Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.3 may. 2007
Leiomyoma of the hard palate: A case report
Miguel Angel González Sánchez1, Mar Colorado Bonnin2, Leonardo Berini Aytés3, Cosme Gay Escoda4
(1) DDS and resident of the Master of Oral Surgery and Implantology University of Barcelona Dental School
(2) DDS and Master of Oral Surgery and Implantology University of Barcelona Dental School
(3) DDS, MD. Assistant Professor of Oral Surgery. Professor of the Master of Oral Surgery and Implantology. University of Barcelona Dental School
(4) DDS, MD, PhD. Chairman of Oral and Maxillofacial Surgery. Director of the Master of Oral Surgery and Implantology.
University of Barcelona Dental School. Oral and maxillofacial surgeon of the Teknon Medical Center, Barcelona (Spain)
ABSTRACT
Leiomyoma is a benign smooth muscle tumor that is very rarely located in the oral cavity. It is accepted that the smooth muscle giving rise to this tumor corresponds to the tunica media of the arteries. The tumor can develop at any age, with no clear gender predilection, and typically manifests as a slow-growing, asymptomatic lesion. The diagnosis is based on the histopathological study, with the use of specific staining techniques, including immunohistochemical markers. Treatment consists of complete resection of the lesion, with due safety margins.
We present the case of a 57-year-old male with a tumor located for the previous four months in the region of the hard palate, adjacent to the left upper premolars. After surgical resection with safety margins, hematoxylin-eosin staining and immunohistochemical study confirmed the diagnosis of leiomyoma.
Key words: Leiomyoma, smooth muscle tumor, palatal tumor.
RESUMEN
El leiomioma es un tumor benigno del músculo liso muy poco frecuente a nivel de la cavidad bucal. Se acepta que la fuente de músculo liso originaria de este tumor es la túnica media de los vasos arteriales. Se trata de un tumor que puede aparecer a cualquier edad, sin presentar una clara predilección por el sexo y normalmente lo hace en forma de tumoración asintomática de crecimiento lento. Su diagnóstico está basado en el estudio anatomopatológico, utilizándose tinciones específicas como podrían ser las técnicas de inmunohistoquímica. Su tratamiento consiste en la extirpación completa de la lesión con márgenes de seguridad.
En este artículo se expone el caso de un paciente hombre de 57 años que presentaba una lesión en el paladar duro, adyacente a los premolares superiores del lado izquierdo, de 4 meses de evolución. Tras la exéresis quirúrgica con márgenes de seguridad de dicha lesión, se realizó su estudio anatomopatológico. La tinción con hematoxilina y eosina junto con el estudio inmunohistoquímico de la muestra confirmaron el diagnóstico de leiomioma.
Palabras clave: Leiomioma, tumor de músculo liso, tumor de paladar.
Introduction
Leiomyoma is a benign smooth muscle tumor that may appear in any location, though it is more common in the uterus, gastrointestinal tract and skin. It is rarely found in the oral cavity (0.065%), due to the scarcity of smooth muscle in this territory (1).
Leiomyoma is usually seen in adults and shows no gender predilection. The most frequent oral locations are the lips, tongue, hard and soft palate, and the cheeks.
The tumor generally manifests as a slow-growing painless lesion, often of a purplish color. The diagnosis is exclusively based on the histological findings. Clinically, a differential diagnosis must be established with lesions of the oral mucosa or connective tissue, such as fibromas, lipomas, salivary gland neoplasms, vascular tumors such as lymphangioma or hemangioma, etc. The differential diagnosis moreover must also include the malignant form of leiomyoma, i.e., leiomyosarcoma.
Treatment consists of complete resection, with due safety margins and periodic controls to ensure early identification of possible tumor relapse.
The present article describes a new case of oral leiomyoma, located in the palatal region, and evaluates the clinical and histological characteristics of the lesion, with a view to including the latter in the routine differential diagnosis of oral mucosal lesions.
Clinical case
A 57-year-old male presented with a history of arterial hypertension controlled with medication (telmisartan 80 mg/day via the oral route). There were no surgical antecedents, and no known drug allergies. The patient had stopped smoking (30 cigarettes and a cigar daily) 16 years before, and referred moderate alcohol consumption.
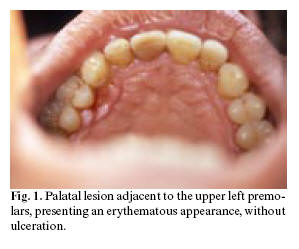
The patient was referred to our Service by his personal dentist for evaluation of an erythematous lesion on the hard palate, adjacent to the palatal surface of the left upper premolars (Figure 1). The lesion had been present for the previous four months and persisted despite treatment by the dentist with antiseptic rinses and antibiotics (spiramycin and metronidazole).
We compiled a case history, and the physical examination revealed a lesion measuring about 5 mm in diameter, located adjacent to the palatal surface of the upper premolars in the second quadrant. The lesion was of a red color, similar to an ulceration, painless and non-hemorrhagic in response to palpation. Orthopantomography revealed no alterations in the region of the lesion. Based on the clinical and radiological findings, moderate chronic periodontitis was diagnosed - the lesion thus being suspected to have a periodontal origin.
Periodontal treatment with an excisional biopsy of the lesion under local anesthetic was decided. A cold scalpel was used to remove the entire lesion, leaving safety margins, with the inclusion of periosteum. The surgical wound was allowed to heal by second intention. There were no intra- or postoperative complications.
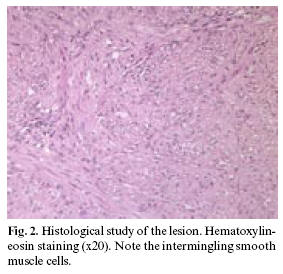
The histopathological study diagnosed oral leiomyoma. Hematoxylin-eosin staining (Figure 2) revealed the presence of intermingling smooth muscle bands separated by cellular fibrous connective tissue. Immunohistochemical techniques were also applied, involving monoclonal antibodies against actin, vimentin, cytokeratin and the S-100 protein (Figure 3). Positivity was observed for actin and vimentin, with negative results for the rest of markers - thus confirming the diagnosis of leiomyoma. Computed tomography (CT) ruled out bone involvement, thus confirming the exclusively mucosal distribution of the leiomyoma.
Periodic controls were made every 6 months the first year, and yearly thereafter. No evidence of tumor relapse was observed after 28 months of follow-up.
Discussion
Leiomyoma is infrequent in the oral cavity, due to the scarcity of smooth muscle in this territory (1). It possible origin has been commented by a number of authors (2,3). Thus, Stout (3) suggested the smooth muscle of the tunica media of the arteries to be the probable origin of oral leiomyomas. Other authors in turn consider leiomyomas to derive from the remains of embryonic tissue such as the lingual duct or circumvallate papilla of the tongue (2).
The first case of oral leiomyoma was described in 1884, and since then a number of additional cases have been documented (1). In the review published by Farman (4) in 1975, involving 7748 smooth muscle tumors located throughout the body, only 5 cases (0.065%) corresponded to the oral cavity. The most common location was the female genitourinary tract, representing 95% of the total cases. Hachisuga et al. (5) recorded 15 cases (2.7%) of oral angioleiomyomas in a series of 562 angioleiomyomas registered in a General Pathology Department. Brooks et al. (6) in turn published a retrospective study of 12 angioleiomyomas, one solid leiomyoma and one leiomyosarcoma, out of a total of 76,412 biopsies / oral lesions registered in a Department of Oral Medicine in the period between 1963 and 2001. The incidence of angioleiomyoma was 0.016%, and represented 92.3% of all benign smooth muscle tumors located in the oral cavity.
Leiomyoma is usually seen in adults - the greatest incidence corresponding to the 40-59 years age interval. Regarding gender distribution, some authors consider both males and females to be affected in equal proportion (7,8), though considerable controversy exists on this point, since other investigators have reported a 2:1 female predilection (6), while others consider males to outnumber females 2:1 (1). Our case corresponded to a 57-year-old male, and coincides with the typical presentations reported in the literature.
The most frequent oral locations are the lips, tongue, hard and soft palate, and the cheeks (9). In the series described by Svane et al. (9), 21% of the leiomyomas were located in the palate. Of these, 91% were angioleiomyomas, while the remaining 9% corresponded to solid leiomyomas. Brooks et al. (6) recorded two angioleiomyomas at palatal level (16.7%) - one in the hard palate and the other in the soft palate.
The World Health Organization (10) classifies leiomyomas into three histological types: leiomyoma (solid), angiomyoma (vascular leiomyoma) and epithelial leiomyoma (leiomyoblastoma). Solid leiomyoma is a well delimited tumor not associated to the vascular smooth muscle, and which consists of a network of fusiform cells with a variable presence of collagen. Angioleiomyomas derive from the smooth muscle of the blood vessels. The smooth muscle fibers of the vessels exhibit a circular distribution around the lumen, and are associated to collagen fibers. Lastly, leiomyoblastoma is composed of round or polygonal cells with clear areas surrounding the nucleus, and an acidophilic cytoplasm. Smooth muscle fibers are rarely found. The most frequent presentation is angioleiomyoma, which accounts for 74% of all oral leiomyomas. In comparison, solid leiomyoma represents 25%, and only one case of leiomyoblastoma has been documented to date (9). According to other authors, angioleiomyomas represent 64-66.2% of all types of oral leiomyomas (6). In a review of 142 oral leiomyomas, 67.0% were vascular leiomyomas, 31.7% corresponded to solid leiomyomas, and 1.3% were leiomyoblastomas (11). This is probably because the main source of smooth muscle tissue in the oral cavity is tunica media of the arteries (7). Duhig and Ayer (12) suggested that vascular leiomyoma represents only a stage within a continuous process of smooth muscle maturation. The maturation sequence would be as follows: hemangioma, angioma, vascular leiomyoma, leiomyoma and solid leiomyoma. According to Damm and Neville (13), solid leiomyoma is histologically very different from angioleiomyoma, and the two entities therefore should be regarded as separate tumors.
Leiomyoma tends to manifest as a smooth-surfaced submucosal nodule. The overlying epithelium rarely ulcerates, though in some cases there is histological evidence of ulceration. The color of the lesions depends on their vascularization and depth. However, although their origin is related to the blood vessels, only 55.9% are red, blue or purple in color. The rest show the appearance of normal mucosa, or have a grayish tone (6). At palpation, the tumors appear firm and are generally well delimited, with free displacement within the lax tissues of the lip and oral mucosa (14). The lesions tend to grow slowly, with a size ranging from a few millimeters to 3 cm (7). In the cases described by Brooks et al., all the lesions were between 2-10 mm in size (6). The tumor in our patient was 7 mm in diameter, and presented a pink-purple color, as commented above.
Most oral leiomyomas present as asymptomatic lesions, though different authors have described clinical symptoms - most often pain in response to palpation, chewing and swallowing difficulties, and tooth mobility (1). Since most leiomyomas are asymptomatic, months or years may elapse before the patient seeks medical help (6).
The diagnosis of leiomyoma is relatively difficult to establish, due to the similarity with other fusiform cell tumors. The differential diagnosis must include other mesenchymal tumors (fibroma, neurofibroma, lipoma, etc.), salivary gland neoplasms (mucocele, pleomorphic adenoma, etc.), vascular tumors (lymphangioma, hemangioma, pyogenic granuloma, etc.), and soft tissue cysts such as dermoid cysts (6,7). When located in the region of the hard palate, adjacent to teeth (as in our case), the tumor can be confused with a periodontal lesion.
The definitive diagnosis of leiomyoma is therefore based on the histological study of the lesion. Leiomyomas are composed of fusiform smooth muscle cells with elongated nuclei, similar to fibroblasts. The cells are distributed in parallel bundles, and the lesions are encapsulated or well delimited within the surrounding tissue. No fibrous stroma is noted - only small capillaries among the tumor cells (14). In order to differentiate leiomyoma from the rest of fusiform cell tumors, specific stains are used to identify collagen and muscle cells, such as the Van Gieson, Masson trichromic and Mallory phosphotungstic acid-hematoxylin (PTAH) stains. Van Gieson staining is recommended for muscle. The Masson trichromic stain differentiates the cytoplasmic elements of the smooth muscle cells, which stain red, from collagen and fibroblasts, which stain blue or green. However, both the Van Gieson and Masson trichromic stains can give rise to false positive results for muscle and collagen fibers; it is therefore advisable to confirm the presence of myofibrils by using the Mallory PTAH stain (13). Immunohistochemical techniques can also be used, as in our patient. In this context, specific monoclonal antibodies for actin (a smooth muscle marker) are useful for confirming the diagnosis of leiomyoma.
Leiomyoma must be carefully differentiated from leiomyosarcoma, particularly low-grade leiomyosarcoma. To this effect, a determinant factor is the presence of mitotic figures. In the presence of over 10 mitoses per high-magnification field (x40), the lesion is considered to have a malignant behavior, while fewer than two mitotic figures per 10 high-magnification fields is indicative of a good prognosis (1). The presence of ulceration is also considered to be indicative of malignancy. Immunohistochemical techniques and molecular markers such as PCNA, bcl-2, CDK4, p53 and MDM2 are correlated to malignant lesions; the diagnostic procedure for differentiating muscle tumors is therefore based on these methods (15).
The treatment of choice is local resection, including an adequate safety margin of normal-appearing tissue. Despite the vascular origin of these lesions, important bleeding after exeresis is rare. Likewise, these benign smooth muscle tumors rarely relapse. Nevertheless, Brooks et al. (6) documented relapse two weeks and 9 months after resecting two hard palate leiomyomas.
It can be concluded that leiomyoma is a benign tumor of scant incidence in the oral cavity, and with a good prognosis, though it must be included in the differential diagnosis of oral mucosal lesions. The treatment of choice is surgical resection with adequate safety margins in all cases, due to the high incidence of malignancy of this tumor within the oral cavity, when compared with the rest of anatomical locations. The possibility of relapse moreover requires periodic patient controls after resection.
References
1. Lloria-Benet M, Bagán JV, Lloria de Miguel E, Borja-Morant AB, Alonso S. Leiomioma oral: A propósito de un caso clínico. Med Oral 2003;8:215-9. [ Links ]
2. Praal FR, Ioannides CA, Jan van Beek G, Van de Molengraft F. Oral leiomyomas. J Maxillofac Surg 1982;10:229-35. [ Links ]
3. Stout AP. Solitary cutaneous and subcutaneous leiomyoma. Am J Cancer 1937;29:435. [ Links ]
4. Farman AG. Benign smooth muscle tumours. S Afr Med J 1975;49:1333-40. [ Links ]
5. Hachisuga T, Hashimoto H, Enjoji M. Angioleiomyoma: A clinicopathologic reappraisal of 562 cases. Cancer 1984;54:126-30. [ Links ]
6. Brooks JK, Nikitakis NG, Goodman NJ, Levy BA. Clinicopathology characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;94:221-7. [ Links ]
7. Leung KW, Wong DY, Li WY. Oral Leiomyoma: Case Report. J Oral Maxillofac Surg 1990;48:735-8. [ Links ]
8. Natiella JR, Neiders ME, Greene GW. Oral leiomyoma: Report of six cases and a review of the literature. J Oral Pathol 1982;11:353-65. [ Links ]
9. Svane TJ, Smith BR, Cosentino BJ, Cundiff EJ, Ceravolo JJ. Oral leiomyomas: Review of the literature and report of a case of palatal angioleiomyoma. J Periodontol 1986;7:433-5. [ Links ]
10. Enzinger F, Lattes R, Torloni H. Histological typing of soft tissues and tumors. Geneva, World Health Organization 1969:30-1. [ Links ]
11. Baden E, Doyle JL, Lederman DA. Leiomyoma of the oral cavity: A light microscopic and immunohistochemical study with review of the literature from 1884-1992. Oral Oncol Eur J Cancer 1994;30:1-7. [ Links ]
12. Duhig JT, Ayer JP. Vascular leiomyoma: A study of sixty-one cases. Arch Pathol 1959;68:424-30. [ Links ]
13. Damm DD, Neville BW. Oral leiomyomas. Oral Surg 1979;47:343-7. [ Links ]
14. Sapp J, Eversole L, Wysocki G. Patología oral y maxilofacial contemporánea. Madrid: Elsevier; 2005. p. 314-5. [ Links ]
15. Nikitakis NG, Lopes M, Bailey J, Blanchaert R, Ord R, Sauk J. Oral leiomyosarcoma: Review of the literature and report of two cases with assessment of the prognosis and diagnostic significance of immunohistochemical and moleculars markers. Oral Oncol 2002;38:201-8. [ Links ]
![]() Correspondence:
Correspondence:
Prof. Cosme Gay Escoda
Centro Médico Teknon
C/Vilana,12.
08022. Barcelona
E-mail: cgay@ub.edu
Received: 5-08-2006
Accepted: 08-03-2007