
RESULTS
After the bibliographic search in the databases, a total of 896 articles were obtained, which were tabulated in order to be evaluated by both authors. Initially 37 of them were eliminated because they were repeated. Of the remaining 859 articles, 715 were discarded because after reading the summary they either dealt exclusively with CRA in the hospital setting (234), or they only considered CRA in the paediatric patient (460) or they did not provide data related to the objective of the study (19). Of the 144 articles that were selected, 121 were eliminated once they had been read in their entirety, for four reasons: they dealt with CPR only in hospitals (14), they dealt exclusively with CPR in paediatric victims (81), they did not provide information related to the 6 categories of analysis derived from the study objective (26). After this selective process, 23 (Table 2) are the articles finally selected for this review of the scientific literature (Figure 1).
Table 2: Characteristics of the articles included
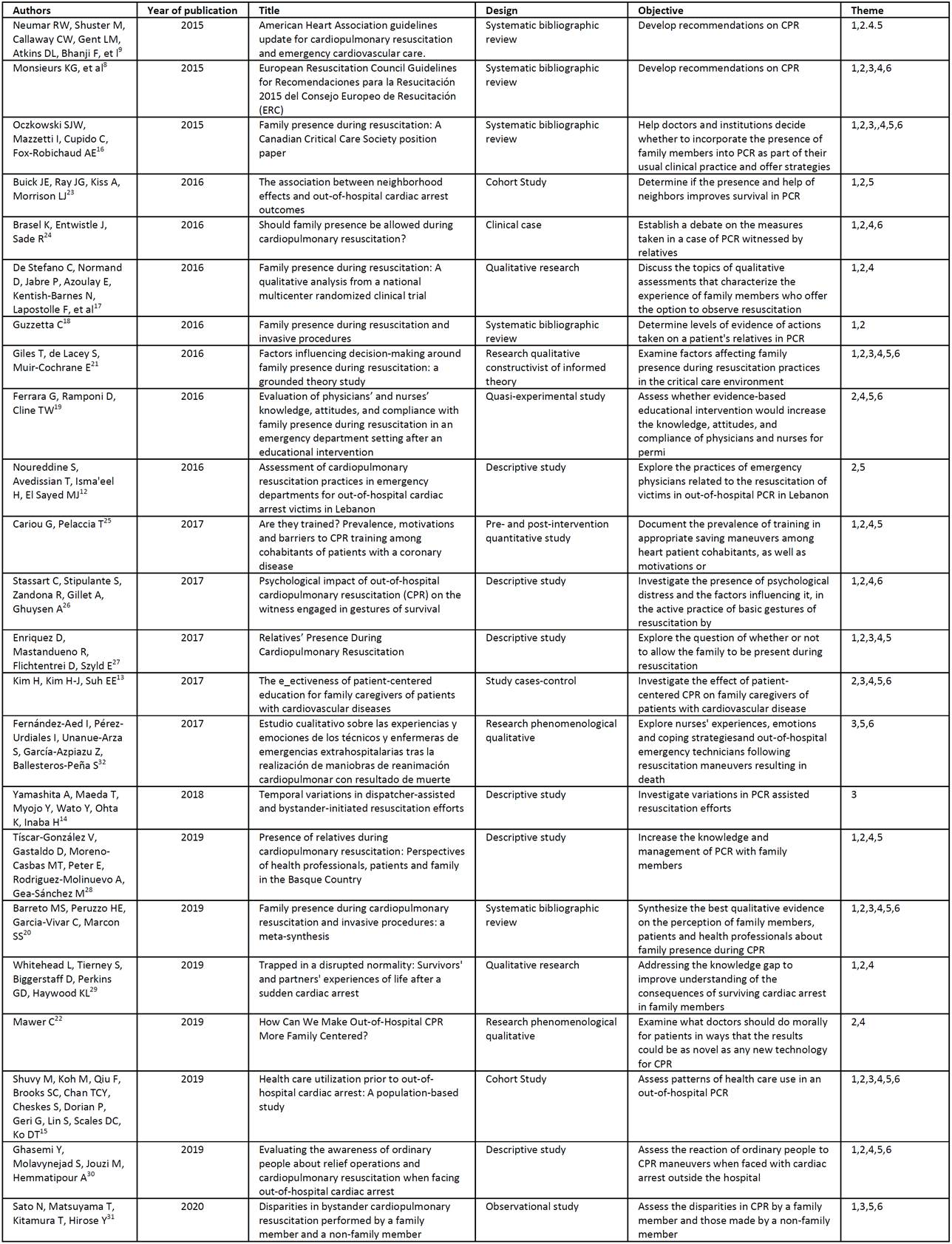
Legend: 1. The mourning of the relatives of those killed by PCR, 2. Situations in which the presence of relatives can be proposed, 3. Difficulties that exist for the implementation of these programmes, 4. Advantages of the programmes for the presence of relatives in out-of-hospital CRA, 5. Barriers that professionals contribute to the implementation of the programmes, 6. Motivation of professionals to present barriers to programmes
CPR=Cardiopulmonary Resuscitation; CPR=Cardiorespiratory Arrest
Categories of analysis of results
Mourning of relatives of adults who have died of CRP in the out-of-hospital setting
The CRP of a loved one has a huge emotional impact on the relatives and if the death occurs, it often generates grief that can be complicated by feelings of guilt 12)(13)(14)(15)(16. Several studies show that the family would have liked to have been present in the process of resuscitation of the deceased and that they believe that their presence could have been useful for the healthcare team 15)(17)(18)(19)(20. Feelings of hopelessness are common in these cases 21)(22)(23. In addition, it has an enormous emotional impact 18)(20)(24)(25)(26)(27.
Those people who were able to be present during the resuscitation of their deceased relative in most cases report that they felt that the help given by the professional team reassured them, understanding that everything possible was done to try and keep their relative alive 8)(15)(18)(28.
In 2001, a group of nurses from the out-of-hospital setting demonstrated that the presence of family members in CRA meant a significant reduction in family anxiety, a feeling that everything possible had been done to save the patient's life, feelings of usefulness, less abrupt disruption of the relationship with the family member and also facilitates mourning 21.
There is evidence of a greater positive effect on intra-family relationships and lower rates of post-traumatic stress and intrusive images if the family member is allowed to accompany them during CPR 16,24.
Situations in which the presence of family members can be proposed and limiting assumptions about the presence of family members in out-of-hospital CPR in the adult
The AHA's recommendations from 2015 indicate that family members should be allowed to be present during CPR at all times, unless this would place excessive stress on CPR personnel or would be considered harmful for any reason 8. In accordance with this recommendation, it does not seem clear in which specific situations the presence of relatives should be allowed 12)(16)(17)(18)(19)(30. Moreover, the decision is taken exclusively by the health team 15)(20)(23)(24)(26)(27)(29.
The limitation that the authors usually find in their studies is the inability to guarantee the safety of the family member or the refusal to do so after offering to collaborate with the intervening team 13)(20)(21)(22)(30, but this does not justify the generalised absence.
Difficulties that exist for the implementation of these programmes
Many studies recommend the collaboration of relatives 13)(14)(15)(16)(28)(30. The most important of these was published in March 2013 in The New England Journal of Medicine (32), but despite this, the reality is quite different, as few out-of-hospital emergency services have programmes for the presence of relatives 8,9.
Health professionals are in some cases reluctant to have family members remain close to the victim because they become nervous and feel pressured (20, 21). In addition, there is a lack of awareness of this issue on the part of public and private administrations 28. It is frequent that both professionals and managers, when faced with new CPR scenarios, are very interested in aspects of the rescue area such as the efficiency of chest compressions and not so much in other aspects of an ethical and social nature 16,27.
Advantages of programmes for the presence of family members in out-of-hospital CPR in adults
Research shows that the presence of a family member can be positive for the team involved as the patient and event information is more accesible 13)(15)(16)(17)(19)(20)(30. Studies different from those mentioned above also show that relatives who have been present at a CPR would make the same decision again 21)(22)(24)(26)(30.
In addition to the advantages mentioned, there is a further advantage which is to comply with the ethical and social need to implement programmes for the presence of relatives in CPR 29. According to the recommendations of the AHA of 2015, ethical aspects should evolve at the same pace as the practice of resuscitation 8. In 2010, both the AHA and the ERC recommended the presence of a family member during CPR as a means of respecting and promoting the autonomy of the patient 8,9, but the reality is quite different, as only half of European countries have implemented such measures 16)(17)(28.
Barriers contributed by professionals to the implementation of programmes for the presence of family members in the case of out-of-hospital CRA in adults
According to Colbert and collaborators (33), it seems that the main barriers to achieving the presence of relatives during CPR manoeuvres are shown by health professionals who believe that the quality of care can be affected, have a false belief that this will generate pathological mourning in the relatives, express fear of legal action and fear of being overburdened in a situation that could require a lot of effort for them. Fear of ethical and legal responsibility is also a barrier 12)(13)(15)(19)(23)(27)(28. Furthermore, there is no tacit agreement that the presence of family members facilitates the interruption of resuscitation manoeuvres or hinders care decisions 30. There are authors who consider that the fear of legal problems in the case of CPR witnessed by relatives is due to the paternalistic practice of current health sciences and that it borders on ethical conflicto 16)(19)(20)(21)(25)(27. Awareness and planning could be the key to overcoming all the barriers mentioned 19.
Despite the above, most health professionals believe that each case should be assessed independently 20.
Motivation of professionals to present barriers to out-of-hospital CRA programmes for adults: sphere of power
Healthcare centres are usually defined as an area of power for healthcare professionals 24, where control is in the hands of those who attend, but this is not the case in the out-of-hospital environment, where on many occasions a response to CRP is given in the patient's home, an environment which is considered in some situations as hostile to and by healthcare professionals 16)(19)(21)(30. This conception of the environment sometimes justifies the non-intervention of the family based on the strengthening of the power or supremacy of the healthcare provider over the patient and his/her family members 13)(15)(20)(28. This attempt not to lose the hierarchy is attributed to the sphere of absolute control that occurs in the paternalistic health model, from which we should move away 20)(28)(30.
DISCUSSION
There is sufficient scientific evidence to recommend the implementation of programmes for the presence of relatives in adult CRA in out-of-hospital settings 7)(8)(10)(13)(18)(19)(20)(21)(22)(29)(30. It is also supported by the recommendations of leading scientific societies in the field of CPR, including AHA and ERC, which are internationally recognised 8,9. However, although the scientific literature shows us a scenario that is conducive to the development of programmes to manage the presence of relatives in the case of out-of-hospital CPR, these programmes hardly exist in Spain 8.
The mourning of relatives is less traumatic and less likely to become pathological if they are allowed to be present 7)(8)(9)(15)(17. A more distant study shows that a small number of relatives admit to having been very shocked by being present at CPR manoeuvres and to having shown shame when they wanted to leave the scene 29.
The situations in which relatives should be allowed to be present in the case of CPR on an adult victim are not at all clear 13, but what most authors agree on is giving people the opportunity to choose whether or not to accompany the victim autonomously 8)(9)(13)(24)(25.
The difficulty in implementing these programmes and which appears relatively frequently in the scientific literature is the lack of motivation of the people who manage the emergency services for these ethical aspects 9)(16)(29. Professionals also represent a barrier in situations where they describe the presence of family members as stressful and even an obstacle to assisting the victim 7)(8)(9)(28)(29)(30. Some research highlights the possibility of fear of the loss of power of the health care providers 29.
The vast majority of the authors present a scenario with many more advantages than disadvantages when it comes to allowing the presence of relatives in the out-of-hospital environment for CPR. According to the scientific literature, these advantages are both for the family members who are better able to mourn and for the professionals who are more satisfied with their care 13)(20)(25)(29)(30.
Finally, it should be pointed out that this research, like all others, has a series of limitations, such as the fact that there is little specific literature on the out-of-hospital environment, especially in the case of adults.
CONCLUSIONS
It can be stated that implementing programmes of this type is important for family members, professionals and managers alike. If relatives are more satisfied with the assistance provided to a family member despite the unfortunate outcome of death, health care providers will be exposed to fewer demands and their job satisfaction will increase. Managers will have satisfied users and professionals who identify more with their professional work and the economic investment for the treatment of pathological mourning will be reduced. Furthermore, this is a social demand and an ethical aspect that should not be left out of the out-of-hospital emergency services.
REFERENCIAS
1. Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, et al. Part 1: Executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015 Oct 20;132(18): S315-67. [ Links ]
2. Monsieurs KG, et al. European Resuscitation Council Guidelines for Recomendaciones para la Resucitación 2015 del Consejo Europeo de Resucitación (ERC) Sección 1: Resumen Ejecutivo[Internet]. [cited 2020 Apr 27]. DOI: 10.1016/j.resuscitation.2015.07.038 [ Links ]
3. Noureddine S, Avedissian T, Isma'eel H, El Sayed MJ. Assessment of cardiopulmonary resuscitation practices in emergency departments for out-of-hospital cardiac arrest victims in Lebanon. J Emerg Trauma Shock [Internet]. 2016 Jul-Sep [cited 2020 May 5];9(3):115-21. DOI: 10.4103/0974-2700.185275 [ Links ]
4. Kim H, Kim H-J, Suh EE. The e_ectiveness of patient-centered education for family caregivers of patients with cardiovascular diseases Presence of relatives during cardiopulmonary resuscitation: Perspectives of health professionals, patients and family in the Basque Country. Journal of cardiop rehabi and prevent [Internet]. 2017 [cited 2020 May 6]; 37(6), 459- DOI: 10.1097/HCR.0000000000000309 [ Links ]
5. Yamashita A, Maeda T, Myojo Y, Wato Y, Ohta K, Inaba H. Temporal variations in dispatcher-assisted and bystander-initiated resuscitation efforts. Am J Emerg Med [Internet]. 2018 [cited 2020 May 6];36(12):2203-2210. DOI: 10.1016/j.ajem.2018.03.080 [ Links ]
6. Shuvy M, Koh M, Qiu F, Brooks SC, Chan TCY, Cheskes S, Dorian P, Geri G, Lin S, Scales DC, Ko DT. Health care utilization prior to out-of-hospital cardiac arrest: A population-based study. Resuscitation [Internet]. 2019 Aug [cited 2020 May 7]; 141:158-165. DOI: 10.1016/j.resuscitation.2019.04.033 [ Links ]
7. Oczkowski SJW, Mazzetti I, Cupido C, Fox-Robichaud AE. Family presence during resuscitation: A Canadian Critical Care Society position paper. Can Respir J [Internte]. 2015 Jul 1 [cited 2020 May 3];22(4):201-5. DOI: 10.1155/2015/532721 [ Links ]
8. De Stefano C, Normand D, Jabre P, Azoulay E, Kentish-Barnes N, Lapostolle F, et al. Family presence during resuscitation: A qualitative analysis from a national multicenter randomized clinical trial. PLoS One [Internet]. 2016 Jun 1 [cited 2020 Apr 30];11(6). DOI: 10.1371/journal.pone.0156100 [ Links ]
9. Guzzetta C. Family presence during resuscitation and invasive procedures. Crit Care Nurse [Internet]. 2016 Feb 1 [cited 2020 May 3];36(1):11-4. DOI: 10.4037/ccn2016980 [ Links ]
10. Ferrara G, Ramponi D, Cline TW. Evaluation of physicians' and nurses' knowledge, attitudes, and compliance with family presence during resuscitation in an emergency department setting after an educational intervention. Adv Emerg Nurs J [Internet]. 2016 Jan 28 [cited 2020 May 4];38(1):32-42. DOI: 10.1097/TME.0000000000000086 [ Links ]
11. Barreto MS, Peruzzo HE, Garcia-Vivar C, Marcon SS. Family presence during cardiopulmonary resuscitation and invasive procedures: a meta-synthesis. Rev Esc Enferm USP [Internet]. 2019 [cited 2020 May 7];53: e03435. DOI: 10.1590/S1980-220X2018001303435 [ Links ]
12. Administración General del Estado. Ley 41/2002, de 14 de noviembre, Básica reguladora de la autonomía del paciente y de derechos y obligaciones en materia de información y documentación clínica. Boletín Oficial del estado (BOE) [Internet]. 2002 [Citado 1 May 2020]; 274: 40126-32. Disponible en: https://boe.es/boe/dias/2002/11/15/pdfs/A40126-40132.pdf [ Links ]
13. Giles T, de Lacey S, Muir-Cochrane E. Factors influencing decision-making around family presence during resuscitation: a grounded theory study. J Adv Nurs [Internet]. 2016 Nov [cited 2020 Apr 30];72(11):2706-17. Available from: http://doi.wiley.com/10.1111/jan.13046 [ Links ]
14. Mawer C. How Can We Make Out-of-Hospital CPR More Family Centered? AMA J Ethics [Internet]. 2019 May 1 [cited 2020 May 5];21(5): E461-469. DOI: 10.1001/amajethics.2019.461 [ Links ]
15. Buick JE, Ray JG, Kiss A, Morrison LJ. The association between neighborhood effects and out-of-hospital cardiac arrest outcomes. Resuscitation [Internet]. 2016 Jun [cited 2020 May 4]; 103:14-19. DOI: 10.1016/j.resuscitation.2016.03.008 [ Links ]
16. Brasel K, Entwistle J, Sade R. Should family presence be allowed during cardiopulmonary resuscitation? An Thorac Surg Ìnternet]. 2016 [cited 2020 May 5];102(5):1438-1443. DOI: 10.1016/j.athoracsur.2016.02.011 [ Links ]
17. Cariou G, Pelaccia T. Are they trained? Prevalence, motivations and barriers to CPR training among cohabitants of patients with a coronary disease. Intern Emerg Med [Internet]. 2017 Sep [cited 2020 May 4];12(6):845-852. DOI: 10.1007/s11739-016-1493-8 [ Links ]
18. Stassart C, Stipulante S, Zandona R, Gillet A, Ghuysen A. Psychological impact of out-of-hospital cardiopulmonary resuscitation (CPR) on the witness engaged in gestures of survival. Rev Med Liege [Internet]. 2017 May [cited 2020 May 6];72(5):236-240. PMID: 28520322 [ Links ]
19. Enriquez D, Mastandueno R, Flichtentrei D, Szyld E. Relatives' Presence During Cardiopulmonary Resuscitation. Glob Heart [Internet]. 2017 [cited 2020 mayo 2;12(4):335-340. DOI: 10.1016/j.gheart.2016.01.007 [ Links ]
20. Tíscar-González V, Gastaldo D, Moreno-Casbas MT, Peter E, Rodriguez-Molinuevo A, Gea-Sánchez M. Presence of relatives during cardiopulmonary resuscitation: Perspectives of health professionals, patients and family in the Basque Country. Aten Primaria [Internet]. 2018 May 1 [cited 2020 May 1];51(5):269-77. DOI: 10.1016/j.aprim.2017.12.002 [ Links ]
21. Whitehead L, Tierney S, Biggerstaff D, Perkins GD, Haywood KL. Trapped in a disrupted normality: Survivors' and partners' experiences of life after a sudden cardiac arrest. Resuscitation [Internet]. 2020 Feb 1 [cited 2020 May 6]; 147:81-87. DOI: 10.1016/j.resuscitation.2019.12.017 [ Links ]
22. Ghasemi Y, Molavynejad S, Jouzi M, Hemmatipour A. Evaluating the awareness of ordinary people about relief operations and cardiopulmonary resuscitation when facing out-of-hospital cardiac arrest. J Family Med Prim Care [Internet]. 2019 Jul [cited 2020 May 6];8(7):2318-2321. DOI: 10.4103/jfmpc.jfmpc_408_19 [ Links ]
23. Sato N, Matsuyama T, Kitamura T, Hirose Y. Disparities in bystander cardiopulmonary resuscitation performed by a family member and a non-family member. J Epidemio [Internet]. 2020 Apr 18 [cited 2020 May 7]. DOI: 10.2188/jea.JE20200068 [ Links ]
24. Fernández-Aed I, Pérez-Urdiales I, Unanue-Arza S, García-Azpiazu Z, Ballesteros-Peña S. Estudio cualitativo sobre las experiencias y emociones de los técnicos y enfermeras de emergencias extrahospitalarias tras la realización de maniobras de reanimación cardiopulmonar con resultado de muerte. Enfermer Intens [Internet]. 2017 [cited 2020 May 7]; 28(2): 57-63. DOI: 10.1016/j.enfi.2016.10.003 [ Links ]
25. Colbert JA, Adler JN. Family presence during cardiopulmonary resuscitation - Polling results. N Engl J Med. 2013;368(26): 38. [ Links ]
26. Jabre P, Belpomme V, Azoulay E, et al. Family presence during cardiopulmonary resuscitation. N Engl J Med [Internet]. 2013 [cited 2020 May 8]; 368:1008-18. DOI: 10.1056/NEJMoa1203366 [ Links ]
27. Leung NY, Chow SK. Attitudes of healthcare staff and patients' family members towards family presence during resuscitation in adult critical care units. J Clin Nurs [Internet]. 2012 [cited 2020 May 5]; 21:2083-93. DOI: 10.1111/j.1365-2702.2011.04013.x [ Links ]
28. Lederman Z, Garasic M, Piperberg M. Family presence during cardiopulmonary resuscitation: Who should decide? J Med Ethics [Internet] 2014 [cited 2020 May 6]; 40:315-9. DOI: 10.1136/medethics-2012-100715 [ Links ]
29. Hung MS, Pang SM. Family presence preference when patients are receiving resuscitation in an accident and emergency department. J Adv Nurs [Internet]. 2010 [cited 2020 May 6]; 67:56-67. DOI: 10.1111/j.1365-2648.2010.05441.x [ Links ]
30. Kosowan S, Jensen L. Family presence during cardiopulmonary resuscitation: Cardiac health care professionals' perspectives. Can J Cardiovasc Nurs [Internet]. 2011 [cited 2020 May 7]; 21:23-9. PMID: 21848046 [ Links ]
Received: September 04, 2020; Accepted: January 13, 2021











 texto en
texto en 




