Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.2 mar./abr. 2006
Basal cell adenoma of the parotid gland. Case report and review of the literature
Adenoma de células basales de glándula parótida. Caso clínico y revisión de la literatura
Raúl González García1, Syong H. Nam Cha2, Mario F. Muñoz Guerra1, C. Gamallo Amat2
(1) Servicio de Cirugía Oral y Maxilofacial
(2) Servicio de Anatomía Patológica, Hospital Universitario
La Princesa. Madrid
ABSTRACT
Basal cell adenoma of the salivary glands is an uncommon type of monomorphous adenoma. Its most frequent location is the parotid gland. It usually appears as a firm and mobile slow-growing mass. Histologically, isomorphic cells in nests and interlaced trabecules with a prominent basal membrane are observed. It is also characterized by the presence of a slack and hyaline stroma and the absence of myxoid or condroid stroma. In contrast to pleomorphic adenoma, it tends to be multiple and its recurrence rate after surgical excision is high. Due to prognostic implications, differential diagnosis with basal cell adenocarcinoma, adenoid cystic carcinoma and basaloid squamous cell carcinoma is mandatory. We describe a case of basal cell adenoma of the parotid gland. We also review the literature and discuss the diagnosis and management of this rare entity.
Key words: Basal cell adenoma, parotid, salivary gland.
RESUMEN
El adenoma de células basales de las glándulas salivares es un tipo de adenoma monomorfo de aparición infrecuente. La localización más habitual es la superficie de la glándula parótida. Suele debutar clínicamente como una masa firme y desplazable de crecimiento lento. Histológicamente se observan células isomórficas formando nidos y trabéculas interanastomosadas, con una membrana basal prominente, separadas por un estroma laxo e hialino y ausencia de estroma mixoide o condroide. A diferencia del adenoma pleomorfo, tiende a la multicentricidad y su tasa de recurrencia después de la extirpación quirúrgica es alta. Debido a sus implicaciones pronósticas, el diagnóstico diferencial con el adenocarcinoma de células basales, el carcinoma adenoide quístico y el carcinoma de células escamosas basalioide es prioritario. Describimos un caso clínico de adenoma de células basales de la glándula parótida, realizamos una revisión de la literatura y discutimos el manejo diagnóstico y terapéutico de esta rara entidad.
Palabras clave: Adenoma de células basales, parótida, glándula salivar.
Introduction
Basal cell adenoma (BCA) of the salivary glands is a rare tumour, recognised as an independent entity in the Second Edition of the Salivary Gland Tumours Classification of the World Health Organization (WHO) (1). It is considered as a low-grade malignant tumour with a high recurrence rate and, in general, good prognosis. The most frequent location is the parotid gland, although other sites are possible, such as the upper lip, buccal mucosa, lower lip, palate and nasal septum (2,3).
It represents 54% of monomorphous adenomas and 1-3% of major salivary glands tumours (4). Epidemiologically, these tumours frequently affect patients between their fifth and seventh decades, in contrast to observations in benign mixed tumours. In the opinion of most authors prevalence in favour of women exists, but other authors report a similar frequency for both genders (5,6).
Histologically, 4 characteristic patterns have been described: solid, trabecular, tubular and membranous. It is characteristic the presence of a basaloid cellular layer with a stockade pattern and rounded by hyaline substance (7). The absence of myoepithelial cells, present in benign mixed tumors and other salivary gland neoplasms, has been referred as characteristic of this tumour (8). However, other authors suggest the concurrence of myoepithelial cells, based in the presence of S-100 stromal fusiform cells (9).
Differential diagnosis with entities of varied prognosis such as pleomorphic adenoma and adenoid cystic carcinoma makes necessary the consideration of this entity in the field of glandular tumours of the maxillofacial area.
Case Report
A 30-year old woman with a history of basal cell carcinoma of the paranasal skin came to our Department because of a 3-year slow-growing tumour in the region of the right mandibular angle. The patient had a previous pathological report performed in other centre consisting in two fine-needle aspiration (FNA) procedures, with result suggestive of low-cytological grade epithelial proliferation. This finding was compatible with a salivary gland pleomorphic adenoma. However, quantity of stroma was minimal, and there were deviations in relation to the standard patterns, so other tumours included carcinoma were not rejected. In the physical exploration, the patient showed a 2-cm nodule in the right jugulodigastric region, mobile over deep layers and not adhered to the skin. No other lymph nodes or masses were observed in the cervical and facial regions.
With the suspected diagnosis of superficial right parotid gland tumour, a contrasted cervicofacial computerized tomography (CT) was performed, considering both bone and soft tissue windows. A 1.5-cm well-defined hyper-take nodular image in the superficial parotid lobe was present. Due to its radiological features and slow progression in 3 years, it was interpreted as a benign tumoral lesion, such as pleomorphic adenoma, Warthin tumour and other benign lesion. Radiologically negative cervical nodes were observed in the submandibular, jugulodigastric and posterior cervical region.
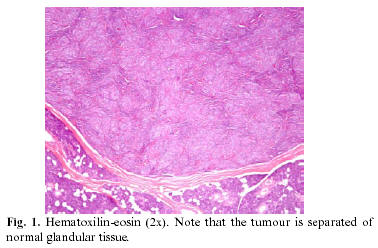
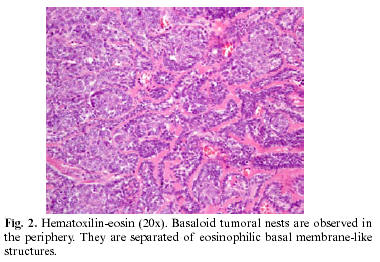
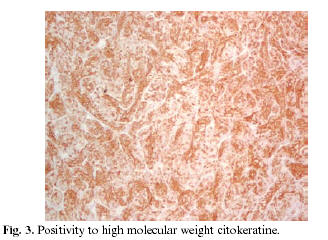
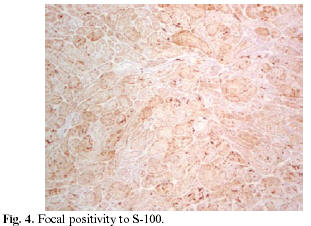
With clinical and radiological diagnosis of benign tumour of the right parotid gland, a suprafacial parotidectomy under general anesthesia was performed. A rithidectomy approach with a 5x3-cm superficial parotid lobe excision and design of the SMAS were performed. In the histological study an 18-mm white-coloured homogeneous and well-defined tumour was observed in the pole of the specimen. After the histological preparation, a well-delimited mass with homogeneous texture was observed. The rest of the glandule showed conventional macroscopic features. A biopsy-resection of a 2.5x1 cm lymph node was also performed in the vicinity of the parotid gland. It showed a white homogeneous appearance and elastic consistency. In the microscopic study, an encapsulated lesion was observed. It was formed by trabecules or nests separated by an eosinophilic basal membrane, and basaloid cells disposed in a peripheric stockade pattern (fig.1,2). Celularity in the immunohistochemical analysis was positive for high-molecular weight cytokeratin and focally positive to S-100 (fig. 3,4). The histological study was basal cell adenoma of parotid gland, and lymph nodes with follicular hyperplasia.
No important complications during the immediate postsurgical period were observed, except for minor frontal and buccal paresia, which experimented progressive improvement after the surgical procedure.
Discussion
Most of parotid tumours (70-80%) are benign and, within this group, pleomorphic adenoma is the most frequent. Within the adenomas group, monomorphic tumours are very uncommon. They are defined as epithelial benign tumours of the salivary glands which are not pleomorphic adenomas. Within this group, basal cell adenoma must be signalled. This tumour is subdivided in solid, trabecular, tubular and membranous subtypes. Frequently, this slow-growing encapsulated tumour do not exceeds 3-cm of major diameter. It is a firm mobile painless mass. It is usually superficial within the glandular body, and a brownish appearance is usually observed (3). The diagnosis of this entity must be established by the histological study. Generally, biopsy is accepted as the most accurate method to obtain the diagnosis, although some authors advocate for FNA if physical access to the tumor is available.
Histologically, BCA is characterized by the presence of uniform and regular basaloid cells. These cells have two differenced morphologies and are intermingled. One group consists in small cells with little cytoplasm and intensive basaloid rounded nuclei that are usually located in the periphery of the tumoral nests or islands. The other group is formed by large cells with abundant cytoplasm and pale nuclei that are located in the centre of the tumoral nests. A basal membrane-like structure rounds these tumoral nests, separating them from the surrounding connective tissue (7). Globally, as it has been referred in classic texts, the tumor adopts an ameloblastoma-like pattern (10). Our case presented histological features similar to those referred in the literature, consisting in basaloid cells disposed in an external stockade pattern and pale-nuclei cells in the centre of the nests. Basal membrane-like structures surrounding cellular nests showed intense eosinophilia which clearly delimited basaloid cells.
Solid BCA are formed by small cells organized in a compact manner. In the trabecular and tubular subtypes, important groups of cells exist. They are disposed in narrow bands and ductal structures or in a combination of both. Membranous subtype is constituted by external cells in a stockade pattern and by an intense hyalinized basal membrane. Some authors have referred the existence of an association between this type and cutaneous cylindroma, trichoepithelioma or eccrine spiradenoma of the scalp (10,11). This association has been observed in one third of the cases. Equally, it has been referred an association of glandular and cutaneous tumours in this BCA subtype, as a dominant autosomic disease, due to the presence of affected subjects within the same family (11-13).
Differential diagnosis must be mostly established with some unfavourable entities, such as the basal cell adenocarcinoma, adenoid cystic carcinoma and basaloid squamous cell carcinoma. In contrast to BCA, an infiltrative growth, more mitotic figures (>4 mitotic count/10 HPF) and Ki67-staining of 5% of the cells are observed in basal cell carcinoma (14). In the adenoid cystic carcinoma, whirlpool of epithelial cells, dark external cells in a stockade pattern and a thick basal membrane-like structure are observed. It is also referred parenchimatous and perineural invasion. Moreover, vascularization in the microcystic areas is absent, in contrast to BCA, in which multiple endothelial canals are present. Some authors have suggested morphometry as a useful method in the differential diagnosis of both entities (15). Basaloid squamous cell carcinoma is characterized by the presence of solid cells in a lobular fashion, close to the superficial mucosa, in which cells are small and have scarce cytoplasm with hyperchromatic nuclei without nucleoli. These cells constitute small cystic spaces filled by mucinous material. In this latter entity, both populations of basal cells are not observed, in contrast to BCA. Continuity of tumoral cells with epithelium of the surface and squamous dysplasia are also observed, in contrast to BCA (16-18). It is interesting that BCA have macroscopic features that may help in the differential diagnosis. Tumoral nests are clearly differenced from inter-epithelial stroma because of an intact basal-cell membrane. This delimitation is observed neither in the pleomorphic adenoma nor in the adenoid cystic carcinoma.
Apart from the pleomorphic adenoma, it is important to consider other benign lesions in the differential diagnosis, such as the mucocele, sebaceous cyst, lipoma and nasolabial cyst. Clinical appearance of BCA may simulate a mucocele of the oral mucosa. Generally, the latter usually appears in the lower lip of young people, whereas the former usually appears in the upper lip of the elder (18).
In relation to the histological diagnosis, immunohistochemical analysis is of great helpful. The majority of authors advocate for the existence of a unique epithelial cell type in the BCA, although some other authors (19) have referred the existence of some heterogeneity in cellular populations, such as ductal epithelial cells and myoepithelial cells. These data contradict what other authors have suggested, in which the absence of myoepithelial cells has been considered as characteristic of this neoplasm, in contrast to pleomorphic adenoma (8). The intense vimentin and HHF-35 staining of some BCA cells have been reported. It is known that these markers are typical for myoepithelial tumoral cells. In the solid BCA subtype the majority of cells show positivity for KL-1 and negativity for vimentin and HFF-35, with a scarce participation of myoepithelial cells. According to some authors (8), it does not occur in the trabecular and ductal subtypes, in which the presence of cells intensively S-100 stained suggest the presence of a myoepithelial nature. However, although some authors (20) advocate for the specificity of S-100 in relation to myoepithelial cells, some other (19) suggest the existence of this marker in the neoplastic cells of BCA, independently of their lineage.
Primary treatment of BCA is surgical excision by means of a suprafacial or total parotidectomy in cases in which parotid affectation exists. Extracapsular excision is performed in cases in which there is affectation of minor salivary glands in the oral mucosa. Total parotidectomy rather than suprafacial parotidectomy has been proposed in the membranous type of BCA. It is due to the elevated tendency to multicentricity, multiple recurrences and occasional malignant transformation (16). It is mandatory not to disrupt the capsule, in order to minimize the risk of recurrence which is observed in rare occasions. Malignization of this tumour has been referred in two occasions (3,21). Despite this benign behaviour, we think that it is completely necessary a long-term follow-up, in order to detect recurrences in a prompt time.
Dr. Raúl González García
C/ Los Yébenes nº 35, 8º C
28047 - Madrid
ESPAÑA
E-mail: raugg@mixmail.com
Received: 4-04-2005
Accepted:12-06-2005
References
1. Seifert G, Sobin LH. The World Health Organization´s Histological Classificatio of Salivary Gland Tumors. Cancer 1992;70:379-85. [ Links ]
2. Mintz GA, Abrams AM, Melrose RJ. Monomorphic adenomas of the major and minor salivary glands. Report of twenty-one cases and review of the literature. Oral Surg 1982;53:375-86. [ Links ]
3. Bernacki EG, Batsakis JG, Johns ME. Basal cell adenoma. Distinctive tumor of salivary glands. Arch Otolaryngol 1974;99:84-8. [ Links ]
4. Luna MA, Tortoledo ME, Allen M. Salivary termal analogue tumors arising in lymph nodes. Cancer 1987;59:212-24. [ Links ]
5. Chaudhry AP, Cutler LS, Satchidanand S, labay G, Sunderraj M. Ultrastructure of monomorphic adenoma (ductal type) of the minor salivary glands. Arch Otolaryngol 1983;109:118-22. [ Links ]
6. Fantasia JE, Neville BW. Basal cell adenomas of the minor salivary glands. A clinicopathologic study of seventeen new cases and review of the literature. Oral Surg 1980;50:433-40. [ Links ]
7. Nagao K, Matsuzaki O, Saiga H, Sugano I, Shigematsu H, Kaneko T, et al. Histopathologic studies of basal cell adenoma of the parotid gland. Cancer 1982;50:736-45. [ Links ]
8. Dardick I, Daley TD, Van Nostrand AWP. Basal cell adenoma with myoepithelial cell-derived stroma: a new major salivary gland tumor entity. Head Neck Surg 1986;8:256-67. [ Links ]
9. Batsakis JG, Brannon RB. Dermal analogue tumors of major salivary glands. J Laryngol Otol 1981;95:155-64. [ Links ]
10. Min BH, Miller AS, Leifer C, Putong PB. Basal cell adenoma of the parotid gland. Arch Otolaryngol 1974;99:88-93. [ Links ]
11. Reingold IM, Keasbey LE, Graham JH. Multicentric dermal-type cylindromas of the parotid glands in a patient with floid turban tumor. Cancer 1977;40:1702-10. [ Links ]
12. Ferrandiz C, Campo E, Baumann E. Termal cylindromas (turban tumor) and ecrine spiradenomas in a patient with membranous basal cell adenoma of the parotid gland. J Cutan Pathol 1985;12:72-9. [ Links ]
13. Batsakis JG. Pathology consultation. Dermal ecrine cylindroma. Ann Otol Rhinol Laryngol 1989;98:991-2. [ Links ]
14. Nagao T, Sugano I, Ishida Y, Hasegawa M, Matsuzaki O, Konno A, et al. Basal cell adenocarcinoma of the salivary glands: comparisson with basal cell adenoma through assesment of cell proliferation, apoptosis, and expression of p53 and bcl-2. Cancer 1998;82:439-47. [ Links ]
15. de Vicente Rodríguez JC, López Arranz JS, Junquera Gutierrez LM, Álvarez Álvarez I, García-Pola Vallejo MJ. Adenoid cystic carcinoma and basal cell adenoma of the parotid gland: a compromised differential diagnosis. Rev Eur Odontoestomatol 1991;3:333-6. [ Links ]
16. Yu GY, Ubmüller J, Donath K. Membranous basal cell adenoma of the salivary gland: a clinicopathologic study of 12 cases. Acta Otolaryngol (Stockh) 1998;118:588-93. [ Links ]
17. Banks ER, Frierson HF, Mills SE, George E, Zarbo RJ, Swanson PE. Basaloid squamous cell carcinoma of the head and neck. Am J Surg Pathol 1992;16:939-46. [ Links ]
18. Zabaleta M, Mollá FJ, Salazar F, Erdozain E, Sánchez L. Monomorphic adenoma of basal cells in a minor salivary gland. Acta Otorrinolaringol Esp 1997;48:169-72. [ Links ]
19. Ogawa I, Nijai H, Takata T, Miyauchi M, Ito H, Ijuhin N. The cellular composition of basal cell adenoma of the parotid gland: an immunohistochemical análisis. Oral Surg Oral Med Oral Pathol 1990;70:619-26. [ Links ]
20. Kahn HJ, Baumal R, Marks A, Dardick I, van Nostrand AWP. Myoepithelial cells in salivary gland tumors: an Immunohistochemical study. Arch Pathol Lab Med 1985;109:190-5. [ Links ]
21. Evans RW, Cruickshank AH. Epithelial tumors of the salivary glands. Major Probl Pathol 1970;1:1-299. [ Links ]











 texto en
texto en