Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.22 no.72 Murcia oct. 2023 Epub 04-Dic-2023
https://dx.doi.org/10.6018/eglobal.558581
Reviews
Use of scientific evidence in care planning among nursing professionals: a systematic review
1Facultad de Ciencias para el cuidado de la salud, Universidad San Sebastián. Santiago. Chile
Objective:
To determine the use of the available scientific evidence among nursing professionals to plan the provision of care.
Methods:
A search was conducted in the following databases: ProQuest, PubMed, Science Direct, MEDLINE. Nine articles, published between 2011 and 2021 in English and Spanish, were selected for the analysis according to the PRISMA statement.
Results:
The search yielded a result of 356 articles, 9 of which met selection criteria. The included articles do not measure the level of utilization of Evidence-Based Nursing (EBN) for care planning, however, facilitating factors and barriers to its implementation are described.
Conclusion:
The available evidence is not sufficient to determine the utilization of evidence by nursing professionals in the provision of care. Barriers to its utilization, of both personal and organizational nature are described. In order to ensure an adequate implementation of EBN, it is necessary to adopt effective strategies in clinical settings and multidisciplinary efforts need to be made to promote its utilization. It is necessary to conduct higher-quality studies to produce reliable data that demonstrate the role that knowledge, the level of research training and institutional support have on the utilization of EBN in the clinical practice.
Key words: Evidence-based clinical practice; Evidence-based nursing; Clinical nurses; Nursing care
INTRODUCCIÓN
Quality of health care is defined as the application of the best clinical practices in order to achieve patient satisfaction with maximum efficiency (1). Nursing professionals have a relevant impact on quality of health care, since they are involved in most health processes, playing a caring and educational role with patients, but also exercising management and leadership functions in healthcare teams (2). This profession requires nurses to possess their own knowledge based on scientific research, so that society validates their role and trusts that they guarantee quality and security in the care(3,4) provided to the population.
Since the days of Florence Nightingale, an Evidence-Based Practice (EBP) approach has been described, a concept adapted to the profession as Evidence-Based Nursing (EBN) (5,6). However, EBN as a methodology derives from Evidence-Based Medicine (EBM) and originated in the academic world in the United Kingdom, where the first conferences were held in 1997 (6). Moreover, it is important to note that EBM is based mainly on quantitative studies, such as randomized clinical trials; in contrast, experimental research is less frequent in nursing. Therefore, EBN has an intermediate approach that adopts from EBM the aspects that enable a better clinical practice, but maintains its psychosocial approach, since its subject of study is the person and their caring needs (6).
EBN consists of providing health care, integrating the best available scientific evidence, the experience of the clinical nurse and the individual preferences of patients to make the best decisions regarding their health care (7). The implementation of EBN requires to follow a series of steps that consist of translating the information that needs to be known into a structured question that serves as a guide for a rigorous literature search, aimed at finding the last available evidence to answer the question. Subsequently, the results found are critically analyzed and once validated they are applied to clinical practice, to later evaluate their effectiveness (7).
The application of EBN is an opportunity to optimize the quality of the provided care, since it enables the reduction of variability in the practice, the identification of successful interventions for patient care and even the evaluation of strategies to enhance the well-being of nursing professionals (7-9). Nevertheless, it is not easy to implement EBN since it entails the responsibility to stay up to date with research findings and to achieve their integration into the professional practice, where resistance is often found (10). The main criticism made regarding EBN is that it aims to standardize clinical practices, which could interfere in offering an individualized and humane care (11).
Hunt (12), after verifying that research utilization in the nursing practice is minimum, suggested that the reasons for this is that nurses do not know about research findings, do not believe research findings, do not understand them or know how to use them, or are simply not allowed to use research findings. Other authors have identified barriers such as lack of readiness to change, organizational culture that does not encourage innovation, training weaknesses, time constraints or excessive workload, lack of incentives to undergo advanced training and/or participate in research, among others (13-16). On the other hand, however, facilitators have also been described, such as educational strategies, greater access to research, and a growth in the number of partnerships between universities and health institutions (16,17).
Nursing professionals are aware of the importance of using updated scientific knowledge to provide optimal care, however, the use of evidence-based clinical practices is uncommon (18). Furthermore, it has been described that undergraduate training do not succeed in creating interest for research among future nurses (19), which explains to a certain extent the existing gap between the available scientific evidence and its implementation in the nursing practice (17).
In view of the foregoing and to ensure quality of care and patient safety, it is necessary to conduct the present systematic review (SR), with the purpose of determining the utilization of available research by nursing professionals to plan care provision.
METHODS
This study presents a systematic review, which was guided by the following research question: Do clinical nurses use evidence for care planning?
With respect to eligibility criteria, the selected articles were published in the last 10 years and belong to the field of clinical nursing. The type of documents analyzed included Systematic Reviews, Randomized Clinical Trials, qualitative and quantitative primary Scientific papers, whose language was Spanish, English or Portuguese and whose Abstract and Full-Text version were available. Books, book chapters, thesis works, case studies, internet documents and any other type of reference which was not a scientific article were excluded from this review.
To conduct the search of studies, the following equation was used:
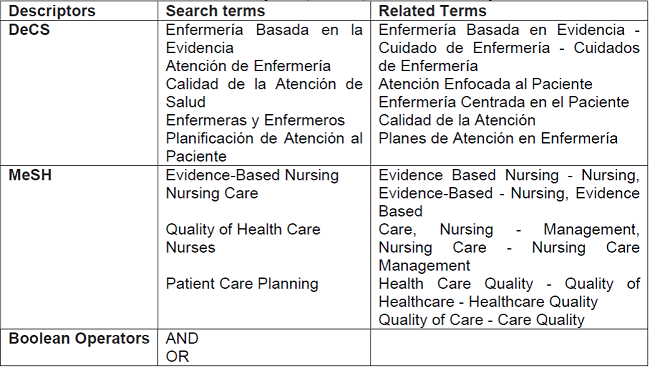
SU (“Evidence-Based Practice” OR “Evidence-based nursing”) AND SU (“clinical nurses” OR “Clinical practice”) AND SU (“Nursing Care Management” OR “Nursing Care”), between years 2011 and 2021. Searched databases included: ProQuest, PubMed, Science Direct and MEDLINE. The search period comprised July 2021. For the elaboration of the search strategy, the Medical Subject Heading (MeSH) descriptors, the Descriptores en Ciencias de la Salud (DeCS) [Descriptors in Health Sciences (DeCS)] and boolean operators were used, which are presented in Table 1:
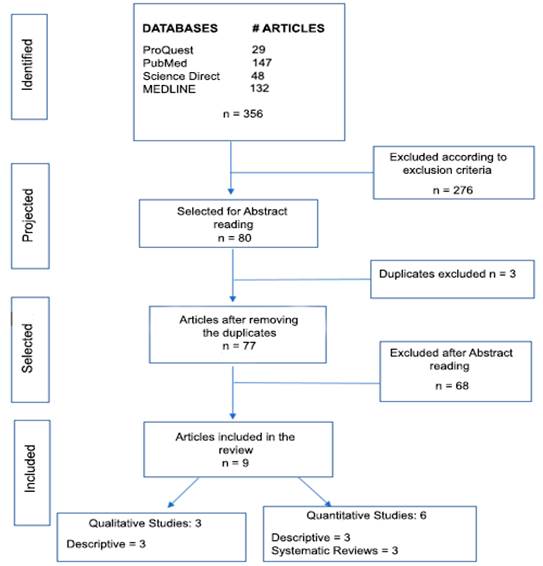
A flowchart was used to select the articles according to the PRISMA statement (Flowchart 1). Firstly, articles published between 2011 and 2021 were selected; later, the titles and abstracts of the articles were analyzed in depth, choosing the relevant articles that met eligibility criteria, to finally perform quality assessment of the selected articles through the CASPe checklist, the STROBE checklist and the Joanna Briggs Institute (JBI) model.
RESULTS
Characteristics of the articles
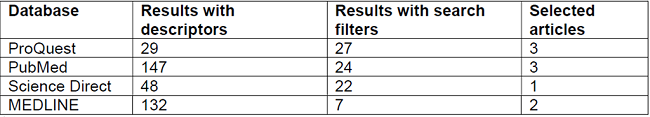
The total number of articles retrieved using the designed search strategy and applying the descriptors was 356; subsequently, filters were applied and 276 articles were excluded, with 80 studies being selected, of which 3 duplicates were eliminated, and after this process 77 abstracts were read. No articles were found that measure the use of EBN, however, 9 articles were included that show factors influencing the implementation of EBN, which were used to perform critical reading.
Source: Prepared by the authors
Flowchart 1. Flow diagram for the selection of articles according to PRISMA.
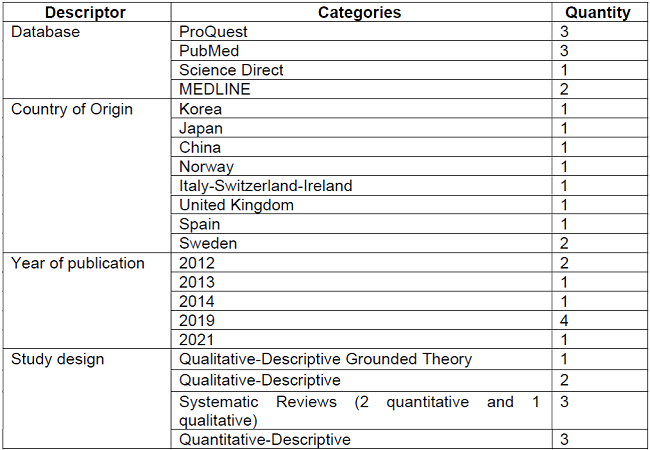
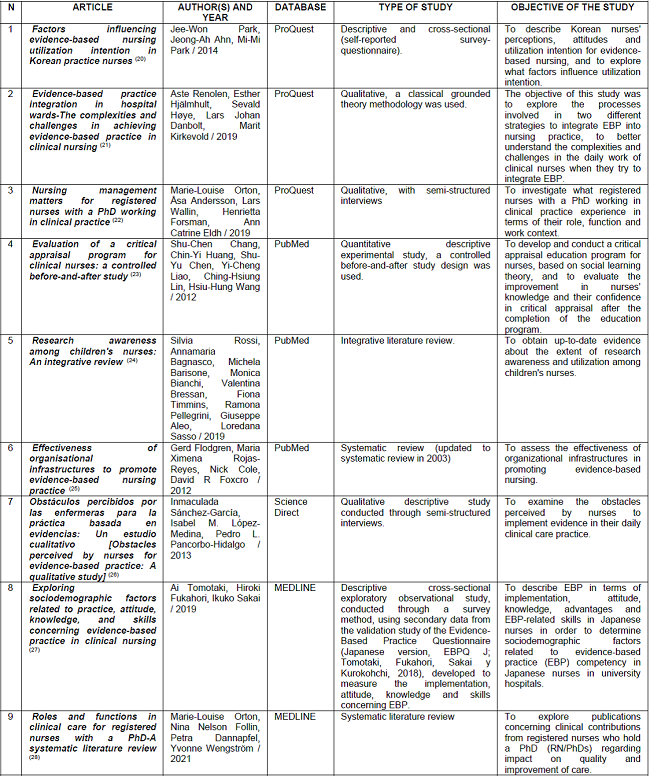
Table 2 describes the database from which each article was obtained.
All of the nine articles selected for the present review were focused on clinical nursing professionals who work in hospital settings in child and/or adult health services and have different levels of professional development, ranging from recently graduated nurses to postgraduate nurses who hold master's or doctoral degrees.
The qualitative-descriptive synthesis of the studies is presented in Table 3.
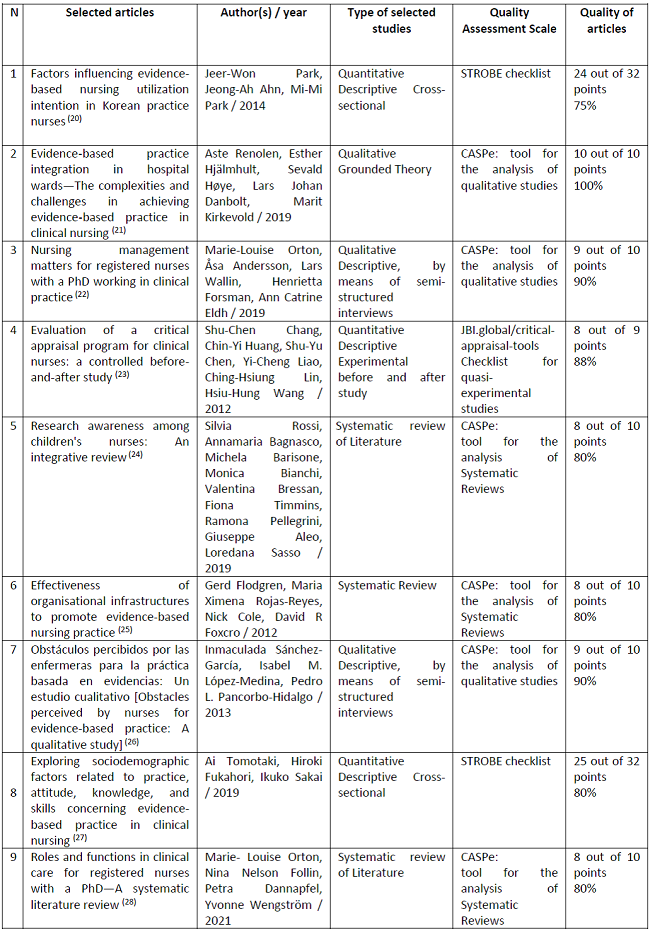
The three Systematic Reviews were subjected to quality assessment using the CASPe guidelines, obtaining rates of 80%; the three qualitative studies were compared against the CASPe guidelines, obtaining rates of 90% and higher; the two quantitative-descriptive studies were applied the STROBE checklist obtaining 75% and 80%, respectively; and, finally, the experimental study was applied the JBI checklist, obtaining 88%. These results are shown in Table 4.
Regarding the utilization of EBN in clinical practice, two articles addressed the importance of academic degrees such as master's and doctoral degrees; three articles established relationships between different influencing factors; two articles described the strategies for the use of EBN; and, finally, one article highlighted the perceived barriers. The descriptions of these studies can be seen in Table 5.
DISCUSSION
The results of this research show that there is no evidence to determine if care planned and performed by nursing professionals is based on scientific evidence, therefore, it is not possible to establish a relationship between evidence-based care and its impact on quality of health care. The aforementioned can be explained by the fact that it is difficult to design studies that achieve an objective measurement of the use of EBN in health care settings. Nevertheless, several studies were found that describe barriers to the implementation of EBN, the most noteworthy being the bureaucracy in the approval of guidelines by physicians and/or managers; time and resources restraints; administrative work overload; training weaknesses; lack of support from organizations; and lack of readiness to change among officials, patients and relatives (26,27). This is in accordance with what have been reported by other authors (12,13,29) and demonstrates the lack of high-level evidence to propose strategies that allow the overcoming of these barriers.
Regarding the facilitating factors described in the reviewed articles, Park et al. (20) described a better perception, attitude and utilization intention for EBN in nurses who held postgraduate qualifications, nurses with more years of experience, nurses who had higher-responsibility jobs, nurses with previous experience in EBN and who experienced a higher level of perceived security and job satisfaction. Similarly, Orton et al. (22) found that the higher the academic degree, the higher the contribution to EBN, due to the nurses' training and the development of clinical research. The aforementioned is in line with what other authors have described (30). Additionally, Shu et al. (23) stated that health institutions that implement EBN education programs targeted at their staff facilitate the overcoming of the commonly mentioned barriers. This enables the identification of the factors that should be borne in mind by health institutions to design strategies that promote the development of EBN.
Among the limitations of this study, it can be mentioned that none of the included articles presented high-level evidence, since they were no randomized, which introduced selection bias.
CONCLUSION
The available evidence is not sufficient to determine the utilization of evidence by nursing professionals in the provision of care. Barriers of personal nature have been described, such as attachment to traditions, training weaknesses, lack of knowledge and time to read and understand research results and to implement them; and other barriers concerning organizational factors in which peer collaboration, perceived usefulness, funding and research culture have an influence on the development of research utilization in the clinical practice.
There is an awareness of the relevance of having thorough knowledge of discipline combined with scientific experience, in order to enhance the quality of care provision, and thereby bridging the existing gap between theory and practice. However, it is important that health organizations keep in mind that there are facilitators for this to occur, which are related to some characteristics of nurses, such as the level of research training, together with a clear description of roles and functions.
In order to ensure an adequate implementation of EBN, it is necessary to adopt effective strategies in clinical settings, one of them being clinical practice guidelines; however, it is crucial to make clear whether or not evidence utilization is a response to an action performed by the institution for accreditation purposes and for enhancing care standards, and not letting it transform into a mechanical action without evaluating the individual needs of each patient. To prevent this to happen, it is required to make multidisciplinary efforts related to EBN training in a sequential, cross-sectional and systematic manner from undergraduate to graduate level. Moreover, it should be noted that job satisfaction favors evidence utilization, and along with support from the organization, can build a research culture and strategies aimed at its implementation.
There is a need to develop methodologically well-designed, minimally biased studies that produce high-level evidence, with the purpose of objectively measuring the level of utilization of EBN, to subsequently test interventions to determine how the implementation of evidence impacts care quality.
REFERENCIAS
1. Urrea Medina E, Retamal Valenzuela M, Tapia Pinto C, Rodríguez Vidal Magaly. Enfermería basada en la evidencia: qué es, sus características y dilemas. Invest educ enferm 2010;28(1):108-18. [ Links ]
2. Mulugeta H, Wagnew F, Dessie G, Biresaw H, Habtewold TD. Patient satisfaction with nursing care in Ethiopia: A systematic review and meta-analysis. BMC Nurs 2019;18(1). [ Links ]
3. Cidoncha-Moreno MA, Garate-Echenique L, Moro-Casuso I, Landaluze-Okerantza G, Martínez-Aramberri I. Implantación de buenas prácticas en cuidados como punto de unión en la integración asistencial. Int J Integr Care 2019;19(4):30. [ Links ]
4. Campos C, Vargas X, Milos P. Los servicios profesionales enfermera(o) en la legislación chilena. Rev. méd. Clín. Las Condes 2018;29(3):270-7. [ Links ]
5. McDonald L. Florence Nightingale and the early origins of evidence-based nursing. Evid Based Nurs. 2001;4(3):68-9. [ Links ]
6. Alcolea M teresa, Oter C, García Á. Enfermería Basada en la evidencia. orígenes y fundamentos para una práctica enfermera basada en la evidencia. NURE inv. 2011;52(1). [ Links ]
7. Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: A guide to best practice. Lippincott Williams & Wilkins; 2022. [ Links ]
8. Connor L, Dean J, McNett M, Tydings DM, Shrout A, Gorsuch PF, et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: Findings from a scoping review. Worldviews Evid Based Nurs. 2023; 20:6-15. [ Links ]
9. Tomietto M, Paro E, Sartori R, Maricchio R, Clarizia L, de Lucia P, et al. Work engagement and perceived work ability: An evidence-based model to enhance nurses' well-being. J Adv Nurs. 2019; 75(9):1933-42. [ Links ]
10. Gomes Pereira RP, Oliveira Cardoso MJ da SP de, Cardoso Martins MAC dos S. Atitudes e barreiras à prática de enfermagem baseada na evidência em contexto comunitário. Revista de Enfermagem Referência. 2012; 3(7):55-62. [ Links ]
11. Cañon H. La práctica de la enfermería basada en evidencia. Investigación en enfermería. 2007; 9(1):101-10. [ Links ]
12. Hunt JM. Barriers to research utilization. J Adv Nurs 1996;23(3):423-5. [ Links ]
13. Hendricks J, Cope V. Research is not a 'scary' word: Registered nurses and the barriers to research utilisation. Nord J Nurs Res 2017;37(1):44-50. [ Links ]
14. Dakka FJ. Nurses Barriers to Evidence-Based Practice in Palliative Care: A Systematic Review. SAGE Open Nurs (Internet) 2022; 8:1-8. Disponible en: https://doi.org/10.1177/23779608221142957 [ Links ]
15. Madhuvu A, Endacott R, Plummer V, Morphet J. Healthcare professional views on barriers to implementation of evidence-based practice in prevention of ventilator-associated events: A qualitative descriptive study. Intensive Crit Care Nurs 2022; 68:1-8. [ Links ]
16. DeBruyn RR, Ochoa-Marín S, Semenic S. Barriers and facilitators to Evidence-Based Nursing in Colombia: perspectives of nurse educators, nurse researchers and graduate students. Invest Educ Enferm 2013;31(3). [ Links ]
17. Hickman LD, DiGiacomo M, Phillips J, Rao A, Newton PJ, Jackson D, et al. Improving evidence based practice in postgraduate nursing programs: A systematic review: Bridging the evidence practice gap (BRIDGE project). Nurse Educ Today. 2018;63:69-75. [ Links ]
18. López-Morales AB, Barrera-Cruz A. Enfermería basada en la evidencia y su aplicación en el plan de cuidados de enfermería Evidence-based nursing and its application in the nursing care plan. Rev Enferm Inst Mex Seguro Soc. 2016;24(3):161-2. [ Links ]
19. Gálvez-Díaz N, Gonzáles-Hernández Y, Monsalve-Menor M. Actitud hacia la investigación científica al final de la carrera de Enfermería en Perú. Gac Med Bol. 2019;42(1). [ Links ]
20. Park JW, Ahn JA, Park MM. Factors influencing evidence-based nursing utilization intention in Korean practice nurses. Int J Nurs Pract. 2015;21(6):868-75. [ Links ]
21. Renolen Å, Hjälmhult E, Høye S, Danbolt LJ, Kirkevold M. Evidence-based practice integration in hospital wards-The complexities and challenges in achieving evidence-based practice in clinical nursing. Nurs Open. 2019;6(3):815-23. [ Links ]
22. Orton ML, Andersson Å, Wallin L, Forsman H, Eldh AC. Nursing management matters for registered nurses with a PhD working in clinical practice. J Nurs Manag. 2019;27(5):955-62. [ Links ]
23. Shu-Chen C, Chin-Yi H, Shu-Yu C, Yi-Cheng L, Ching-Hsiung L, Hsiu-Hung W. Evaluation of a Critical Appraisal Program for Clinical Nurses: A Controlled Before-and-After Study. J Contin Educ Nurs. (Internet) 2013; 44(1):43-8. Disponible en: https://doi.org/10.3928/00220124-20121101-51 [ Links ]
24. Rossi S, Bagnasco A, Barisone M, Bianchi M, Bressan V, Timmins F, et al. Research awareness among children's nurses: An integrative review. J Clin Nurs. 2020;29(3-4):290-304. [ Links ]
25. Flodgren G, Rojas-Reyes MX, Cole N, Foxcroft DR. Effectiveness of organisational infrastructures to promote evidence-based nursing practice. Cochrane Database of Systematic Reviews. 2012;(2). [ Links ]
26. Sánchez-García I, López-Medina IM, Pancorbo-Hidalgo PL. Obstáculos percibidos por las enfermeras para la práctica basada en evidencias: Un estudio cualitativo. Enferm Clin. 2013;23(6):279-83. [ Links ]
27. Tomotaki A, Fukahori H, Sakai I. Exploring sociodemographic factors related to practice, attitude, knowledge, and skills concerning evidence-based practice in clinical nursing. Jpn J Nurs Sci. 2020;17(1). [ Links ]
28. Orton ML, Nelson Follin N, Dannapfel P, Wengström Y. Roles and functions in clinical care for registered nurses with a PhD-A systematic literature review. Scand J Caring Sci. 2022;36(1):16-26. [ Links ]
29. Williams B, Perillo S, Brown T. What are the factors of organisational culture in health care settings that act as barriers to the implementation of evidence-based practice? A scoping review. Nurse Educ Today. 2015;35(2):34-41. [ Links ]
30. Baird LMG, Miller T. Factors influencing evidence-based practice for community nurses. Br J Community Nurs. 2015;20(5):233-42. [ Links ]
Received: February 27, 2023; Accepted: April 18, 2023











 texto en
texto en