Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.23 no.73 Murcia ene. 2024 Epub 23-Feb-2024
https://dx.doi.org/10.6018/eglobal.573161
Originals
Working conditions and mental health indicators in medical and nursing professionals in Chile during the COVID-19 pandemic
1Pueblo Nuevo Community Mental Health Center, Temuco, Chile
2Department of Mental Health and Psychiatry, Faculty of Medicine, Universidad de La Frontera, Temuco, Chile
3Department of Psychology, Faculty of Education, Social Sciences and Humanities, Universidad de La Frontera, Temuco, Chile
4Laboratory of Cognition, Aging and Health. Doctorate in Psychology, Faculty of Education, Social Sciences and Humanities, Universidad de La Frontera, Temuco, Chile
Background:
The mental health of health personnel was affected by the SARS-CoV-2 pandemic and its associated consequences, including the change in working conditions.
Results:
Nursing staff reported greater depressive, anxiety, and insomnia symptomatology. In turn, they manifested greater indicators of depression in interaction with the change in workday (F (1,86) = 3.83, p= 0.05, partial η² = 0.04) and work shift (F (1,86) = 6.80, p= 0. 01, partial η² = 0.07); greater anxious symptomatology in interaction with change in workday (F (1,86) = 5.83, p= 0.02, partial η² = 0.06) and work shift (F (1,86) = 9.26, p= 0.003, partial η² = 0.10). Additionally, more indicators of insomnia in interaction with being on the front line (F (1,86) = 4.96, p = 0.04, partial η²= 0.05) and changes in working hours (F (1,86) = 3.88, p = 0.05, partial η²= 0.04).
Conclusion:
The nursing staff was more affected by changes in working conditions, having more symptoms of anxiety, depression, and insomnia.
Keywords: Mental health; depression; anxiety; insomnia; SARS-CoV-2; health workers; working conditions
INTRODUCTION
The COVID-19 pandemic associated with the SARS-CoV-2 virus was one of the events of the greatest psychological impact in recent decades. The speed with which the disease propagated is relevant: the first cases in Wuhan (China) were reported in December 2019, and by March 2020, a worldwide pandemic had been declared (1).
In this regard, there was an early warning about the effect this scenario could have on people's mental health, considering there were risk factors related to economic and social vulnerability before the pandemic. It was foreseeable that these would be exacerbated by such measures as border closures, quarantine, and social distancing, thus triggering increases in the rates of violence, depression, suicides, and substance abuse (2). This was evidenced in one of the first exploratory studies published on the psychosocial impact of social isolation in Santiago, Chile, which reported rates of worry and anxiety that reached 67% and 60%, respectively (3).
In this light, health professionals are particularly vulnerable to developing adverse indicators of poor mental health. Several factors can explain this; however, the leading causes include job demands, a higher risk of contagion for themselves and their families, and in those settings where resources were scarce, they constantly faced ethical dilemmas (4). In this sense, among the available scientific evidence, three systematic literature reviews stand out for their methodological quality(5,6,7). The common points of these works are, first, considering the variables of depression, anxiety, and insomnia as mental health indicators; second, they emphasize the existence of sociodemographic variables (e.g., sex) and the working environment (e.g., profession) that end up as predispositions for a greater manifestation of symptoms.
Previous studies have emphasized that working conditions, such as being on the front line, i.e., being in direct contact with infected patients, can cause major psychological distress (8). In the Latin American context, transcultural studies compared the depression and anxiety levels of health professionals in different countries. The report by Abeldaño et al. (9) was particularly relevant to this study, which revealed that health professionals in Chile presented higher anxiety scores than in Argentina, Colombia, and Mexico. Additionally, the studies conducted solely in Chile show a high prevalence of depression, anxiety, and insomnia symptoms in health personnel (10,11,12).
The available literature to date has focused predominantly on the differences by profession and being on the front line; however, the interaction among these factors has been less explored. At the same time, there is little evidence of the impact of workload and changes in the routine of health personnel compared to their pre-pandemic dynamics, which is particularly relevant for those with a sedentary routine (5).
Given the theoretical and empirical background and considering the lack of evidence in the Latin American context concerning the interaction of sociodemographic elements in health personnel, this study sought to determine the relationship between mental health indicators and socio-professional factors in a sample of medical and nursing professionals in southern Chile.
MATERIALS AND METHODS
Participants
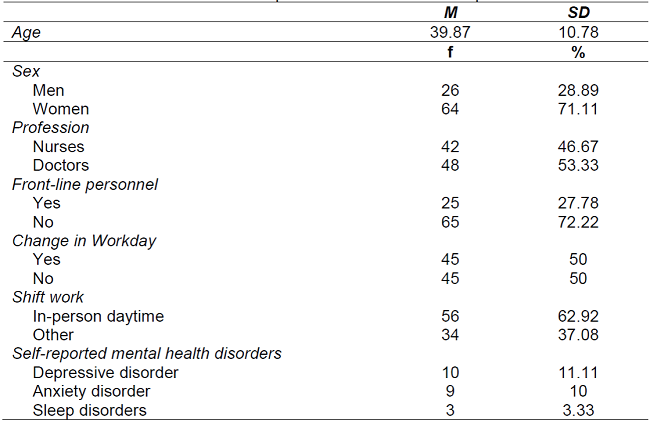
The sample was initially comprised of 112 professionals. The inclusion criteria were: working in health, specifically doctors and nurses, who could answer the survey digitally way and who participated voluntarily. Also, as an exclusion criterion for this study, participants could not have been off sick or on medical leave since the beginning of the pandemic; therefore, a total of 22 participants were excluded from the study. Consequently, the final sample contained 90 health professionals, 71% women, and 53% doctors with an average age of 39 years (see Table 1). The sample size was considered adequate when the statistical power required to detect a moderate effect size in the most robust analysis (2 x 2 factorial ANOVA) was taken into account, with a type I error probability of 5%, obtaining a total size of at least 84 individuals for a power of 95% and a critical F of 3.96; this estimation was done using the G Power software.
Variables and instruments
Depressive symptomatology: This was measured using the Spanish version of the Patient Health Questionnaire in its 9-question version (PHQ-9) (13), validated in Chile (14),(15). It evaluated the presence and frequency of depressive symptomatology in the last two weeks using a response scale from 0 to 3 points (0= never, 3= almost every day) and has suitable internal consistency (⍺ = 0.87).
Anxiety symptomatology: This was measured using the Generalized Anxiety Disorder (GAD-7) scale in its Spanish version (16). With this test, anxiety symptoms in the last two weeks were evaluated on a scale from 0 to 3 points (0=never and 3=almost every day), with excellent indicators of internal consistency (⍺ = 0.92).
Insomnia: Measured using the Spanish version of the Insomnia Severity Index (ISI-3) (17), this instrument assessed the severity of insomnia perceived on a 5-point Likert scale to evaluate each element (0= no problem and 4= very severe problem). This questionnaire showed excellent levels of internal consistency (⍺ = 0.91)
Procedure
The data were collected by applying an online, self-administered questionnaire to doctors and nurses in a hospital in the Araucanía Region, with voluntary participation and prior acceptance of the letter of informed consent approved by the Araucanía Sur Health Service ethics committee. The questionnaire was applied in September 2020, and those professionals who reported having been on medical leave before answering the first survey were excluded from the final sample.
RESULTS
First, the descriptive statistics were calculated for the sociodemographic variables of the sample, and the working conditions were analyzed. Women were in the majority (71.11%), with an average age of 39.87 years. Most participants were medical personnel (46.67%), did not work on the front line (72.22%), and had a daytime work schedule (62.92%). Regarding the change in workday, half of the sample reported working on a different shift from before the pandemic. In addition, 24.44% of the sample reported having presented mental health disorders before.
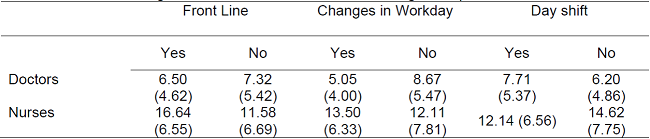
When analyzing the interaction between profession and being in the front line of care for depressive symptomatology scores, no significant interaction was obtained (F (1,86) = 0.34, p= 0.56). The main effects reveal a significant effect was found only for the variable profession (F (1,86) = 19.36, p= 0.001, η² partial= 0.18), which in terms of the marginal means, indicates that nurses have higher scores (M= 12.55 ± 0.86) than doctors (M= 7.48 ± 0.77). The results of the analysis of variance, which include the inter-subject factors profession and change in workday, pointed to a significant interaction effect between the two variables (F (1,86) = 3.83, p= 0.05, η² partial= 0.04). In this sense, an analysis of the marginal means (see Table 2) reveals that being nursing staff and having had a change in workday leads to significantly higher scores in the depression measurement. Finally, when analyzing the profession and the type of workday, a significant interaction (F (1,86) = 6.80, p= 0.01, η was obtained ² partial = 0.07); when analyzing the marginal means, being a nurse and working a shift other than daytime leads to higher scores on the depression measurement.
Table 2. Averages of PHQ-7 test scores when combining socio-professional factors.
Note:Standard deviation in parentheses.
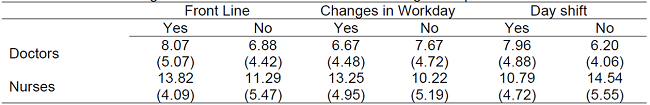
Regarding the GAD-7 anxiety scale scores, no significant interaction was obtained between the profession and being on the front line (F (1,86) = 0,20, p =0.66). When the main effects were analyzed, a significant effect was found only for the variable profession (F (1,86) = 30.05, p= 0.001, η² partial= 0.26), which in light of the marginal means, indicates that nurses have higher scores (M= 10,47 ± 5,01) than doctors (M= 5.02 ± 3.40). When profession and change in a workday are included as inter-subject factors, there is a significant interaction effect between the two variables (F(1,86) = 5.83, p= 0.02, η² partial= 0.06). When analyzing the marginal means, it is observed that being nursing staff and having a change in workday leads to higher anxiety scores. Moreover, a significant interaction was obtained between profession and type of workday, (F (1,86) = 9.26, p= 0.003, η² partial = 0.10) from the analysis of the marginal means (see Table 3). It is concluded that being part of the nursing staff and working a schedule other than the day shift leads to higher scores in the anxiety measurement.
Table 3. Averages of GDA-7 test scores when combining socio-professional factors.
Note:Standard deviation in parentheses.
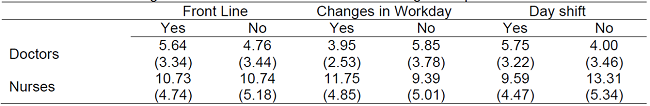
The analysis of variable insomnia, including profession and being on the front line as factors, obtained a significant interaction between the two variables (F (1,86) = 4.40, p = 0.04, η² partial= 0.05). The marginal means (Table 4) show that being a nurse combined with being on the front line of care of patients with COVID-19 results in greater insomnia-related symptomatology. A significant effect of interaction between profession and change in workday was identified (F (1,86) = 3.88, p = 0.052, η² partial= 0.04), which, when visualizing the marginal means, reflects that being part of the nursing staff and having had changes in workday leads to more significant insomnia issues. There was no interaction effect when profession and work schedule were included as fixed factors (F (1,86) = 2.21, p = 0.14). Only one main effect was found for the variable profession, with sleep disturbances being greater for the nursing staff (M = 12.90 ± 6.95) than for the medical staff (M = 7.08 ± 5.17).
DISCUSSION
This study aimed to determine the relationship between mental health indicators and socio-occupational factors in medical and nursing personnel in Chile. The results obtained show that nursing staff consistently reported more depressive symptoms, anxiety, and sleep disturbances than medical staff. It is known that the presence of these symptoms not only affects mental health and work performance but is also a risk factor for the development of psychiatric morbidity in the future(18). This higher prevalence may be due at least in part to gender-related factors, as previous studies have reported that a considerable percentage of nursing staff are women, who also report higher levels of discrimination (11).
This creates a complex scenario for nursing staff, given the nature of their work, where there is greater exposure to biological risk factors as well as elements that threaten psychosocial stability(19,20). In this respect, several studies have concluded that the COVID-19 pandemic has caused greater vulnerability among health personnel, being affected by different stressors in their place of work, primarily the responsibility of providing care and treatment (21).
The change in workday in the context of the COVID-19 pandemic and having a different shift from the daytime schedule also affected the nursing staff more. The convergence of these elements resulted specifically in the report of greater anxiety symptomatology. This result is consistent with several previous studies that describe high levels of anxiety in nursing personnel, even higher than depressive symptomatology (22,23,24,25,26). The global pandemic context has generated circumstances of uncertainty, work overload, and a greater perception of risk associated with contagion in the general population and particular health personnel (27). This scenario could be the cause of the symptoms reported by those who participated in this study.
This study has some limitations. Therefore, the results must be interpreted with caution, considering the specific features of this sample. It is also important to note that the instruments used in this study do not constitute a diagnosis since they evaluate the presence of a group of symptoms and cannot replace an assessment by mental health professionals. Moreover, according to the DSM-5 diagnostic criteria, temporality is a component to determine the intensity of symptomatology. Given that the minimal temporality for the intensity threshold in the conditions reported is over three months, it is suggested that the time between measurements be increased in future studies.
Nevertheless, the present study is a valuable contribution to understanding how work-related aspects can influence the mental well-being of health workers. It also opens the possibility that future research may identify protective factors against the development of mental health disorders in health workers, mainly because there is evidence that variables such as social support (28) and dispositional optimism can help people reduce the impact of negative feelings and make possible the development of healthier coping strategies or increase the willingness to seek psychological help where depressive or anxiety symptoms are present (29). Finally, it is recommended that health institutions guarantee working conditions consistent with the prevention of mental health disorders and increase the supply of psychosocial support services to promote the well-being of health personnel (30).
CONCLUSIONS
The results obtained make it possible to conclude that during the COVID-19 pandemic, the nursing staff presented a greater negative affective response than the rest of the health personnel, which was also intensified by the changes in working conditions, such as shift changes and the extension of working hours. This poses a challenge for institutions and management and well-being teams to follow up with these employees, given the consequences of excessive exposure to stressful events like those that occurred during the pandemic.
REFERENCIAS
1. Cañete Villafranca R, Noda Albelo A, Ferreira Moreno V, Brito Pérez K, García Herrera A. SARS-Cov-2, el virus emergente que causa la pandemia de COVID-19. Rev Med Electron 2020; 42 (3): 1862-81. http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1684-18242020000301862#:~:text=El%20diagn%C3%B3stico%20de%20infecci%C3%B3n%20por,ya%20que%20ofrecen%20mayor%20sensibilidad. [ Links ]
2. Caqueo-Urízar A, Urzúa A, Aragón-Caqueo D, Charles C, El-Khatib Z, Otu A, Yaya S. Mental health and the COVID-19 pandemic in Chile. Psychol Trauma 2020; 12 (5): 521. https://doi.org/10.1037/tra0000753. [ Links ]
3. Dagnino P, Anguita V, Escobar K, Cifuentes S. Psychological effects of social isolation due to quarantine in chile: an exploratory study. Front Psychiatry 2020; 11. https://doi.org/10.3389/fpsyt.2020.591142. [ Links ]
4. Khajuria A, Tomaszewski W, Liu Z, Chen J-h, Mehdian R, Fleming S, Vig S, Crawford M. Workplace factors associated with mental health of healthcare workers during the COVID-19 pandemic: an international cross-sectional study. BMC Health Serv Res 2021; 21 (1): 1-11. https://doi.org/10.1186/s12913-021-06279-6. [ Links ]
5. Tolsa M, Malas O. COVID-19: Impacto Psicológico, Factores de Riesgo e Intervenciones Psicológicas en el Personal Sanitario. Una Revisión Sistemática. Revista Iberoamericana de Psicología y Salud 2021; 12 (2): 58-75. https://doi.org/10.23923/j.rips.2021.01.045. [ Links ]
6. Pappa S, Ntella V, Giannakas T, Giannakoulis V, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun 2020; 88: 901-7. https://doi.org/10.1016/j.bbi.2020.05.026. [ Links ]
7. Batalla-Martín D, Campoverde K, Broncano-Bolzoni M. El impacto en la salud mental de los profesionales sanitarios durante la COVID-19. Rev Enferm Salud Ment 2020; 16: 17-25. https://doi.org/10.5538/2385-703X.2020.16.17. [ Links ]
8. Danet A. Impacto psicológico del COVID-19 en profesionales sanitarios de primera línea en el ámbito occidental. Una revisión sistemática. Med Clin (Barc) 2021; 156 (9): 449-58. https://doi.org/10.1016%2Fj.medcli.2020.11.009. [ Links ]
9. Abeldaño Zuñiga RA, Juanillo-Maluenda H, Sánchez-Bandala MA, Burgos GV, Müller SA, Rodríguez López JR. Mental Health Burden of the COVID-19 Pandemic in Healthcare Workers in Four Latin American Countries. Inq (United States). 2021;58:1-9. https://doi.org/10.1177/00469580211061059. [ Links ]
10. Olivares-Tirado P, Zanga-Pizarro R. Impact of COVID-19 pandemic outbreak on mental health of the hospital front-line healthcare workers in Chile: a difference-in-differences approach. J Public Health. 2023;45(1):57-64. https://doi.org/10.1093/pubmed/fdac008. [ Links ]
11. Alvarado R, Ramírez J, Cortés M, Aguirre J, Bedregal P, Allel K, et al. El impacto de la pandemia de COVID-19 en la salud mental de los trabajadores de la salud en Chile: datos iniciales de The Health Care Workers Study. Rev Med Chil. 2021;149(8):1205-14. http://dx.doi.org/10.4067/s0034-98872021000801205. [ Links ]
12. Urzúa A, Samaniego A, Caqueo-Urízar A, Zapata Pizarro A, Irarrázaval Domínguez M. Salud mental en trabajadores de la salud durante la pandemia por COVID-19 en Chile. 2020; Rev Med Chile 148 (8): 1121-7. http://dx.doi.org/10.4067/S0034-98872020000801121. [ Links ]
13. Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer R. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med 2001; 63 (4): 679-86. https://doi.org/10.1097/00006842-200107000-00021. [ Links ]
14. Baader T, Molina J, Venezian S, Rojas C, Farías R, Fierro-Freixenet C, Backenstrass M, Mundt C. Validación y utilidad de la encuesta PHQ-9 (Patient Health Questionnaire) en el diagnóstico de depresión en pacientes usuarios de atención primaria en Chile. Rev Chil Neuro-Psiquiat 2012; 50 (1): 10-22. http://dx.doi.org/10.4067/S0717-92272012000100002. [ Links ]
15. Saldivia S, Aslan J, Cova F, Vicente B, Inostroza C, Rincón P. Propiedades psicométricas del PHQ-9 (Patient Health Questionnaire) en centros de atención primaria de Chile. Rev Med Chile 2019; 147(1): 53-60. http://dx.doi.org/10.4067/S0034-98872019000100053. [ Links ]
16. García-Campayo J, Zamorano E, Ruiz M, Pardo A, Pérez-Páramo M, López-Gómez V, Freire O, Rejas J. Cultural adaptation into Spanish of the generalized anxiety disorder-7 (GAD-7) scale as a screening tool. Health Qual Life Outcomes 2010; 8 (1):1-11. https://doi.org/10.1186/1477-7525-8-8. [ Links ]
17. Bastien C, Vallières A, Morin C. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med 2001; 2 (4): 297-307. https://doi.org/10.1016/s1389-9457(00)00065-4. [ Links ]
18. Gupta A, Mehra A, Niraula A, Kafle K, Deo S, Singh B, Sahoo S, Grover S. Prevalence of anxiety and depression among the healthcare workers in Nepal during the COVID-19 pandemic. Asian J Psychiatr 2020; 54: 102260. https://doi.org/10.1016%2Fj.ajp.2020.102260. [ Links ]
19. Lopez V. Nurses at the forefront of COVID-19 pandemic. NPT. 2020;8(1):1-3. https://doi.org/10.18502/npt.v8i1.4485. [ Links ]
20. Lozano-Vargas A. Impacto de la epidemia del Coronavirus (COVID-19) en la salud mental del personal de salud y en la población general de China. Rev Neuropsiquiatr [Internet]. 2020. http://dx.doi.org/10.20453/rnp.v83i1.3687. [ Links ]
21. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, Rasoulpoor S, Khaledi-Paveh B. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health 2020;16 (1):57. https://doi.org/10.1186/s12992-020-00589-w. [ Links ]
22. Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res 2020; 290: 113129. https://doi.org/10.1016%2Fj.psychres.2020.113129. [ Links ]
23. de Pinho LG, Sampaio F, Sequeira C, Teixeira L, Fonseca C, Lopes M. Portuguese nurses' stress, anxiety, and depression reduction strategies during the covid-19 outbreak. Int J Environ Res Public Health 2021; 18 (7): 3490. https://doi.org/10.3390/ijerph18073490. [ Links ]
24. Luceño-Moreno L, Talavera-Velasco B, García-Albuerne Y, Martín-García J. Symptoms of posttraumatic stress, anxiety, depression, levels of resilience and burnout in Spanish health personnel during the COVID-19 pandemic. Int J Environ Res Public Health 2020; 17 (15): 5514. https://doi.org/10.3390/ijerph17155514. [ Links ]
25. Obando Zegarra R, Arévalo-Ipanaqué JM, Aliaga Sánchez RA, Obando Zegarra M. Ansiedad, estrés y depresión en enfermeros de emergencia Covid-19. Index Enferm 2020; 29 (4): 225-9. http://ciberindex.com/index.php/ie/article/view/e13056. [ Links ]
26. Shen X, Zou X, Zhong X, Yan J, Li L. Psychological stress of ICU nurses in the time of COVID-19. Crit Care 2020; 24 (1): 200. https://doi.org/10.1186/s13054-020-02926-2. [ Links ]
27. Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J Psychosom Res 2020: 110343. https://doi.org/10.1016/j.jpsychores.2020.110343. [ Links ]
28. Romero C, Delgado C, Catalá J, Ferrer C, Errando C, Iftimi A, Benito A, de Andrés J, Otero M. COVID-19 psychological impact in 3109 healthcare workers in Spain: The PSIMCOV group. Psychol Med 2020:1-7. https://doi.org/10.1017/s0033291720001671. [ Links ]
29. Shechter A, Diaz F, Moise N, Anstey D, Ye S, Agarwal S, Birk J, Brodie D, Cannone D, Chang B, Claassen J, Cornelius T, Derby L, Dong M, Givens R, Hochman B, Homma S, Kronish I, Lee S, Manzano W, Mayer L, McMurry C, Moitra V, Pham P, Rabbani L, Rivera R, Schwartz A, Schwartz J, Shapiro P, Shaw K, Sullivan A, Vose C, Wasson L, Edmondson D, Abdalla M. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry 220; 66: 1-8. https://doi.org/10.1016/j.genhosppsych.2020.06.007. [ Links ]
30. World Health Organization. Coronavirus disease (COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health: interim guidance, 19 March 2020. World Health Organization; 2020. https://apps.who.int/iris/handle/10665/331510. [ Links ]
Received: June 11, 2023; Accepted: August 14, 2023











 texto en
texto en