Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.1 ene. 2007
Synovial chondromatosis of the temporomandibular joint
Juan Francisco Reyes Macías 1, Martín Sánchez Prieto 2
(1) Especialista en Diagnostico Integral y Patología Bucal. Master en Medicina Oral por la Universidad de Valencia. Coordinador de los departamentos de Patología y Diagnóstico de la Facultad de Estomatología de la Universidad Autónoma de San Luis Potosí
(2) Cirujano Máxilofacial. Profesor de la Maestría en Endodoncia de la Facultad de Estomatología de la Universidad Autónoma de San Luis Potosí
ABSTRACT
Synovial Chondromatosis (SC) is a disease whose etiology is unknown, can be defined as a benign synovial process characterized by the formation of metaplastic cartilaginous nodes inside connective tissue of articular surfaces, is considered an active metaplastic phenomenon better than a neoplastic process; it presents a greater preference to affect women who constitute almost 70% of reported cases, the age range is wide and oscillates between 18 - 75 years (average 44.6 years). Between the main clinical findings are: pain, crackle, volume augmentation and a limited buccal opening.
SC is an unusual state and the reports in the English literature are no more than 75 cases, only 66 of those where histologically verified, most of those were affecting great joints like hip, knee and shoulder, but if SC is not frequent in this sites, is even more infrequent on temporomandibular joint.
The aim of this paper is to report a clinical case and at the same time to realize a brief review of the literature.
Key words: Chondromatosis, temporomandibular joint, clicking.
RESUMEN
La condromatosis sinovial (CS) es una enfermedad de etiología desconocida, la cual pude definirse como un proceso benigno sinovial caracterizado por la formación de nódulos cartilaginosos metaplásicos dentro del tejido conectivo de las superficies articulares, se le considera un fenómeno metaplásico activo más que un proceso neoplásico; presenta una marcada preferencia por afectar a mujeres constituyendo casi el 70% de los casos reportados, el rango de edad es amplio y oscila entre los 18 y 75 años con una media de 44.6 años. Dentro de los principales hallazgos clínicos destacan: sintomatología dolorosa, presencia de crepitación, aumento de volumen y limitación de la apertura bucal.
La CS es una entidad poco frecuente de la cual se han reportado no más de 75 casos en la literatura inglesa, sólo 66 de ellos comprobados histológicamente, la mayoría afectando principalmente grandes articulaciones como cadera, rodilla y hombro; pero si la frecuencia es rara en estas localizaciones, lo es más aún en la articulación temporomandibular.
El objetivo del presente artículo es el de reportar un caso clínico a la vez que se realiza una breve revisión de la literatura.
Palabras clave: Condromatosis, articulación temporomandibular, chasquido.
Introduction
Synovial chondromatosis is an infrequent disease, who was first described according to Ginaldi (1), in 1558 by Ambrosio Pare. Is an entity that has been mainly reported affecting greater joints as hip, knee and shoulder (2); but if SC is not frequent in this sites, is even more infrequent on temporomandibular joint. (TMJ).
In 1764, Haller (3) reported the presence of shapeless, loose structures inside TMJ; on the other hand, Axhausen in 1969 (4) made the first detailed scientific description followed by others (5-7). Since the first description, there have been reported on English literature not more than 75 cases in which the TMJ is affected.
In an excellent article, von Lindern et al.(2) reported 8 cases and realized the analysis of 74 cases reported between 1764 y 2002, with only 66 of those histopathologically verified.
The aim of this paper is to report a case of synovial chondromatosis and at the same time to realize a review of the literature about it.
Report of the case
Female patient 54 years old, hypertensive well controlled with Captorpil®, presents allergy to amoxicillin and with an antecedent of cryosurgery of the uterus because of intense hemorrhages.
According to her own words, her illness began at 18 years with the eruption of upper right third molar, associated to pain and purulent drainage. She links that event with the starting of "clicking" and light discomfort in right TMJ; she consulted several doctors who recommended the application of humid heat over the skin in the painful site, she presented a temporary improvement but the symptoms returned after 3 weeks.
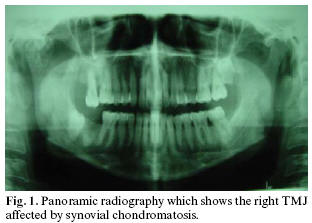
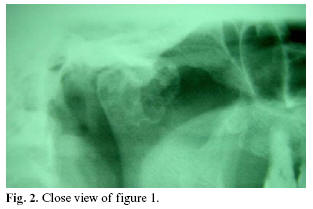
The patient refers she never presented decrease of buccal opening, but presented pain and crackle on right side every time she opened her mouth. In the last 5 years the pain and click were increasing gradually. When she arrived for advice she presented severe pain to buccal opening; at exploration she presented click on TMJ at opening and closing, without limited buccal opening, at palpation we noticed a deformity in TMJ, the panoramic radiography reveled the presence of a mass at level of the right TMJ condyle (Figures 1 and 2), without other alterations.
On the basis of clinical and radiographic findings, the presumptive diagnosis of chondroma and osteoma were established, and even if the clinical findings not supported a lot, a possible malign process must be discarded.
It was explained to the patient about the tumoral nature of the illness, indicating the convenience of a surgical intervention.
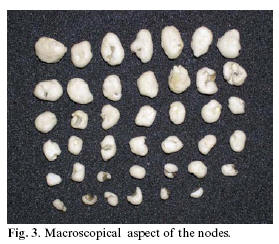
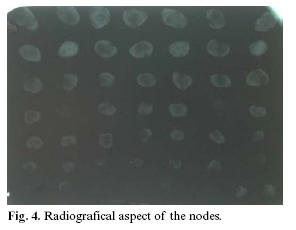
The patient enter to the operating room on June 3 of 2003; under general anesthesia is removed the lesion consisting in multiple fragments of variable size, hard consistence, white-yellow color, oval shaped and smooth surface (Fig.3,4), the fragments were placed into formalin and then were sent for an histopathological study. The patient evolutions without complications and two days after the surgery is discharged and cited on June 10, that day is observed normal healing, the only complain referred was discomfort to buccal opening, the sutures were removed at level of the outer ear and the patient was cited after one week, when was observed normal healing again, therefore the remaining sutures were removed, a dressing with fitoestimulina , a gauze was placed and was prescribed norflex plus 6 tablets per day and the patient was cited after two weeks for revision.
The next month the patient arrived and referred she felt good, she only felt occasional pain on the operated zone, and discomfort in teeth 17 and 46 due to the surgery, and the result of the pathologic study with the diagnosis of synovial chondromatosis was given.
On September 13 a new panoramic radiography was made and no significant differences were observed. Later, the patient was asymptomatic, a forced opening of 43mm was observed, she only referred discomfort at level of the right mandibular molars, therefore the extraction of teeth 47 and 48 is planned and the patient is cited in two weeks. She arrives referring persistence of pain at level of right TMJ, therefore is prescribed 12 mg of Lexotan, the extractions were realized without incidents and was prescribed Zinnat tablets of 250 mg 2 per day and Tylex750; and was cited after one week. She called after 34 days referring intense pain, she came presenting symptoms of acute alveolar osteitis, a healing was placed and the patient was cited after one web for change of the healing or definitive discharge, and then she came practically without discomfort.
On February 7 of 2004 the patient arrives referring light discomfort at level of the right TMJ, at intrabuccal palpation was perceived bilateral muscular spasm and decrease of buccal opening to 45 mm, a new panoramic radiography was taken and didnt revealed evident irregularities of the joint, but neither was observed evidence of cortical maturation at level of the right remaining condyle, therefore, the patient was cited for infiltration of 1 ml of triamcinolone with 1 ml of lidocaine 2% with epinephrine 1:100,000 in the TMJ zone on February 28, presenting temporary facial palsy.
A new appointment was concerted for checking, and actually the patient is asymptomatic and with the same limitation of buccal opening.
Discussion
Synovial chondromatosis (SC) can be defined as an infrequent benign synovial process, characterized for the formation of metaplastic cartilaginous nodes inside the synovial connective tissue of the articular surfaces.
As was mentioned before, the SC of the TMJ is an extremely infrequent entity, with only 66 histopathologically verified cases according some authors,(2) while another mention only 50 reports about it (8). SC is an entity of unknowed etiology, nevertheless Milgram (9, 10) considers that is an active metaplastic phenomenon better than a neoplastic process.
In an analysis of the cases reviewed by Von Linder and et al. (2) the next results were obtained: SC is an entity more frequently observed in women, who constitute almost 69 % of the total of the cases, the age of presentation to diagnosis shows a wide rank oscillating between 18 and 75 years, with an average of 44.6, and affects lightly more the right TMJ than the left [54.4 %(37 cases) vs 45.5 % (31 cases)]. Nevertheless the majority of the cases are monoarticulars, bilateral cases reported exist on literature (11).
Between common clinical findings pain is one of the most important because 74,2% of 66 patients referred pain, while 78.1 % (50 cases) presented volume augmentation, and 61.4 % of 57 patients (35 cases) presented limited buccal opening; about the matter von Lindern (2) does not precise quantities, however Holmlund and et al..(8) in a report of nine cases establish for their patients a minimal buccal opening of 25 mm and a maximum of 40 mm, with an average of 31 mm, observing an increase of buccal opening after treatment. About the presence of clicking, 30 (69.7 %) of 43 patients evaluated presented clicking. About the duration of the symptoms, the data obtained of 65 patients presented a wide variability (between one week to 25 years, with an average of 4.9 years). All the anterior clinical parameters were coincident with the data obtained in our patient.
The terminology about SC is not constant, therefore sometimes are used synonyms as chondrometaplasia, osteochondromatosis and synovial chondrosis. Due to the low incidence, is extremely rare to consider it as a first choice when making diagnosis. Is characterized for the formation, by synovial cells, of cartilaginous nodes inside the synovial membrane (12) who can eventually be ossificated as a metaplastic phenomenon of mesenchymal cells.
Milgram (9) consider the nodes respect to if they are adhered or incipiently free and free nodes. He classificates pathologically the first ones in three groups: 1)synovia osteochondromatosis, 2)fragments of osteochondral fracture in situ and 3) cases of degenerative arthritis or avascular necrosis . On the other hand, for the fee nodes inside the TMJ, propose the next variants: 1) secondary to synovial osteochondromatosis, 2) secondary to osteochondral fractures and 3) secondary to disintegration of the articular surface.
The histopathological variation of 119 cases of Milgram, (9) established the next kind of tissues in the composition of the nodes: a) articular cartilage only (31.9 %), b) articular cartilage and bone (26 %), c) lobular cartilage (15.1 %), d) osteophytic cartilage (10 %), e) bone only (10 %), f) non-identifiable tissue (6.7 %).
Nevertheless most of the cases stay circumscribed to the affected joint, there are reports of cases in which the process can present intra cranial extension, (13) and extension to temporal, parotideus and masticator spaces, (14) and the process can be complicated by displacement and calcification of the articular disk . (15)
With respect to the pathogenesis of the SC, is generally accepted that the metaplastia of the mesenchymal cells plays an important roll in the etiology of this entity. It has been reported a marked immunoreaction for anti-factor transformer of growth beta (TGF-b) on the surface of the synovial membrane, and to tenascin (TN) in extracellullar matrix. (16) About the matter Centrella et al. (17) have been reported that the TGF increases the differentiation of mesenchymal cells and the production of proteoglycans and the replication of chondroblasts. Pearson and et al. (18) establish that the TGF has a preponderant paper in stimulation of the production of extracellullar matrix, especially in the promotion of tenascin, who, in opinion of Mackie et al. (19) is important for the chondrogenesis in extracellular matrix and the mesenchymal condensation of the growing bones. Recent studies,(20) directed to explore the possible responsible factors of the metaplasias of synovial cells in cases of SC, have determinated as responsible to the fibroblastic growth factor receptor (FGFR3).
SC is a benign condition in which the cells are diploids; however, the recurrence in 15 % of the cases determinates an aggressive potential, which is proved starting of a relative frequency of malignant transformation reported in 5 % of the cases (21)
The synovial fluid of patients with SC presents high levels of fibroblastic growing factor (FGF 9) when is compared with other synovial fluids. This factor constitutes the principal link of the fibroblastic growing factor receptor 3 (FGFR 3) and is capable to maintain a line of mesenchymal cells in a proliferative state before their final differentiation. (22)
Finally is necessary to puntualize that in agreement with what was previous said, in opinion of Davis et al. (23), and others (24), SC constitutes an intermedium state between malignant proliferative lesions like chondrosarcomas and benign lesions like enchondromas, on the other hand and even if is a relatively infrequent phenomenon, is necessary to remember its capability of malignant transformation.
References
1. Ginaldi S. Computed tomography feature of synovial osteochondromatosis. Skeletal Radiol 1980;5:219-22 [ Links ]
2. von Lindern JJ, Theuerkaf I, Niederhagen B, Berge S, Appel T, Reich RH. Synovial chondromatosis of the temporomandibular joint: Clinical, diagnostic, and histomorphologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:31-8 [ Links ]
3. Haller AV. Elemental Physiologiae corporus Humani. Sumptibus Societatis Typhograficae, Bernae 1764;8. [ Links ]
4. Axhausen G. Pathologie und therapie des Kiefergelenks. Fortschr Zahnheilk 1933;9:171
5. Trevor D. A case of synovial chondromatosis of the temporo-mandibular joint. Postgrad Med J 1952;28:408-9 [ Links ]
6. Schulte WC, Rhyne RR. Synovial chondromatosis of temporomandibular joint: report of a case. Oral Surg 1969;28:906-13 [ Links ]
7. Silver CM, Simon SD, Litchman HM, Dyckman J. Synovial chondromatosis of the temporomandibular joint: a case report. J Bone Joint Surg 1971;53:777-0. [ Links ]
8. Holmlund AB, Eriksson L, Reinholt FP. Synovial chondromatosis of the temporomandibular joint. Int J Oral Maxillofac Surg 2003;32:143-7 [ Links ]
9. Milgram JW. The classification of loose bodies in human joints. Clin Orthop 1997:124:282-91 [ Links ]
10. Milgram JW. Synovial Chondromatosis: a histopathologic study of thirty cases. J Bone Joint Surg Am 1997:59:792-801 [ Links ]
11. Keogh CF, Torreggiani, Munk PL. Bilateral synovial chondromatosis of the temporomandibular joint. Clinical Radiol 2002;57:862. [ Links ]
12. Robinson D, Hasharoni A, Evron Z, Segal M, Nevo Z. Synovial chondromatosis: the possible role of FGF 9 and FGF receptor 3 in its pathology. Int J Exp Pathol 2000;81:183-9 [ Links ]
13. Nokes SR, King PS, Garcia Jr.R, Silbiger ML, Jones III D, Castellano ND. Temporomandibular joint chondromatosis with intracranial extension: MR and CT contributions. AJR Am Roengenol 1987;148:1173-4 [ Links ]
14. Yildiz ST, Demir A, Kaya A. Synovial chondromatosis of the temporomandibular joint extending to temporalis, masticator, and parotid spaces. J Comput Assist Tomogr 2001;25:126-9 [ Links ]
15. Koyama J, Ito J, Hayashi T, Kobayashi F. Sinovial chondromatosis in the temporomandibular joint complicated by displacement and calcification of the articular disk: Report of Two Cases. AJNR Am J Neuroradiiol 2001;22:1203-6 [ Links ]
16. Fujita S, Iizuka T, Yoshida H, Segami N. Transforming growth factor and tenascin in synovial chondromatosis of the temporomandibular joint: Report of a case. Int J Oral Maxillofac Surg 1997;26:258-9 [ Links ]
17. Centrella M, McCarthy T, Canalis E. Current concepts review; transforming growth factor-beta and remodeling of bone. J Bone Joint Surg Am 1991;73A:1418-28 [ Links ]
18. Pearson CA, Pearson D, Shibahara S, Hofsteenge J, Chiquet-Ehrismann R. Tenascin: cDNA cloning and induction of TGF-[beta]. EMBO J 1988;7:2977-8 [ Links ]
19. Mackie EJ, Thesleff I, Chiquet-Ehrisman R. Tenascin is associated with chondrogenic and osetogenic differentiation in vivo and promotes chondrogenesis in vitro. J Cell Biol 1987;105:2569-79 [ Links ]
20. Robinson D, Hasharoni A, Cohen N, Yayon A, Moskowitz RM, Nevo Z. Fibroblast growth factor receptor-3 as a marker for precartilaginous steam cells. Clin Orthop 1999;367:S163-75. [ Links ]
21. Davis RI, Hamilton A, Biggart JD. Primary synovial chondromatosis: a clinicopathologic review and assessment of malignant potential. Hum Pathol 1988;29:683-8 [ Links ]
22. Hecht D, Zimmerman N, Bedford M, Avivi A, Yayon A. Identification of fibroblast growth factor 9 (FGF9) as a high affinity, heparin dependent ligand for FGF receptors 3 and 2 but no for FGF receptors 1 and 4. Growth Factors 1995;12:223-33 [ Links ]
23. Davis RI, Foster H, Athur K, Trewin S, Hamilton PW, Biggart DJ. Cell proliferation studies in primary synovial chondromatosis. J Pathol 1998;184:18-23. [ Links ]
24. Martín-Granizo R, Sánchez JJ, Jorquera M, Ortega L. Synovial chondromatosis of the temporomandiblar joint; a clinical, radiological and histological study. Med Oral Pathol Oral Cir Bucal 2005;10:272-6. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Juan Francisco Reyes Macías
Facultad de Estomatología de la U. A. S. L. P.
Av. Dr. Manuel Nava No. 2 CP 78290, Zona Universitaria
San Luis Potosí México.
E-mail: jfreyes@uaslp.mx
Received: 2-05-2006
Accepted: 24-10-2006