INTRODUCTION
Prescriptions for chronic medications are written with a limited number of refills allowed (e.g., ten) and expire within a state’s designated time frame (e.g., Colorado = 1 year, California = 2 years). Thus, patients may not realize that the prescription order for their chronic mediation has expired and/or has no more refills available. Pharmacists are allowed to use their judgment to dispense a short-term supply (tider) of a medication for a patient while a new prescription from the patient’s prescriber is provided.1,2 A tider is intended to allow a patient to continue taking her/his medication while awaiting the new prescription and, potentially, prevent poor health outcomes.
The tider phenomenon may be less prevalent in pharmacy settings that have an automatic refill system in place.3 With such a system, a prescriber or patient would be notified prior to the patient running out of medication so that a new prescription could be written. In a setting without a system in place, patients with an expired/no more refills available prescription may arrive at a pharmacy to find out that they are unable to receive any medication until a new prescription can be written. In this scenario, a tider may need to be provided to the patient.
Depending on the pharmacy setting, a tider is typically provided to the patient at no charge or as a loan that is “repaid” when the new prescription is prepared (e.g., a 27-day supply dispensed subsequently after the 3-day tider dispensing for the original 30-day supply prescription). If a tider is provided at no charge, a pharmacy that dispenses numerous tiders could be incurring substantial medication and dispensing costs.
Few studies have described the tider phenomenon. These studies reported the characteristics of patients who received a tider4,5, the tider medications dispensed4,5, and patients’ and pharmacists’ perceptions of tiders on medication adherence.6,7 These studies had either small sample sizes or were focused on the legal implications of providing a tider.4,5,6,7 Studies detailing the cost of tider medication dispensing and contrasting the characteristics of tider and non-tider patients and medications have not been reported.
The purpose of this study was to describe the rate of medication short-term supply dispensing (tider), patient and medication characteristics associated with a tider, and costs for tider dispensing in an integrated healthcare delivery system’s outpatient pharmacies in Colorado in the United States.
METHODS
Study Design and Setting
The study was a retrospective, observational study conducted at Kaiser Permanente Colorado. Tider prescription data from all Kaiser Permanente Colorado pharmacies were collected from its electronic, administrative pharmacy database during the first quarter of 2016. Patients were grouped by having had or not had a tider during any of the study months. A tider was identified as a 3-day supply of a study prescription medication that was dispensed at no charge to a patient.
Kaiser Permanente Colorado is a not-for-profit, integrated health care delivery system that serves over 600,000 members throughout Colorado’s front range and central mountains. Kaiser Permanente Colorado utilizes an electronic medical record that provides e-prescribing capabilities and owns and operates 28 medical clinics each with an outpatient pharmacy where its members can receive subsidized prescription medications. When presented with a tider request by a member, Kaiser Permanente Colorado pharmacy staff attempt to obtain a new prescription at the time of the request; however, they will provide a tider but will not charge for a tider nor make a loan of the medication when a new prescription cannot be obtained.
Coded and free-text medical, pharmacy, sociodemographic, and membership information from within the delivery system, as well as from other contracted and affiliated facilities, are captured in Kaiser Permanente Colorado’s administrative and claims databases. All aspects of this study were reviewed and approved by the Kaiser Permanente Colorado Institutional Review Board.
Study Population
Patients who had at least one prescription dispensed at an outpatient Kaiser Permanente Colorado pharmacy during the first quarter were included. Patients were excluded if their prescription was dispensed through mail order since the mail order pharmacy does not dispense tiders (i.e., patients can be dispensed a tider only at one of Kaiser Permanente Colorado’s 28 outpatient pharmacies). Patients were assigned to the observation group (Tider group) if they had at least one tider dispensed during the study months. Patients were assigned to the control group (Non-tider group) if none of their prescriptions dispensed during the study months was a tider. Medications that typically have only a 3-day supply (e.g., pain medications, muscle relaxants etc.) or dispensed in full amounts (e.g., vials, tubes, inhalers, etc.) were excluded because they are not dispensed as tiders or were unable to be determined if they were dispensed as a tider due to their potential short duration of use.
Study Outcomes
The primary outcome was the tider rate during the first quarter of 2016. Secondary outcomes included describing and contrasting the characteristics of tider medications against non-tider medications, the characteristics of tider patients versus non-tider patients, and the estimated annualized cost of filling and dispensing tiders.
Data Collection
Data were collected from Kaiser Permanente Colorado’s electronic, integrated, administrative databases. Information regarding tider and non-tider prescriptions and medication characteristics was obtained from the Kaiser Permanente Colorado pharmacy database. Information on patient characteristics was obtained from Kaiser Permanente Colorado’s data warehouse databases using International Classification of Diseases 9th and 10th revisions codes.
Patients were assessed in the first quarter of 2016 for a tider. For patients in the Tider group, the date of their first tider dispensing during the study months was considered their index date. For patients in the Non-tider group, the date of their first prescription dispensing during the study months was considered their index date. The pharmacy where the patient had their medication(s) dispensed on the index date was considered the index pharmacy. Information on patients’ benefit design, study medication, and demographic characteristics was collected as of their index date. Information on patients’ previous medication dispensing and comorbidities was collected during the 180 days prior to their index date. Medication costs were determined using National Drug Codes for dispensed tider medications to identify their wholesale acquisition cost or average wholesale price when a wholesale acquisition cost could not be found.
Data Analyses
No formal power calculation was performed due to the large sample size and its likelihood to produce statistically significant differences unless proportions/means were equivalent. Age was calculated as of the index date. Comorbidities were identified from inpatient stays, emergency department visits, and medical office visits. A chronic disease score, a validated measure of a patient’s burden of chronic illness, was calculated for each patient using outpatient prescription medication dispensing during the 180 days prior to the index date. The chronic disease score ranges in values from 0 to 36 with increasing values indicating a higher burden of chronic illness.8 The Quan adaptation of the Charlson comorbidity index was calculated from diagnoses that were recorded in the 180 days prior to the index date to provide a 30-point comorbidity score.9
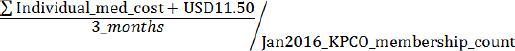
The overall tider rate was calculated by summing all tiders during the study months and dividing this value by the sum of all study medications that were dispensed during the study months. The rate and its 95% confidence interval are reported as percentages. The cost of filling and dispensing tiders was estimated by summing the wholesale acquisition cost (WAC)/average wholesale price (AWP) for each tider medication dispensed during the study period. In addition, an USD 11.50 dispensing fee was added per tider medication.10 The cost per member per month was estimated by:
Medication and patient characteristics are reported as means, medians, and standard deviations (SD) for interval-level data and percentages for nominal and ordinal data. Nominal and ordinal characteristics were compared with chi-square tests of association or Fischer’s exact test, as appropriate. Interval-level characteristics were compared by using either two-sample t-tests or Wilcoxon rank-sum tests, as appropriate.
RESULTS
A total of 444,225 medications for 135,907 patients for the study medications were dispensed during the first quarter of 2016. Of the 444,225 prescriptions, 3,430 (0.77%, 95%CI 0.75%:0.80%) were a tider. Of the 135,907 patients, 1,092 (0.8%) had at least one tider and 134,815 (99.2%) did not have a tider during the study period. The estimated cost of all tider medications during the study period was USD 20,633. The estimated total cost (i.e., medication cost plus dispensing fees) was USD 60,078. The mean cost of dispensing a single tider medication was approximately USD 17.50. These equate to an annualized total cost of USD 240, 312 with a per member per month cost of USD 0.03.
Tider medications were primarily generic (93.8%) (Table 1). Compared to Non-tider medications, Tider medications were more likely (1) to be generic (97.6% vs. 93.8%), (2) for chronic disease (96.9% vs. 89.7%), (3) formulary (95.9% vs. 90.4%), and (4) dispensed on a weekend (16.2% vs. 6.2%) (all p<0.001). The month with the highest rate of tiders was January (0.8% of all medications). There were statistically significant differences between the two groups across medication classes. The most noticeable differences between Tider and Non-tider medications were for endocrine and metabolic (16.9% vs. 19.4%), cardiovascular (41.9% vs. 32.7%), respiratory (0.1% vs. 3.5%), gastrointestinal (4.1% vs. 7.3%), central nervous system (17.2% vs. 20.0%), neuromuscular (7.4% vs. 4.9%), hematologic (3.6% vs. 2.4%) and miscellaneous (i.e., antiseptics, antidotes, diagnostic products, chemicals, adjuvants, and otherwise unclassified pharmacy products) (2.0% vs. 3.8%) medication classes (all p<0.001).
Table 1 Prescription medication characteristics overall and by tider status.
| Characteristic (n, %) | Overall (N=444225) | Tider prescription (n=3430) | Non-tider prescription (n=440795) | p-value |
|---|---|---|---|---|
| Generic medication | 416681, 93.8% | 3348, 97.6% | 413333, 93.8% | <0.001 |
| Chronic disease medication | 401802, 90.5% | 3322, 96.9% | 398480, 89.7% | <0.001 |
| Formulary medication | 430918, 97.0% | 3287, 95.9% | 427631, 90.4% | <0.001 |
| Requested on a weekend | 27810, 6.3% | 556, 16.2% | 27254, 6.2% | <0.001 |
| Dispensing Month | ||||
| January | 146459, 33.0% | 1207, 35.2% | 145252, 33.0% | 0.006 |
| February | 144184, 32.5% | 1043, 30.4% | 143141, 32.5% | 0.010 |
| March | 153582, 34.5% | 1180, 34.4% | 152402, 34.5% | 0.833 |
| Medication Class | ||||
| Cardiovascular | 145342, 32.7% | 1436, 41.9% | 143906, 32.7% | <0.001 |
| Central Nervous system | 88692, 20.0% | 589, 17.2% | 88103, 20.0% | <0.001 |
| Endocrine and metabolic | 85896, 19.3% | 581, 16.9% | 85315, 19.4% | <0.001 |
| Gastrointestinal | 32357, 7.3% | 139, 4.1% | 32218, 7.3% | <0.001 |
| Neuromuscular | 21650, 4.9% | 253, 7.4% | 21397, 4.9% | <0.001 |
| Miscellaneous | 16703, 3.8% | 70, 2.0% | 16633, 3.8% | <0.001 |
| Respiratory | 15551, 3.5% | 1, <0.1% | 15550, 3.5% | <0.001 |
| Genitourinary | 12320, 2.8% | 96, 2.8% | 12224, 2.8% | 0.927 |
| Hematologic | 10762, 2.4% | 125, 3.6% | 10637, 2.4% | <0.001 |
| Nutritional | 7095, 1.6% | 71, 2.1% | 7024, 1.6% | 0.027 |
| Analgesics and anesthetics | 7555, 1.7% | 69, 2.0% | 7486, 1.7% | 0.157 |
| Biological/Immunological | 302, 0.1% | 0, 0.0% | 302, 0.1% | 0.183 |
Overall, patients were primarily middle aged, female, and white race (Table 2). Patients in the Tider group were older (mean age 59.7 vs. 51.1, p<0.001), had a higher count of unique prescription medications dispensed during baseline (mean 4.1 vs. 3.9, p<0.001), had at least one previous tider dispensed (8.2% vs. 2.2%, p<0.001), been a Medicare beneficiary (47.5% vs. 30.4%, p<0.001), and had a higher burden of chronic disease (mean 3.6 ±3.1 vs. 2.4 ±2.9, p<0.001). Patients without a tider were more likely to be female (61.1% vs. 54.0%, p<0.001), of Hispanic ethnicity (16.4% vs. 11.8%, p<0.001), a new KPCO member (15.5% vs. 7.7%, p<0.001), a Medicaid beneficiary (9.4% vs. 6.4%, p<0.001), and have had a high deductible health plan (8.8% vs. 5.1%, p<0.001).
Table 2 Patient characteristics overall and by tider status
| Characteristic (n, %) | Overall (N=135907) | Tider patients1 (n=1092) | Non-tider patients2 (n=134815) | p-value3 |
|---|---|---|---|---|
| Mean age4 (SD) | 51.2 (19.3) | 59.7 (18.4) | 51.1 (19.3) | <0.001 |
| Female (n, %) | 82940, 61.0% | 590, 54.0% | 82350, 61.1% | <0.001 |
| White race (n, %) | 91240, 67.1% | 760, 69.6% | 90480, 67.1% | 0.082 |
| Hispanic ethnicity (n, %) | 22224, 16.4% | 129, 11.8% | 22095, 16.4% | <0.001 |
| Mean chronic disease score (SD) | 2.4 (2.9) | 3.6 (3.1) | 2.4 (2.9) | <0.001 |
| Mean Charlson comorbidity index (SD) | 0.7 (1.5) | 1.1 (1.8) | 0.7 (1.5) | <0.001 |
| Median family income (mean, SD) | USD 62932 (USD 64680, USD 23593) | USD 63438 (USD 65863, USD 24819) | USD 62891 (USD 64669, USD 23582) | 0.674 |
| Mean percent of household aged ≥25 years with at least some college education (%, SD) | 65.3% (18.3%) | 66.5% (17.8%) | 65.3% (18.3%) | 0.520 |
| At least one previous tider dispensing5 | 3067, 2.3% | 90, 8.2% | 2977, 2.2% | <0.001 |
| Mean count of unique prescription medications5 (SD) | 4.1 (4.0) | 5.5 (4.1) | 4.1 (3.9) | <0.001 |
| New member6 (n, %) | 20926, 15.4% | 84, 7.7% | 20842, 15.5% | <0.001 |
| Membership terminated7 (n, %) | 1190, 0.9% | 8, 0.7% | 1182, 0.9% | 0.611 |
| Medicaid beneficiary4 (n, %) | 12707, 9.4% | 70, 6.4% | 12637, 9.4% | <0.001 |
| Medicare beneficiary4 (n, %) | 41510, 30.5% | 519, 47.5% | 40991, 30.4% | <0.001 |
| High deductible health plan4 (n, %) | 11889, 8.8% | 56, 5.1% | 11833, 8.8% | <0.001 |
| HMO (n, %) | 132626, 97.6% | 1066, 97.6% | 131560, 97.6% | 0.943 |
| PPO health plan4 (n, %) | 390, 0.3% | 2, 0.2% | 388, 0.3% | 0.775 |
| Comorbidities8 (n, %) | ||||
| Atrial Fibrillation | 3707, 2.7% | 70, 6.4% | 3637, 2.7% | <0.001 |
| Benign prostatic hyperplasia | 3523, 2.6% | 50, 4.6% | 3473, 2.6% | <0.001 |
| Depression/Anxiety | 26772, 19.7% | 223, 20.4% | 26549, 19.7% | 0.547 |
| Diabetes mellitus | 17260, 12.7% | 179, 16.4% | 17081, 12.7% | <0.001 |
| Epilepsy | 1694, 1.3% | 34, 3.1% | 1660, 1.2% | <0.001 |
| Gastroesophageal reflux disease | 15221, 11.2% | 146, 13.4% | 15075, 11.2% | 0.022 |
| Hypercholesterolemia | 2935, 2.2% | 25, 2.3% | 2910, 2.2% | 0.767 |
| Hypertension | 29987, 22.1% | 334, 30.6% | 29653, 22.0% | <0.001 |
| Hyperthyroidism | 438, 0.3% | 3, 0.3% | 435, 0.3% | 1.000 |
| Hypothyroidism | 10782, 7.9% | 114, 10.4% | 10668, 7.9% | 0.002 |
| Parkinson’s | 443, 0.3% | 12, 1.1% | 431, 0.3% | <0.001 |
| Transplant/ immunosuppression | 594, 0.4% | 9, 0.8% | 585, 0.4% | 0.052 |
1- Patients had at least one tider dispensing between 1/1/2016 and 3/31/2016
2- Patients had no tider dispensing between 1/1/2016 and 3/31/2016
3- Value is for the statistical test of between Tider and Non-tider group difference
4- As of the index date. For tider patients, index date is the date of the first tider dispensing between 1/1/2016 and 3/ 1/2016. For non-tider patients, index date is the date of the first prescription dispensing between 1/1/2016 and 3/31/2016.
5- Dispensed during the six months prior to the index date
6- Joined KPCO during the six months prior to the index date
7- During the 30 days after the index date
8- At least one diagnosis recorded during the six months prior to the index datePPO - preferred provider organization; SD - standard deviation
DISCUSSION
In our retrospective analysis of short-term medication supplies dispensed at 28 outpatient pharmacies, we identified a tider rate of 0.8% of study medications. Our findings appear to be the first large-scale assessment of the tider phenomenon. While 0.8% is a somewhat low percentage of all study medications dispensed, a tider was dispensed for one in every 125 patients who had a study medication dispensed during the study period. We estimated the total tider cost implications to be USD 0.03 per member per month and USD 17.50 per tider. We identified no other studies that have estimated this cost. Loaning the patient the tider does not appear to be cost-effective as the cost of dispensing a tider is primarily related to the dispensing fee not the medication. Nevertheless, the total cost of dispensing a tider appears reasonable since the benefits of providing patients with needed medications likely outweigh the cost. For example, a patient with epilepsy who requires an anticonvulsant medication but has no more refills available requests a tider. By receiving the anticonvulsant tider, the patient may not experience a seizure that would limit his/her ability to work, drive, etc.11
Published peer-reviewed information on tider rates were not identified. O’Neil and colleagues reported that 67% of 243 pharmacists from Greater London and Southeast England who were surveyed responded receiving at least one request monthly for an emergency supply of a prescription medication in 1998.5 Morecroft and colleagues reported from their clinical audit of 22 pharmacies in Northwest England that 450 patients had requested an emergency supply of a prescription medication during a 4-week time period in 2013.4 Neither of these studies’ results readily are comparable to our findings as they do not report the denominator of prescriptions dispensed during the study period. It may be that the denominator date were not available or difficult to obtain.
This study assessed a wide array of patient characteristics for their association with a tider. The most striking characteristics associated with the patients who had a tider that we identified included having been older, male, a Medicare beneficiary, and having had a previous tider dispensing and a higher burden of chronic disease. O’Neil and colleagues reported that elderly patients most frequently requested an emergency supply of a prescription medication.5 Similarly, Morecroft and colleagues reported that older patients more frequently requested an emergency supply of a prescription medication.4 In addition, Morecroft and colleagues in their pharmacists’ survey reported that patients having forgotten to re-order their prescription in a timely manner, delays in prescriber providing the prescription, and the pharmacy not having medication available when patient presented previously were reasons that patients requested a tider.4 No other studies were identified that assessed patient characteristics associated with a tider or reasons why patients requested a tider.
This study identified that medication characteristics most prominently associated with a tider included the cardiovascular and neuromuscular medication classes. Additionally, tiders were more likely to be dispensed on a weekend. O’Neil and colleagues reported that patients most commonly requested an emergency supply of respiratory, cardiovascular, and central nervous system medications.5 Morecroft and colleagues reported that patients most commonly requested an emergency supply of cardiovascular, respiratory, and endocrine medications and a high proportion of requests around the weekend.4 While we identified high rates of cardiovascular and endocrine tider dispensing, we identified relatively few respiratory (i.e., decongestants) tider dispensing since these medications are not dispensed as tiders at Kaiser Permanente Colorado.
Limitations
While our study provides important information on medication and patient characteristics of tiders, there are limitations to our study. It was conducted in one integrated health care delivery system with its own pharmacies. Other systems and their pharmacies (e.g., network pharmacies) may not have the same experience with tiders. We did not survey patients to identify reasons why they required a tider. Any small difference detected would likely be statistically significant because of the large sample size. We may have under estimated the tider rate as some medication classes were excluded due to our inability to determine tider status administratively. We did not assess the impact of tider dispensing on health outcomes (e.g., medication adherence).
CONCLUSIONS
One out of every 125 patients had at least one tider during the first three months of pharmacy prescription dispensings at an estimated cost of USD 0.03 per member per month. Patients who had a tider were more likely to be older, male, a Medicare beneficiary, and having had a previous tider dispensing and a higher burden of chronic disease. The tider medication was more likely to be a cardiovascular or neuromuscular medication class and more likely to be dispensed on a weekend. The mean total cost of dispensing a single tider, including the medication cost and dispensing fee, was approximately USD 17.50. This cost appears reasonable since the benefits of providing patients with needed medications likely outweigh the cost. Future intervention studies (e.g., a system that alerts a patients that she/he has no more refills of a chronic medication, automatic prescription refilling) should be performed to assess the impact on the rate of tider dispensings and health outcomes.