INTRODUCTION
Acute kidney disease (KD) causes between 5-7% of hospitalizations in acute care units and 30% of admissions in intensive care units (ICU), where mortality is up to 50%1. In Spain, the chronic kidney disease (CKD) prevalence in people over 64 years is around 21.4%. This population is more vulnerable to suffer from potentially inappropriate medication (PIMs) because of the combination of pluripathology and polymedication2.
Many drugs (and their metabolites), which represents a part of the patients' polypharmacy, are mainly excreted by the kidneys. An alteration in this level, as a result, can produce a decrease in its elimination, increasing its half-life and plasma concentrations. This can be highly dangerous in drugs with narrow therapeutic index, which serious adverse effects could appear3. As a consequence of this, a huge number of guidelines and recommendations have been published by scientific societies and other authors, whose purpose is to establish the appropriate adjustment of the regimen (dose and rate of administration) of drugs that are eliminated by kidneys, and even propose their withdrawal, depending on the different stages of kidney disease.
Safety is one of the main characteristics of Health Care Systems. Therefore, it is necessary to introduce tools in daily clinical practice to optimize the pharmacotherapy in patients with KD, in order to detect and prevent PIMs that could potentially cause clinical negative consequences and unnecessary costs associated. However, several studies carried out in different hospitals revealed discrepancies between clinical performance and the recommendations included in the guidelines4,5.
These tools consist on training physicians and pharmacists in this subject, by integrating the pharmacist in care units or incorporating assisted electronic prescribing programs in clinical practice. Nevertheless, cross-validation methods with pharmacist intervention remain effective in optimizing prescription results and patient safety.
Aim of the study
The aim of this study is to evaluate the acceptance rate of the pharmaceutical interventions carried out, through the implementation of a daily cross-validation procedure in electronic prescription in patients with KD, susceptible to suffer a drug-related problem (DRP).
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Comité de Ética de la Investigación con medicamentos del Hospital Universitario Severo Ochoa) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
METHOD
A prospective 9-month intervention study was carried out in a 400-bed medium general university hospital, with a clinical electronic history, electronic prescription system and a Pharmacokinetic Unit in the Pharmacy Unit.
The study included adult patients, admitted to any hospitalization unit and emergency room, with serum creatinine (Cr) levels greater than 1.7 mg/dL. The patients excluded from study were those on hemodialysis and hemofiltration and those who died during the study period. Patients admitted in Nephrology Unit were rejected also because nephrologists use to adjust drugs susceptible of cause renal impairment.
The drugs included in the study were those prescribed and susceptible to dosage regimen adjustment (dose, rate of administration, or both) or those contraindicated in KD. We excluded prescribed drugs that were monitored by plasma levels in the Pharmacokinetic Unit, regardless of the elimination route: valproic acid, amikacin, carbamazepine, cyclosporine, digoxin, phenytoin, phenobarbital, gentamicin, lithium, theophylline and vancomycin.
Data was recorded in Microsoft Excel® and the following items were collected:
1. Demographic data: history number, age, sex, weight, clinical service.
2. Pharmacological data: medication, administration schedule, administration route.
3. Analytical data: Cr and estimated glomerular filtration rate calculated.
4. Intervention: intervention text, type of intervention, acceptance or rejection.
Creatinine clearance (CrCl) was assessed according to estimated glomerular filtration rate (GRF), calculated with MDRD-4 equation (Modification of Diet in Renal Disease): GFR ml/min/1.73 m2 = 186 x (concentration Cr [mg/dl]) - 1,154 x (age [years]) - 0.203 x (0.742 [if woman]) x (1,210 [if black race]).
Based on GFR value obtained, patients were grouped into three categories of KD according to National Kidney Foundation classification, based on the KDIGO guidelines, and the document consensus of the Spanish Society of Nephrology (SEN).
The adjustment recommendations were made based on the value of the GFR obtained through treatment sheets from other bibliographic sources.
The study´s process was conducted by daily incorporation of patients with drugs susceptible to adjust in KD. It was performed by calculating the GFR and stage of KD, collecting the patient's clinical situation (through the electronic history clinic application SELENE®) and, if it was necessary, carrying out the intervention. This was done in all cases by means of a written alert in the electronic prescription program, FARHOS®. After 48 hours of this intervention, the physicians´ responses were noted taking into account their type.
Data analysis was carried out with StataIC 14® statistical software.
RESULTS
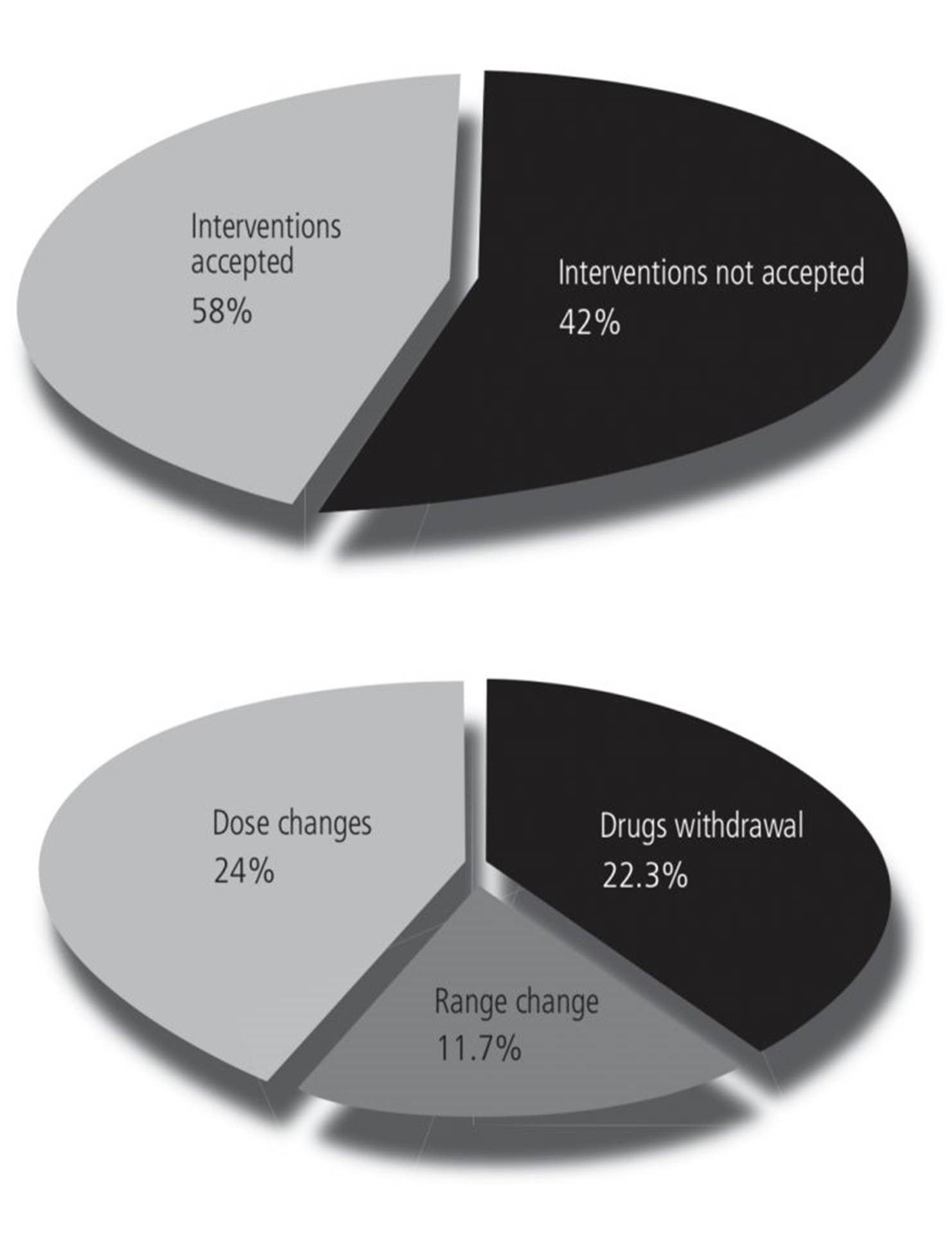
During the period, from February to October 2017, an amount of 11467 patients were admitted to hospital, of which 539 presented inclusion criteria. 179 interventions were performed in 135 (25%) patients, of which 104 (58%) were accepted by the physician (Table 1).
Twenty percent of total interventions were done in KD G3 stage patients, 56% with G4 stage and 23% with G5 stage. No interventions were performed in G1 and G2 stage patients (Table 1).
Table 1. Characteristics of the population and interventions accepted and unaccepted according to degree of renal impairment

Within the accepted interventions, 43 (41.3%) were due to dose change, 40 (38.4%) to drug withdrawal and 21 (20.1%) to range change (Figure 1). We evaluated whether the degree of KD was influenced by the number of accepted interventions, not being statistically significant (p=0.302).
Interventions were carried out in 25 active ingredients divided into 13 therapeutic groups, of which antibiotics are those that represent the greatest number of interventions. Analyzing by drugs, the main four active principles with higher number of interventions both performed and accepted are: spironolactone, ranitidine, meropenem and allopurinol (Figure 2).
Administration route was also analyzed, with 112 (62.57%) interventions in orally administered drugs and 66 (36.87%) in intravenous drugs. No statistical significance was found when analyzing the accepted interventions against administration route (p=0.068).
The interventions performed by clinical services were also analyzed. General Medicine was the service with the highest number of interventions, with 68 (38%) and an acceptance rate of 58.8%. During the study period, 1,641 patients were in charge of this service, and one of twenty-four KD patients required adjustment recommendations in their prescription. The second service with most interventions was Emergency, with 25 (14%) and an acceptance rate of 76%. No statistically significances were found when analyzing the accepted interventions versus the prescribing service (p=0.168).
Table 2 shows interventions by age group. No statistical differences were found between the accepted interventions and the age group (p=0.288).
DISCUSSION
KD is a public health problem since it affects a large percentage of population. According to data of SEN, only in the Community of Madrid more than 550,000 people suffer from it and 6,900 would require dialysis or kidney transplant. Age is one of the risk factors for the development of KD, because the prevalence in people over 65 rises up to 21%. Moreover, a huge percentage of these patients have comorbidities and polypharmacy. This scenery could worsen the patient's clinical situation, leading to a possible increase in the incidence of PIMs in those drugs that are preferably excreted by kidneys6.
One of the main aspects that arises in the pharmacotherapeutic follow-up of the elderly patient with KD is to evaluate whether the pharmacological treatment is either dose-adjusted or it is established by the recommended guidelines for renal clearance, being real or estimated. There are guidelines, recommendations and publications in this field. However, in many cases they are not carried out in the daily clinical practice due to various circumstances. In the bibliography, there are described different ways to inform and to recommend, varying from assisted electronic prescription systems (through a set of alerts) to manual review systems of treatments by pharmacists or other health professionals, all of them with different outcomes7.
In our hospital there is an electronic prescribing system, with analytical data integration, but currently there is no specific prescription for drugs adjustment in KD, so it does not alert the physician at the time of prescription. For this reason, an interventionist research was proposed in which the pharmacist, once the treatment is prescribed, having checked the patient GFR and reviewing the patient's medical history, establish the type of intervention to be carried out when it was convenient.
To evaluate the renal function, the predictive equation of the glomerular filtration rate MDRD-4 was used, whose calculation includes the concentration of Cr, sex, age and race. This method is recommended by SEN because of the greater diagnostic accuracy in elderly patients and filtration rates values between 15 and 60 mL/min/1.73 m2. It is one of the most used in clinical practice in this context, but it may become inaccurate in some situations, which is why other studies use Cockcroft's Gault equation8. Given the lack of the real value of Cr, the limitations in the use of these calculation based on Cr are known, which can be affected by many factors, such as malnutrition or dehydration.
The population is mainly elderly (average age between 67 and 89 years), with an average Cr value of 3 mg/dl and a glomerular filtration rate of 22.55±8.7 ml/min/1.73 m2. Higher creatinine plasma levels have been observed in men rather than in women, which agrees with Such Díaz et al.9,10.
During the research, 179 interventions were performed, with an acceptance rate of 58%, similar or slightly lower than others published, whose intervention rates ranged between 60-65%11,12. The high percentage of not accepted interventions can be explained by the context of patients with prerenal insufficiency, who have restored their blood volume, or in clinical situations with severe acute pathology. In the last case, it generates uncertainty for the prescriber, related to recommendations of dose-reducing, increasing the therapeutic interval or avoiding the drug, prioritizing the possible benefit or efficacy of the treatment rather than its toxicity10,13. Despite of this, a fair percentage of accepted interventions was obtained (53.8%) in patients with severe KD, G4 (15-29 ml/min/1.73 m2). However, no statistically differences were found between interventions accepted and renal impairment stage, so there is no greater number of interventions in patients with more severe KD, as it might be expected.
The analysis by therapeutic groups shows that three of them are those that concentrate greater number of recommendations, both realized and accepted: antibiotics, diuretics and antacids.
As it coincides with other authors, antibiotics include a large number of active ingredients susceptible to adjustment in KD. In the study of Such Díaz et al., levofloxacin includes the 19% of the interventions, and Arrabal Durán et al. also obtain the highest number of interventions in the antimicrobial group (57.5%)10,13,14.
In our case, meropenem, levofloxacin, amoxicillin-clavulanic acid and piperacillin-tazobactam were antibiotics with the highest number of interventions.
The second group with the largest number of interventions were diuretics. Similarly, in the study of Holm et al., furosemide was the third drug with the highest association with drug-related problems in patients with an average age of 78.7 year12.
Finally, the interventions carried out and accepted by clinical service were analyzed. The clinical service with the greatest number of both was General Medicine. This fact appears in the study of Arrabal-Duran et al. and Devesa García et al., which can be explained by a greater volume of polymedicated patients in this unit and where it is usual to manage antimicrobials13. With half of the interventions for this service, there is the Emergency Service, where the first evaluation and prescription take place for the patient. Other studies have focused exclusively on evaluating pharmaceutical intervention systems15. In third place, Geriatrics Service, although it has a lower number of interventions performed, has registered a greater increase in accepted ones (58.7%).
In order to know if there is an increase in the number of interventions both made and accepted in certain subgroup, they were analyzed by age group. No differences were found between the older population (over 80) and under 60 years old. They were also analyzed according to the administration route and no differences were found between oral and intravenous administration, being the latter more harmful for patients if recommendations are not made or accepted.
CONCLUSION
It has been observed in the results of this study, that a large percentage of patients with KD have required treatment intervention, being the population with G4 stage the most inteventioned. Particularly, more than half of these interventions have been accepted. In spite of this, pharmaceutical intervention stands out as a strategy to improve the population's pharmacotherapeutic quality taking into account the integration of assisted electronic prescription systems to facilitate a fast and immediate intervention in decision-making in these situations.
Conflicts of interest: The authors declare no conflicts of interest.