Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.1 ene./feb. 2006
ORAL SURGERY
Treatment of temporomandibular joint ankylosis by gap arthroplasty
Belmiro Cavalcanti do Egito Vasconcelos 1, Ricardo Viana Bessa-Nogueira 2, Rafael Vago Cypriano 3
(1) Profesor Adjunto de la asignatura de Cirugía bucal y maxilofacial. Director del Programa de Master y
Doctorado en Odontología (Cirugía bucal y maxilofacial)
(2) Alumno del Master en Odontología (Cirugía bucal y maxilofacial)
(3) Alumno del Curso de Especialización en Cirugía bucal y maxilofacial. Facultad de Odontología de Pernambuco.
Universidad de Pernambuco Brasil
ABSTRACT
Purpose: The purpose of this paper is to show that gap arthroplasty
improve mouth opening when treating TMJ ankylosis.
Patients and methods: Eight patients with TMJ ankylosis were treated by gap
arthroplasty. The patients were evaluated by at least twenty-four months (minimum
24 and maximum 48 months).
Results: Of the eight patients (eleven joints), five (62.5%) had unilateral
involvement and three patients (37.5%) had bilateral involvement. The mean age
was 20 years ± 9 (range 3 to 30 years). The mean maximal incisal opening (MIO)
in the preoperative period was 9.25 ± 6.41 mm and in the postoperative period
it was 29.88± 4.16 mm. The complication of temporary facial nerve paresis was
encountered in two patients (25%). No recurrence was observed in our series.
Conclusions: Trauma was the major cause of tempomandibular joint ankylosis
in our sample. Gap arthroplasty showed good results when treating TMJ ankylosis.
Key words: Temporomandibular joint disorders, ankylosis, arthroplasty.
RESUMEN
Objetivo: El propósito de este trabajo es mostrar que la artroplastia
simple mejora la apertura bucal al tratar la anquilosis temporomandibular.
Pacientes y métodos: Fueron tratados ocho pacientes con anquilosis de la
articulación temporomandibular por medio de artroplastia simple. Los pacientes
fueron evaluados en el postoperatorio por un periodo por lo menos de
veinticuatro meses (mínimo 24 y máximo 48 meses).
Resultados: De los ocho pacientes (once articulaciones), cinco (62,5%)
presentaron afectación unilateral y tres pacientes (37.5%) afectación
bilateral de la ATM. La edad media fue de 20 años ± 9 (rango de 3 a 30 años).
La máxima apertura bucal en el período preoperatorio fue de 9,25 ± 6,41 mm,
mientras en el período postoperatorio fue de 29,88 ± 4,16 mm (p = 0.011). Se
observó parálisis del nervio facial en dos pacientes (25%) la cual fue de carácter
temporal. No se observó ninguna recurrencia en nuestra serie.
Conclusiones: El trauma fue la mayor causa de la anquilosis tempomandibular
en nuestra muestra. La artroplastia simple mostró buenos resultados para el
tratamiento de la anquilosis de la ATM.
Palabras clave: Articulación temporomandibular, anquilosis, cirugía.
Introduction
Temporomandibular joint (TMJ) ankylosis is a disorder that leads to a restriction of the mouth opening from partial reduction to complete immobility of the jaw. It is most commonly associated with trauma (13% to 100%), local or systemic infection (0% to 53%), or systemic disease, such as ankylosing spondylitis, rheumatoid arthrits, or psoriasis.(1,2)
TMJ ankylosis may be classified by a combination of location (intra- or extra-articular), type of tissue involved (bony, fibrous, or fibro-osseus) and extent of fusion (complete, incomplete).(3) Literature classifies ankylosis as true and false. Any condition that gives rise to osseous or fibrous adhesion between the surfaces of the temporo-mandibular joint is a true ankylosis. False ankylosis results from pathologic conditions not directly related to the joint.(1,4)
The TMJ ankylosis is a extremely disabling affliction that causes problems in mastication, digestion, speech, appearance, and hygiene.(5) In growing patients, deformities of the mandible and maxilla may occur together with malocclusion.(6,7)
There are no consensous in the existing literature of the best treatment for TMJ ankylosis. Several authors studied and developed different techniques, but reccurence still remains the major problem when treating TMJ ankylosis.(1,2,5,8-11)
Inadequate exposure of the TMJ region for not to know on the adjacent structures (facial nerve, carotid, jugular and maxillary vessels) often leads to insufficient removal of the ankylotic bone, thus leading to a recurrence of the problem. (3,7)
The purpose of this paper is to show that gap arthroplasty improve mouth opening when treating TMJ ankylosis.
Material and Methods
Eight patients (eleven TMJs) with TMJ ankylosis were treated at the departament of oral and maxillofacial surgery at Oswaldo Cruz Hospital. All patients were treated by gap arthroplasty.
Preoperative assessment included the clinical history of the patient, radiographic and physical examination. The collected data were: the cause of the ankylosis, facial asymmetry, presence of micrognathia, the onset time of the ankylosis, the side affected (uni or bilateral) and occlusion. Measurements of maximal interincisal opening (MIO), lateral movements and protrusion were made one day before the surgical procedure. The radiographic examination included panoramic radiographs and computerized axial tomograms to determine the anatomic boundaries of ankylosis and the type of the ankylosis (Figures 1a, 1b, 1c).
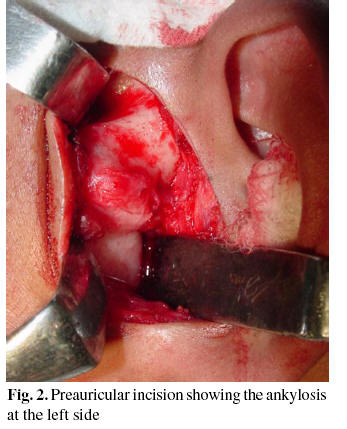
All surgical procedures were performed in the operating room under general anesthesia. The hair in the temporal region was clipped. For all patients, the TMJ approach consisted of a preauricular incision.(8) (Figure 2) Dissection was carried out through the superficial temporal fascia, which was retracted anteriorly to protect the facial nerve, and the periosteum over the zygomatic arch was incised.
After exposing the joint and identification of the site of the ankylosis, aggressive excision of the fibrous and/or bony mass was realized initially with drills and completed with a chisel, followed by excision of the coronoid process and burring of the glenoid fossa, creating a gap of at least 15 mm between the roof of the fossa and the mandible (Figure 3). A passive interincisal mouth opening of at least 30 mm was achieved. Contralateral coronoidectomy was performed when necessary, in accordance with Kaban´s protocol.(9)
After vigorous irrigation with saline, suction drains were placed after the resection to avoid edema and infection. The incisions were closed, and a pressure dressing was applied. The physiotherapy began one day postoperatively with jaw exercises under orientation. During the surgical procedure the following data were collected: time of the operation, maximal mouth opening and occlusion. During the next 3 to 4 weeks the diet was evolved to solid consistency.
All the patients were followed-up at minimum period of evaluation of twenty-four months. Postoperative data consisted of: maximal mouth opening, complications and recurrence.
The results were expressed by mean ± SD. The Wilcoxon matched pairs signed ranks test were used to compare the maximal interincisal opening in the preoperative period and in the posoperative period. Statistical significance was established at the P≤ .05 level.
Results
Eight patients were submitted to TMJ surgery - four men and four women (1:1) with 11 involved TMJs. Five patients (62.5%) had unilateral involvement and three patients (37.5%) bilateral involvement. The mean age was 20 years ± 9 (range 3 to 30 years). Etiology included trauma (n = 6), and others (n = 2). Preoperative CT scans revealed fibrous ankylosis (n = 2), fibro-osseus ankylosis (n = 1) and bony ankylosis (n = 8), and that diagnosis was confirmed when the joint was exposed in the intraoperative period (Table 1).
The mean maximal incisal opening (MIO) in the preoperative period was 9.25± 6.41 mm (range 0 to 17 mm) and in the postoperative period it was 29.88 ± 4.16 mm (range 26 to 37 mm). The results were statistically significant (p = 0.011).
The most frequent complication was temporary facial nerve paralysis and it was encountered in two patients (25%). No recurrence was observed in our series.
Discussion
Trauma is the major cause of TMJ ankylosis in our series (62.5%). The kind of trauma that usually results in ankylosis of the TMJ is predominantly experienced in childhood, and if no treatment is undertaken for a fracture of the condyle, the myositic mass grows in the juxta-articular tissue, resulting in a bone mass. Of particular significance is the decision as to the indication and timing of surgical treatment during childhood. The facial remodeling is greater when the release is done in childhood. Remodeling of the mandible after surgery, especially in unilateral ankylosis, is a phenomenon that has no parallel elsewhere in the body.(5) Our results are similar to the works of Roychoudhury et al and Raveh et al.
The administration of anesthesia to patients with TMJ ankylosis is a challenge inasmuch as securing the airway can be very difficult. It requires considerable expertise and adequate monitoring facilities. (5) The safest technique for securing the airway would be a nasal fiberoptic assisted intubation with the pacient awake and under local anesthesia. However, in our series, 100% of the patients were intubated blindly under spontaneous respiration with oxygen and nitrous oxide.
To prevent surgical recurrence in cases afflicted with ankylosis, radical removal of the bony or fibrous ankylotic segment is essential. (7,9) However the unfavorable anatomic configuration and the proximity of vital structures make the surgical procedure particularly difficult.(8)
Roychoudhury et al. (5) recommended a gap of at least 15 mm between the recountoured glenoid fossa and the mandible and subjected this gap to extensive active jaw opening exercises to prevent re-ankylosis when using gap arthroplasty. In all cases the gap was made accordance with this recommendation.
According to Kaban et al. (9) the advantages of gap arthroplasty are its simplicity and short operating time and the disadvantages include 1) creation of a pseudoarticulation and a short ramus; 2) failure to remove all the bony pathology, and 3) increased risk of reankylosis. In our series, using this technique, we were able to reduce operating time, but patients with bilateral involvement showed more frequent anterior open bite. This complication was treated with physiotherapy and the use of elastics.
A careful surgical technique, and subsequent meticulous attention to long-term physiotherapy are both considered essential to achieve a satisfactory result. (10) Many studies have shown that the choice of interposition material is important in preventing recurrence. (6,11) Interposition of autogenous or alloplastic material at the ostectomy site is a mechanism to prevent recurrence; however, there are possible disadvantages, such as morbidity at the donor site and unpredictable resorption when autogenous material is used, and the risk of a foreign body reaction when alloplastic material is used. (10)
Bilateral arthroplasty is frequently associated to anterior open bite, because there is a shortening of the ramus and only hinge movement is possible. This complication could be minimized, when interpositional arthroplasty or total reconstruction of the TMJ is used. Unstable occlusion after the arthroplasty is corrected once the patient is taught to close in occlusion. (5)
The complication of facial nerve weakness occurs when there is excessive retraction intraoperatively of the soft tissues, and it usually responds to steroid therapy. (4) In our series, patients who experienced this complication (25%) were followed up and within 3 months it has disappeared completely without additional treatment.
![]() Correspondence
Correspondence
Prof. Dr. Belmiro Cavalcanti do Egito Vasconcelos
Faculdade de Odontologia de Pernambuco.
Universidade de Pernambuco.
Av. General Newton Cavalcanti, 1650
Camaragibe Pernambuco. CEP: 54753-220
Fax: 55 (81) 3458 2867
E-mail: belmiroc@terra.com.br
Received: 2-01-2005
Accepted: 19-06-2005
References
1. Gay-Escoda C, Arguero M. La corrección quirúrgica de la anquilosis de la articulación temporomandibular. Descripción de siete casos. Avances en Odontoestomatología 1994;10:74. [ Links ]
2. Kaban L, Pogrel MA, Perrott DH. Complications in oral and maxillofacial surgery. 1st ed. Philadelphia: WB Saunders; 1997. [ Links ]
3. Rowe NL. Ankylosys of the temporomandibular joint. J R Coll Surg Edinb 1982;26:67-79. [ Links ]
4. Kazanjian VH. Temporomandibular joint ankylosis. Am J Surg 1955;90: 905. [ Links ]
5. Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: A report of 50 cases. Oral Surg Oral Med Oral Pathol 1999;87:166-9. [ Links ]
6. Miyamoto H, Kurita K, Ogi N, Ishimaru JI, Goss A. The role of the disk in sheep temporomandibular joint ankylosis. Oral Surg Oral Med Oral Pathol 1999;88:151-8. [ Links ]
7. Raveh J, Vuillemin T, Lädrach K, Sutter F. Temporomandibular joint ankylosis: surgical treatment and long-term results. J Oral Maxillofac Surg 1989;47:900-6. [ Links ]
8. Ellis III E, Zide MF, eds. Surgical Approaches to the facial skeleton. Philadelphia: WB Saunders; 1995. [ Links ]
9. Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg 1990;48:1145-51. [ Links ]
10. Manganello-Souza LC, Mariani PB. Temporomandibular joint ankylosis: Report of 14 cases. Int J Oral Maxillofac Surg 2003;32:24-9. [ Links ]
11. Chossegros C, Guyot L, Cheynet F, Blanc JL, Cannoni P. Full-thickness skin graft interposition after temporomandibular joint ankylosis surgery: A study of 31 cases. Int J Oral Maxillofac Surg 1999;28:330-4. [ Links ]











 texto en
texto en