Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versión On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.12 no.6 oct. 2007
Cinnamon products as a possible etiologic factor in orofacial granulomatosis
Hiroyasu Endo1, Terry D. Rees2
(1) Assistant Professor, Department of Periodontology, Nihon University, School of Dentistry at Matsudo, Japan
(2) Professor and Former Chairman, Director of Stomatology, Department of Periodontics, Baylor College of Dentistry, Texas A&M University Health Science Center, Dallas, TX, USA
ABSTRACT
Objectives: It has been reported that clinical changes due to hypersensitivity reactions to various foods, preservatives, and oral hygiene products may be consistent with the characteristic signs of orofacial granulomatosis (OFG). The objective of this study was to examine 37 well-documented cases of cinnamon-induced contact stomatitis for clinical and histological features consistent with a diagnosis of OFG.
Study design: We reviewed the records of the 37 cases to screen them for the clinical and histopathologic features of OFG.
Results: Twelve patients showed clinical characteristics of OFG. The most commonly affected site was the gingiva. Focal non-caseating, epitheloid granulomas were observed in four histologic specimens. Multinucleated giant cells were observed in an additional four cases.
Conclusions: Although OFG may have multiple etiologies, it is clear that, in some instances, a hypersensitivity reaction to cinnamon products can elicit lesions consistent with OFG.
Key words: Orofacial granulomatosis, cinnamon, contact stomatitis.
Introduction
The term orofacial granulomatosis (OFG) was suggested by Wiesenfeld et al. (1) in 1985 as representative of one or more of a group of diseases or disorders that feature the presence of non-caseating, epitheloid granulomas involving the facial or oral tissues. In general, however, these diseases may or may not have distinct histologic features. Focal granulomas may be present, and lymphangiectasia and perivascular lymphocytic infiltration have been described. However, a non-specific inflammatory infiltrate is occasionally the only histopathologic finding. On other occasions, multinucleated giant cells may be evident. Clinically, the conditions may manifest as localized or generalized erythema, edema and tissue enlargement. The lips or face may be swollen, and the buccal mucosa and tongue may exhibit enlargement, folding, leukoplakia and occasional ulceration. A fiery red gingivitis is often noted. These tissue changes may be induced by a variety of conditions such as Crohns disease, sarcoidosis, foreign body reaction, deep mycotic infections and possibly, contact allergic reactions (2-7). Melkersson-Rosenthal syndrome (MRS) is an unusual related condition that features orofacial swelling, facial paralysis (Bells palsy) and fissuring of the dorsum of the tongue. According to some authorities, the presence of only one or two features of MRS should be classified as monosymptomatic or oligosymptomatic MRS (3).
In recent years, a number of case reports and case series have suggested that OFG is sometimes elicited by a hypersensitivity reaction to various foods, preservatives, oral hygiene products and dental restorative materials (3,7-16). Although not all authors are in agreement with this conclusion (17,18), in some cases, eliminating provoking factors clearly led to remission of OFG signs and symptoms (3,9-14). Reported provoking factors of OFG are cocoa (16), cinnamon (3,9), carvone (9), piperiton (9), aspartate(14), carmoisine (11), sunset yellow (11), monosodium glutamate (11,13), sodium benzoate (12) and tartrazine (12). A few case reports have described OFG as a hypersensitivity reaction to dental restorative metals and remission after removal of the materials (7,15,19).
Cinnamon is a common flavoring agent contained in toothpaste, foods, and chewing gum and is known to occasionally cause contact allergic stomatitis (20-22). In a previous paper, we reported on characteristic clinical symptoms, diagnosis, and treatment in 37 cases of cinnamon-induced contact stomatitis (20). Characteristic clinical symptoms of OFG were observed in the lips, gingiva, and buccal mucosa in some cases (20). These characteristics have rarely been described in other papers reporting on cinnamon-induced contact stomatitis. The objective of this study was to examine 37 well-documented cases of cinnamon-induced contact stomatitis for clinical and histological features consistent with a diagnosis of OFG.
Materials and methods
The subjects were 37 patients diagnosed with cinnamon-induced contact stomatitis, as described in a previous paper (20). Briefly, we examined the patient records from the database of the Stomatology Center at Baylor College of Dentistry and identified 65 cases from 1985 through 1998 that were classified as cinnamon-induced contact stomatitis. The records examined contained information such as the types of oral hygiene products being used by the patients and the frequency of gum chewing. Patients kept food diaries for 1 to 2 weeks, and the contents of their diets were evaluated if necessary. In some cases, evaluation included patch tests and biopsies. In 37 of these 65 cases, causative cinnamon flavoring agents were identified, and signs and symptoms subsided after discontinuing the use of the agents. These 37 cases were used in the present study. Of these 37 cases, five were males and 32 were females ranging in age from 20 to 80 years with an average age of 48.4+/-15.2 years. All 37 patients were examined for clinical features of OFG. Those with such features were analyzed in more detail. Selection of the OFG cases from patient records was based on recorded clinical symptoms or biopsy reports (1,8,9,22). The diagnostic criteria were lip swelling, erythema in the gingiva and oral mucosa, localized edema, or tissue enlargement. The histologic presence of non-caseating granulomas or multinucleated giant cells in biopsy reports was considered to be characteristic of OFG.
Results
Of the 37 patients diagnosed with cinnamon-induced contact stomatitis, 12 (32%) showed characteristics of OFG (Table 1). The 12 patients included two males and ten females aged 20 to 65 years with an average age of 45.1+/-14.8 years. The cinnamon-containing causative agents were toothpaste and foods. One case was caused by cinnamon-flavored chewing gum.
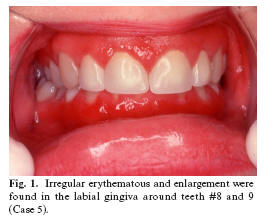
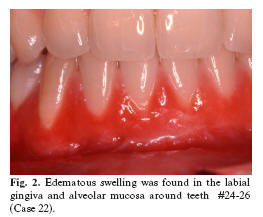
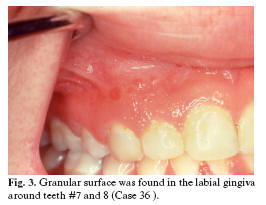
The most common site of clinical signs and symptoms was the gingiva (9 cases, or 75% of the OFG group), followed by the lips (6 cases) and the tongue (6 cases). The clinical symptoms described were erythematous gingiva (8 cases), lip swelling (6 cases), and edematous gingiva (5 cases) (Table 1, Figures 1 and 2). Other characteristic clinical signs described were a granular gingival surface (3 cases, Figure 3), gingival hyperplasia (1 case), and cobblestone enlargement of the buccal mucosa (1 case).
Of the 12 patients with clinical features of OFG, seven underwent histopathological examination of the gingiva or the buccal mucosa. All seven showed non-specific inflammatory reactions and this was the exclusive feature in two cases. Focal granulomas were reported to be present in the lamina propria of four cases, while four cases exhibited the presence of multinucleated giant cells. In three of these cases both granulomas and giant cells were present (Table 2). Five of the 12 OFG patients underwent patch testing for cinnamon using standard skin tests for cinnamon compounds (5% cinnamic acid and 2% trans cinnamic aldehyde). All five showed positive reactions to cinnamic acid and/or cinnamic aldehyde.
Discussion
After examining the patient records of the 37 cases of cinnamon-induced contact stomatitis, 12 patients (32%) were found to have clinical and/or histopathologic characteristics consistent with OFG. The provoking factors were cinnamon-containing foods or cinnamon-flavored toothpaste. Discontinuation of cinnamon-containing causative agents led to remission of symptoms in all of the 12 cases. It must be remembered that OFG may have any one of several possible etiologies. Therefore, it is important to question patients about the presence of symptoms possibly suggestive of Crohns disease, sarcoidosis or angioedema. If such symptoms are noted, the patient should be referred for appropriate medical examination. Testing may include laboratory screening tests such as complete blood count with differential and blood chemistry (Crohns disease), serum angiotensin-converting enzyme and/or chest X-ray (sarcoidosis), and assessment of C-1 esterase inhibitor levels (angioedema) (3). Additionally, however, patients should be questioned regarding the type(s) of oral hygiene products they use, and a 1-2 week food diary may help identify causative agents (3,20). Diagnosis of contact stomatitis is determined when the discontinuation of the intake of the causative agent(s) results in the remission of clinical signs and symptoms. This was achieved in all of the 12 cases included in this study. It has been suggested that allergic reactions associated with OFG represent a delayed, cell-mediated immune response, since the rate of clinical atopy is high in OFG patients (23). However, contact stomatitis due to cinnamon may represent either a contact allergy or a contact irritant effect. Patch testing proved to be effective for identifying the antigens involved in the allergic reactions of our patients, thereby demonstrating that the stomatitis was not due to irritant effect alone.
Based on these findings, patch testing for appropriate allergens appears to be an important component in the diagnostic process for suspected OFG (3). Although not all 12 patients underwent patch tests, all five of the patients that did undergo patch tests experienced a positive reaction to cinnamon in this study. The two most common cinnamon flavoring agents are cinnamic aldehyde, the principal component of cinnamon oil, and cinnamic acid. Toothpaste intolerance has been reported previously in some OFG cases (3,9,10). Common allergens in toothpaste are flavoring agents and preservatives (3,20,21). Most reports indicate that adverse reactions due to the use of cinnamic aldehyde-containing tartar control toothpaste commonly occur in the gingiva (20,21). These reactions may take place because the causative agents mainly come into contact with the gingiva during tooth brushing (21).
In the cases examined in this study, 50% of the patients experienced lip swelling, a typical clinical symptom of OFG. However, the most common site of signs and symptoms of OFG was the gingiva (75%). A few authors previously described gingival manifestations in OFG (1,3,8,22). Involved gingiva has been described as erythematous (1,22), enlarged (1), thickened (9), hyperplastic (8,9), granular textured (22) or lobulated with extensive edematous swelling (22). Some of our patients were reported to have granular surface changes and hyperplasia in addition to gingival erythema (Table 1). Consistent with previous reports (1,8,9,22), these symptoms were observed in the anterior region (20) and were clearly different from those of dental plaque-induced gingivitis (1,8,22). Wiesenfeld et al. (1) examined 60 cases of OFG and reported that 22% showed gingival symptoms. Worsaae et al. (22) described the gingival symptoms of five cases of MRS. They stated that gingival signs and symptoms are common in patients with MRS and that they may sometimes be the first manifestation of MRS. Ferguson et al. (8) suggested that the gingival form of the disorder is probably under-diagnosed and is more likely to be ascribed to inadequate oral hygiene, especially when gingival involvement is the only manifestation of OFG. In addition, Rees (3) recommended that periodontists should pay more attention to OFG because the number of OFG patients appears to be increasing, and gingival involvement is relatively common.
Buccal and labial mucosa are also sites affected in OFG patients (1,8). Edematous mucosa may have a characteristic "lobulated" or "cobblestone" appearance. In this study, buccal cobblestoning was seen in only one case.
OFG is histopathologically characterized by the presence of non-caseating granulomas in the lamina propria, with or without multinucleated giant cells (1,8,9,22). However, not all OFG patients show these features (1,3,8). Wiesenfeld et al. (1) reported that 47 of 57 cases of OFG showed granulomas, but no clinical differences were noted between those individuals with granulomas and those without. Similarly, some of our cases with characteristic clinical signs of OFG (labial swelling, granular surface changes, cobblestoning, gingival erythema) showed no granulomas or multinucleated giant cells although all histopathologic specimens were infiltrated with inflammatory cells. In order to routinely detect histolopathologic features of OFG, it may be necessary to extend biopsies deep into the tissues because granulomas may be found superficially or deep within connective tissues or even in submucosa (1,8). It is also possible that granuloma formation is a late feature in the development of OFG lesions and, therefore, is not visible in tissue obtained from early lesions in individuals with an allergenic component to their condition. (3)
In conclusion, 12 of 37 patients with cinnamon-induced contact stomatitis showed clinical features characteristic of OFG. The provoking factors in these cases were cinnamon-containing foods or cinnamon-flavored toothpaste. In all 12 patients, eliminating the use of cinnamon-containing foods or products led to resolution of the lesions. The most common site of signs and symptoms was the gingiva, which characteristically showed gingivitis that extended into the alveolar mucosa. The reason adverse reactions due to cinnamon may target the gingiva has not been fully elucidated, but it is probable that allergens are concentrated in that area of the oral cavity. The results of this study indicate that contact allergic reactions to cinnamon-containing foods and oral hygiene products may be one of the etiologic factors associated with OFG.
References
1. Wiesenfeld D, Ferguson MM, Mitchell DN, MacDonald DG, Scully C, Cochran K, et al. Oro-facial granulomatosis--a clinical and pathological analysis. Q J Med. 1985 Jan;54(213):101-13. [ Links ]
2. Sciubba JJ, Said-Al-Naief N. Orofacial granulomatosis: presentation, pathology and management of 13 cases. J Oral Pathol Med. 2003 Nov;32(10):576-85. [ Links ]
3. Rees TD. Orofacial granulomatosis and related conditions. Periodontol 2000. 1999 Oct;21:145-57. [ Links ]
4. Girlich C, Bogenrieder T, Palitzsch KD, Scholmerich J, Lock G. Orofacial granulomatosis as initial manifestation of Crohns disease: a report of two cases. Eur J Gastroenterol Hepatol. 2002 Aug;14(8):873-6. [ Links ]
5. Mignogna MD, Fedele S, Lo Russo L, Lo Muzio L. Orofacial granulomatosis with gingival onset. J Clin Periodontol. 2001 Jul;28(7):692-6. [ Links ]
6. Armstrong DK, Biagioni P, Lamey PJ, Burrows D. Contact hypersensitivity in patients with orofacial granulomatosis. Am J Contact Dermat. 1997 Mar;8(1):35-8. [ Links ]
7. Lazarov A, Kidron D, Tulchinsky Z, Minkow B. Contact orofacial granulomatosis caused by delayed hypersensitivity to gold and mercury. J Am Acad Dermatol. 2003 Dec;49(6):1117-20. [ Links ]
8. Ferguson MM, MacFadyen EE. Orofacial granulomatosis--a 10 year review. Ann Acad Med Singapore. 1986 Jul;15(3):370-7 [ Links ]
9. Patton DW, Ferguson MM, Forsyth A, James J. Oro-facial granulomatosis: a possible allergic basis. Br J Oral Maxillofac Surg. 1985 Aug;23(4):235-42. [ Links ]
10. Haworth RJ, MacFadyen EE, Ferguson MM. Food intolerance in patients with oro-facial granulomatosis. Hum Nutr Appl Nutr. 1986 Dec;40(6):447-56. [ Links ]
11. Sweatman MC, Tasker R, Warner JO, Ferguson MM, Mitchell DN. Oro-facial granulomatosis. Response to elemental diet and provocation by food additives. Clin Allergy. 1986 Jul;16(4):331-8. [ Links ]
12. Pachor ML, Urbani G, Cortina P, Lunardi C, Nicolis F, Peroli P, et al. Is the Melkersson-Rosenthal syndrome related to the exposure to food additives? A case report. Oral Surg Oral Med Oral Pathol. 1989 Apr;67(4):393-5. [ Links ]
13. Oliver AJ, Rich AM, Reade PC, Varigos GA, Radden BG. Monosodium glutamate-related orofacial granulomatosis. Review and case report. Oral Surg Oral Med Oral Pathol. 1991 May;71(5):560-4. [ Links ]
14. Reed BE, Barrett AP, Katelaris C, Bilous M. Orofacial sensitivity reactions and the role of dietary components. Case reports. Aust Dent J. 1993 Aug;38(4):287-91. [ Links ]
15. Guttman-Yassky E, Weltfriend S, Bergman R. Resolution of orofacial granulomatosis with amalgam removal. J Eur Acad Dermatol Venereol. 2003 May;17(3):344-7. [ Links ]
16. Taibjee SM, Prais L, Foulds IS. Orofacial granulomatosis worsened by chocolate: results of patch testing to ingredients of Cadburys chocolate. Br J Dermatol. 2004 Mar;150(3):595. [ Links ]
17. Van der Waal RI, Schulten EA, van der Meij EH, van de Scheur MR, Starink TM, van der Waal I. Cheilitis granulomatosa: overview of 13 patients with long-term follow-up--results of management. Int J Dermatol. 2002 Apr;41(4):225-9. [ Links ]
18. Morales C, Penarrocha M, Bagan JV, Burches E, Pelaez A. Immunological study of Melkersson-Rosenthal syndrome. Lack of response to food additive challenge. Clin Exp Allergy. 1995 Mar;25(3):260-4. [ Links ]
19. Pryce DW, King CM. Orofacial granulomatosis associated with delayed hypersensitivity to cobalt. Clin Exp Dermatol. 1990 Sep;15(5):384-6. [ Links ]
20. Endo H, Rees TD. Clinical features of cinnamon-induced contact stomatitis. Compend Contin Educ Dent. 2006 Jul;27(7):403-9; quiz 410, 421. [ Links ]
21. Rees TD. Drugs and oral disorders. Periodontol 2000. 1998 Oct;18:21-36. [ Links ]
22. Worsaae N, Pindborg JJ. Granulomatous gingival manifestations of Melkersson-Rosenthal syndrome. Oral Surg Oral Med Oral Pathol. 1980 Feb;49(2):131-8. [ Links ]
23. James J, Patton DW, Lewis CJ, Kirkwood EM, Ferguson MM. Oro-facial granulomatosis and clinical atopy. J Oral Med. 1986 Jan-Mar;41(1):29-30. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Hiroyasu Endo
Dept. of Periodontology
Nihon University School of Dentistry at Matsudo
2-870-1 Sakaecho Nishi, Matsudo
Chiba, Japan. 271-8587
E-mail: endo.hiroyasu@nihon-u.ac.jp
Received: 17-09-2006
Accepted: 25-03-2007