Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Sanidad Militar
versión impresa ISSN 1887-8571
Sanid. Mil. vol.68 no.1 Madrid ene./mar. 2012
https://dx.doi.org/10.4321/S1887-85712012000100011
The uses of epidemiologic and public health approaches for HIV/AIDS control among young men in the Royal Thai Army and Thailand
Actuaciones epidemiológicas y de salud pública para el control del VIH/SIDA entre los hombres jóvenes en Tailandia y el Real Ejército de Tailandia
Saengdidtha B.1, Rangsin R.2, Kana K.3, Kaoaiem H.4
1 Col. Army Institute of Pathology.
2 Col. Phramongkutklao College of Medicine
3 Col. Armed Forces Research Institute of Medical Science.
4 Ltc. Royal Thai Army Nursing College
Phramongkutklao Medical Center, Royal Thai Army Medical Department, Bangkok, Thailand.
SUMMARY
The effectiveness of HIV/AIDS control in Thailand is well recognized internationally and is due to the perception of national threat, the acknowledgement of the policy-makers, the efficient mechanisms of management at all levels, the relevant counter-measures and plans, the sustained commitment in the fight against HIV/AIDS and the total mobilization of all sectors of the country to deal with the problems. The Royal Thai Army (RTA) and the RTA Medical Department (RTAMD) have significant roles in solving the HIV/AIDS problems by partnering in the threat assessment, surveillance among conscripts to monitor HIV spread and control it effectively, research on behavioral risks leading to the development of targeted intervention models first piloted with conscripts and later adapted for other risk groups, providing care and support to people living with HIV/AIDS (PWA) and cooperation with civilian and international partners. Factors that have contributed to the success of the RTA's operations include the strong organizational infrastructure and management, the relevant strategies and measures, the determination for long-term commitment and total mobilization of resources and multi-sectoral coordination. The lessons learned from the RTA's experience in HIV/AIDS prevention and impact alleviation, especially by epidemiologic and public health approaches, can be used as a basis for further development towards more effective and efficient models. It can also be a useful example for other agencies in Thailand and other countries with the same problems and similar socio-cultural backgrounds to apply and adapt for their own uses.
Key words: HIV/AIDS, Thailand, Public health, Epidemiology, Royal Thai Army, Young men.
RESUMEN
La eficacia del control del VIH/SIDA en Tailandia es bien conocida a nivel internacional y se debe a la percepción de amenaza nacional, el reconocimiento de los encargados de formular las medidas políticas a adoptar, los mecanismos eficientes de gestión a todos los niveles, las correspondientes contramedidas y planes, el desarrollo sostenido del compromiso en la lucha contra el VIH/SIDA y la movilización total de todos los sectores del país para hacer frente a este problema. El Ejército Real Tailandés (RTA) y el Departamento Médico del RTA (RTAMD) han desarrollado un papel importante en la solución de los problemas del VIH/SIDA mediante la evaluación de la amenaza, la vigilancia sobre los soldados para controlar la propagación del VIH y su control de manera efectiva, la investigación sobre comportamientos de riesgo, que propicien al desarrollo de modelos de intervención, dirigidos primero a los soldados y más tarde adaptado para otros grupos de riesgo, proporcionando atención y apoyo a las personas que viven con el VIH/SIDA (PVVS) y la cooperación con entiddaes civiles e internacionales. Los factores que han contribuido al éxito de las operaciones de la RTA incluyen la sólida infraestructura de organización y gestión, las estrategias y medidas, la determinación de compromiso a largo plazo, la movilización total de los recursos y la coordinación multisectorial. Las lecciones aprendidas de la experiencia de la RTA en el VIH/SIDA y la reducción de sus consecuencias, sobre todo mediante enfoques epidemiológicos y de salud pública, se pueden utilizar como base para un mayor desarrollo hacia modelos más eficaces y eficientes. También puede ser un ejemplo útil para otras agencias en Tailandia y otros países con los mismos problemas y similares contextos socio-culturales donde poderlos aplicar y adaptar para su propio uso.
Palabra clave: VIH/SIDA, Tailandia, Salud pública, Epidemiología, Ejército Real Tailandés, Hombres jóvenes.
Introducción
Thailand was one of the most severely affected countries during the early stage of the HIV/AIDS pandemic. The first AIDS patient was reported in 19841 and epidemic HIV infections were first recognized in 1988, but increased dramatically in the 1990s, primarily as a result of sexual transmission2. However, the country openly addressed the problems and implemented strict and continuous preventive measures. The Ministry of Public Health (MOPH), in cooperation with governmental and nongovernmental organizations, instituted programs, including condom promotion, and massive health education to prevent HIV transmission. These measures have been well recognized for their effectiveness in reducing the cumulative number of HIV infections from the previously estimated number of 6-8 million infected by the year 20003 to a more recent computerized projection of 1 million infected people. The number of new infections in 2010 is estimated to be around 11,000 per year4, down from the estimated annual figure of over 100,000 persons. The course of HIV epidemic has been decreased dramatically since its peak in the early 1990s. The success of Thailand's HIV control has been internationally acknowledged5-6.
By acknowledging that HIV/AIDS could pose a major problem to Thai society and national security, the Thai authorities have raised the awareness of the whole nation. The perception of HIV/ AIDS as a threat to national security has made it justifiable to mobilize all national resources to nullify the threat. The success of the Thai HIV/AIDS control programs can be directly attributed to its multi-sectoral approach that has drawn upon the country manpower, funds, equipment, knowledge, expertise and national will. It has created a sense of responsibility in every sector, and has led to the concept that HIV is not only a public health problem but also the problem of every person and all sectors of the country.
The military is an agency with several intrinsic characteristics that can be used to carry out an HIV control operation effectively and efficiently. These characteristics include a strong and unified command hierarchy, rapid situational analysis and response, basic organizational infrastructure, organizational readiness for disease surveillance and control and recent experience in dealing with communist insurgency in 1965-1983 which Thai officials learned how to mobilize different sectors to fight against a threat to national security.
Thailand has established HIV surveillance among around 60,000 army conscripts annually. It is believed to be the nationally representative sample of young Thai men of 21 years of age, estimated more than 250,000. This ongoing total survey is helpful to be studied for the changes of risk behavior pattern in this risk group. The body of knowledge gained from epidemiological studies regarding HIV among the RTA personnel has provided an understanding of the dynamics of the HIV epidemic in Thailand. Moreover, the use of public health approaches of successful behavioral change interventions in the RTA provide valuable lessons that can be applied in other population groups engaging in risky behaviors. Additionally, the RTA personnel who have been trained in the HIV programs such as peer educators and counselors will be useful for their communities when they re-enter civilian life.
This case study focuses on the experiences of the RTA in HIV/AIDS control over the past two decades. Many lessons can be learned from these experiences and its significant contribution to the response to HIV/AIDS in Thailand. It also documents the processes and strategies, especially, the epidemiologic and public health approaches the RTA medical personnel have used to achieve a sustained decline in HIV prevalence within its conscripts, and outlines the HIV/AIDS policies, programs, research and development used to achieve these results. It shows the efforts of the RTA forces which back up the success of the country in HIV/AIDS control7-8.
HIV/AIDS Epidemic in Thailand
The first AIDS case of Thailand was reported in1984 in a man returning from abroad. In response to the epidemic, the MOPH of Thailand had included AIDS in the lists of notifiable communicable diseases since 1985. This requirement was dropped in 1991 and has been replaced by sentinel surveillance since June 1989. This epidemiologic activity was initially started twice a year in a few provinces, then expanded nationwide in 1991 and has been reduced to once a year since June 1995.
Findings from the surveillance and some research studies have provided a full picture of the HIV/AIDS epidemic, which can be divided into 6 stages2,4: 1) the epidemic began with the transmission among men who have sex with men (MSM), during the period from 1984 to 1987; 2) the spread of HIV into injecting drug users (IDU) was detected in 1988, with 15.6% of those surveyed in March found to be infected, compared to 1-2% in 1987 and the prevalence has been raised over 30% since mid-1988; 3) HIV began to spread into female commercial sex workers (FSWs) with rapidly increased prevalence from 0-0.4% in Bangkok, Chiang Mai and Pattaya in 1988, to 44% in a survey in Chiang Mai in June 1989; 4) the spread of HIV to the men frequenting sex workers who attended sexually transmitted disease (STD) clinics, began to be apparent in 1990; 5) HIV was found to have spread to housewives and 6) HIV infection was found in the newborns of HIV-infected mothers.
HIV/AIDS problems in the RTA
It had been widely accepted that conscripts in the RTA were one of the groups at high risk of HIV infection9-10. When there was a reported spread of HIV in the country, the RTA carried out an immediate assessment of the HIV situation among its personnel. The first case of HIV infection was detected in army conscripts in 1987. The continuing assessment of HIV prevalence among army conscripts since 1989 has revealed increasing trends from 0.5% at the onset, to a peak of 4% in 1993, followed by a gradual decline to less than 1% in May 2003. These data, obtained primarily from 21-year-old conscripts, is a clear indicator of the general HIV situation in the country7.
The RTA became seriously concerned about the consequences of HIV/AIDS when the virus began to spread among men frequenting sex workers in 1990 and, gradually, among the general population and young people. The following impacts were identified: 1) the military preparedness of the RTA has suffered as a result of HIV/AIDS; 2) there is a psychological effect, due to the anxiety and discrimination; 3) there are additional burdens for the medical and social services in the RTA; 4) field medical services personnel are at risk of contamination from HIV-positive persons' blood and body fluids; and 5) screening for deployment for overseas missions is more complicated and time-consuming for groups at risk of contracting HIV. Over time, the HIV epidemic has resulted in economic, psychosocial and political instability in Thai society.
Response to HIV/AIDS Problems
The first group of people to call for serious prevention and solution measures for HIV/AIDS were medical and public health personnel who witnessed the problem first-hand. HIV/AIDS were considered to be communicable diseases and the MOPH was responsible for these problems. This was reflected by the appointment of the Director of Communicable Diseases Control Department as the chairman of the National AIDS Committee. As a result, HIV/ AIDS awareness was mostly confined to the medical and public health fields, and awareness and prevention campaigns were quite limited.
At the first period of the epidemic, HIV/AIDS was perceived as a confidential issue. For fear of affecting tourism and the country's image, there were only limited concrete campaigns or efforts to educate the public. Moreover, surveillance activities were inadequate and did not accurately reflect the threat. During this phase, it was believed that the HIV and AIDS problems were not serious, and that existing communicable disease control measures were sufficient to cope with the problems. This made Thailand miss the opportunity to prevent the spread of the epidemic in its early stages.
In the period of 1987 and 1990, the HIV situation was clearer. The epidemiological information was made available by the MOPH, the danger of HIV/AIDS was fully recognized and the need for an effective response to solve the problem was acknowledged. There were attempts to search for effective epidemiological and problem-solving interventions. The obvious action to be taken at this stage was the dissemination of HIV/AIDS information to the public, based on the assumption that greater awareness would encourage people to avoid engaging in risky behavior. However, there was insufficient information and a tendency among the general public to be hostile towards, and discriminate against people living with HIV/AIDS (PWA). As the epidemic of HIV/AIDS in the North was the most critical, governmental and nongovernmental organizations in the region were fully alerted to tackle the problems. Although these campaigns resulted in increased public knowledge of HIV/AIDS, there were some adverse consequences. People were frightened of infection, and infected persons were discriminated against, while the practice of risky behaviors remained almost unchanged. For the RTA, HIV interventions during this phase took the form of both top-down policy implementation from the RTAMD and the Ministry of Defense (MOD), and bottom-up strategy development. Using the top-down approach, the Royal Thai military had established HIV control committees at ministerial and periphery levels to take action in accordance with the national HIV/AIDS policy.
In the period of 1991-1996, HIV prevention and impact alleviation programs were concretely and effectively carried out at the national level and by the RTA. The main theme of the response was a clear message that HIV was a threat to national security. Strategies were clearly formulated and they became the key to unified efforts to resolve the problem. For the RTA, the bottom-up approach implemented by Fort Naresuan and Fort Kawila Hospitals was adopted and adapted, and effectively integrated into the top-down policy of the central leadership. Some good examples of this include the application of a peer education's model; the research and development programs by the Armed Forces Research Institute of Medical Sciences (AFRIMS) in Prachuab Khiri Khan Province; the risk assessment scale for targeting high risk conscripts for HIV prevention11; and the policy formulation regarding PWA.
The Asian economic crisis during the period of 1997 and 2002 had halted and, in some cases, terminated many HIV/AIDS prevention and impact alleviation programs. There was a need to review past operations in order to remain focused on the positive achievements of existing programs. With the recovery of the economy, existing operations were re-evaluated and renewed in order to improve prevention and impact alleviation measures.
Roles of the RTA in HIV/AIDS control7-8,12-13
When AIDS patient was firstly reported, it was an emerging disease. Health personnel usually use the epidemiologic and public health measures for prevention and control of the diseases. The epidemiologic methods include identification of host, agent and environment; survey of knowledge, attitude, practice and risk behavior of at-risk people; surveillance for cases, prevalence and incidence of the diseases. The public health measures are health education, immunization, nutrition, sanitation, risk reduction, using protective devices or barriers, etc. For HIV/AIDS prevention and control at that time, the appropriate methods were education and risk reduction.
The operation of RTA for the HIV/AIDS battle was originated by the Preventive Medicine Division (PMD) of the RTAMD before HIVinfected personnel was reported in the RTA. The first RTAMD Declaration of "Prevention and Control of HIV/AIDS in the RTA" was proposed by the PMD and signed by the Surgeon General of the RTAMD in 1987. Then, HIV/AIDS education was started among RTA personnel and families. Then, the PMD organized the "Preventive Medicine Seminar in the RTA" in 1988 and the topics of HIV/AIDS was included.
After HIV/AIDS epidemic was detected in the RTA, the PMD acted in various roles as follows: 1) working as member and secretary of AIDS control committees of RTAMD, RTA, Ministry of Defense, and member of National AIDS Subcommittees; 2) performing education campaigns, producing the videos of "AIDS: the Serious Threat of the RTA" in 1989 and "AIDS: the New Killer" in 1992, collecting and producing other HIV/AIDS education material for distribution to the RTA units, and setting mobile education teams for RTA personnel and families in remote areas; 3) developing plans, preventive programs and budget; 4) developing surveillance systems; 5) evaluation of control programs; 6) facilitating HIV researches; and 7) training of personnel, i.e., leaders, educators, counselors, physicians, nurses and others for HIV/AIDS care.
The RTA and the RTAMD have actively been performing roles and functions in full compliance with the national policy on HIV/AIDS prevention and impact alleviation. Such roles include development of national policy and programs, monitoring of the national HIV/AIDS situation, implementation of HIV prevention programs, provision of care and support to PWA, promotion of research and national and international coordination and collaboration on HIV/AIDS.
Role of the militaries in developing national HIV/AIDS prevention and impact alleviation policy and programs14-18
1. The National Committee on AIDS Prevention and Alleviation
The National Committee on AIDS Prevention and Control was established in 1984, and has undergone many revisions. Since the 1991 revision, the Prime Minister has been appointed to be the Chairman. Committee members include representatives from all ministries, many governmental agencies, nongovernmental organizations, the private sectors and PWA. The committee has developed many national plans since 1992. Participation of the MOD in the National Committee has provided a good opportunity for the military sector to take part in the development of national HIV/AIDS policy, as well as providing advice on appropriate HIV/AIDS approaches in the military and the establishment of military strategies and interventions that are in line with the national policy.
2. The RTAMD Committee on HIV/AIDS Prevention and Control
In 1989, a Committee on HIV/AIDS Prevention and Control was set up in the RTAMD. Activities of this committee included the working and the implementing body on HIV/AIDS of the RTA, HIV screening of the army conscripts since 1989 and formulation of army policies on HIV/AIDS. The policies include the scopes of prevention(promote awareness of the risks of HIV and reduction HIV risky behavior, move forward more strategically and steadily, encourage the use of condoms, particularly among conscripts), HIV case detection and care-provision (provide voluntary HIV counseling and testing service in medical units, reserve the rights to refuse recruitment of HIV-positive persons into the RTA, support measures for caring PWA to enable them to resume their normal life), medical care (promote fair and humane conduct towards HIV-infected personnel, improve the capacity of medical personnel in AIDS treatment and care), cooperation with other agencies (promote cooperation between units of the RTA and other governmental and nongovernmental organizations on problem-solving measures relating to HIV/AIDS and promote international cooperation on HIV prevention) and research (promote research and development in measures to resolve HIV/AIDS problems).
3. Committee on AIDS Prevention and Control of the MOD
In 1991, the Committee on AIDS Prevention and Control was established in the MOD. This committee was set up to undertake the following activities: 1) formulate HIV/AIDS policies for the MOD; 2) organize study tours for HIV/AIDS control activities in military population in the United States and United Kingdom; 3) organize HIV/AIDS seminars for military personnel; 4) monitor and evaluate HIV/AIDS programs in the military.
4. Committee on AIDS Prevention and Control of the RTA
In 1994, the committee on AIDS Prevention and Control was set up in the RTA to be responsible for the following activities: 1) implement a course of action corresponding to the national HIV/ AIDS prevention and impact alleviation policy, as well as to the order issued by the Defense Ministry, which required all top-ranking officials under the Ministry of Defense to be responsible for HIV prevention and control and to set up working committees on HIV/AIDS. This policy was a top-down approach in a multi-layered operational management system to establish AIDS committee and plan at all administrative levels; 2) assign HIV/AIDS-related activities as a responsibility of the Personnel Directorate; 3) support the goals set by the AIDS Committee of the RTAMD, in addition to the nationaland central-level policy formulation. There have been representatives of the RTAMD participating in all levels of AIDS committees, and the RTA units in the field have also been actively participating in the multi-sectoral response to prevent and alleviate HIV/AIDSrelated problems at the local level.
Role of the RTA in monitoring the national HIV/AIDS situation
1. HIV surveillance among army conscripts19-22
Recruitment of Thai men occurs in April every year and they will work for 2 years in military service. Placement takes place twice a year in May (group 1) and November (group 2). The AIDS Control Committee of the RTAMD decided to conduct HIV testing among all new army conscripts to assess the HIV epidemic and assign them to appropriate jobs and the participating units were the Army Institute of Pathology (AIP), the AFRIMS of the RTAMD and RTA medical units. The AIP and the AFRIMS have conducted so by enzyme-linked immunosorbent assay (ELISA) with Western Blot confirmation since 1989. Demographic data have been additionally collected since 1991. Data from this measure are useful in planning of the RTA reserve, workforce administration, and the arrangement of counseling services for the affected persons. In the beginning, it was found that the HIV epidemic in the North was the most critical. In 1993, HIV prevalence rate in conscripts was found to be as high as 4%. The situation improved after all concerned sectors undertook HIV preventive programs. At the same time, HIV prevalence in most regions was gradually declining and the average prevalence rate fell to 0.7% in 2002. From 2004 to 2010 the rate of HIV infection has declined and stable at 0.5%20 (Fig. 1). Surveillance was conducted as a total survey, not through a random sampling process. Therefore, the data obtained are highly valid. The MOPH and many agencies have utilized these data as an indicator to monitor the HIV situation and trends at both regional and national levels particularly the situation among young men who are considered to be at high risk of contracting HIV from sexual and drug addictive activities. The reduction of HIV prevalence among RTA conscripts is a good indicator of the success of HIV prevention programs in Thailand.
2. Behavioral surveillance among conscripts12,21-24
In 1991, the PMD of the RTAMD began surveillance among a sample of 400 army conscripts in Bangkok and expanded surveillance to nationwide in 1992. In collaboration with the Epidemiology Division of the MOPH since 1995, the sample size has become 5,000 per year. It was found that the condom use rate with FSWs has increased from 34% in 1992 to more than 80% in 2001. In Bangkok, the rate increased significantly from 26% in 1991 to more than 85% in 2010. But it should be kept in mind that the conscript risk behavior is not stable. Then there should be monitoring system for their risks for the success of HIV control.
3. Surveillance of STDs among RTA conscripts12,21
The PMD of the RTAMD has collected reports on STDs from treatment units within the army since 1991 to monitor the trend of these diseases as an indicator of the extent of the spread of HIV. It was found that this rate decreased from 150 per 100,000 in 1993 to fewer than 10 per 100,000 since 1997.
4. Surveillance of HIV/AIDS patients among RTA personnel12
The PMD of the RTAMD has collected reports on HIV and AIDS patients in the RTA from the medical units across the country since 1987 to obtain data for the preparation of HIV/AIDS-related care. Since 1991, when reporting of HIV diagnoses was no longer required by law, the reports have covered only AIDS patients. This is the passive case-reporting system used by the MOPH, and the same type of form is used. The data are summarized monthly and annually, showing the number of cases receiving services from the RTA medical care facilities.
5. Knowledge, attitudes and behavior survey of HIV/AIDS in the RTA12
In 1993, the PMD of the RTAMD conducted a survey on the knowledge, attitudes and preventive practices among 1,002 RTA personnel. It was found that over 70% had been informed about HIV/AIDS from the RTA medical officers. More than 75% had accurate knowledge about HIV/AIDS and more than 55% consistently used condoms in extra-marital sex. The PMD had also collaborated with the Sub-committee on Research and Evaluation of HIV/AIDS Prevention and Control of the RTAMD and AFRIMS in the evaluation of the RTA HIV control campaigns. In the followup to the repeated research activities, it was found that most RTA personnel at all levels had a good level of knowledge. However, the attitudes and preventive practices were still not satisfactory, especially among young male personnel. The rate of condom use remained at 70% or lower, requiring a continuous campaign against risky behavior.
Role of the RTA in providing care and support to PWA12, 21-22
Located across the country, the 36 Fort hospitals have been active in providing care to PWA not only to those in the RTA but also to their families and the general public. The services provided are counseling, diagnosis and treatment, in accordance with the MOPH guidelines.
The RTAMD initially ruled that conscripts found to be infected with HIV would be discharged with consent from their superior and physician. RTA personnel found to be HIV-infected or suffering from AIDS would receive counseling and symptomatic treatment. However, a revised policy was adopted in 1991 when more cases of HIV infection were found. The policy stated that any RTA personnel who contracted HIV from sharing drug-injecting equipment or any conscripts requiring hospitalization would be dismissed from the RTA, while those who contracted HIV in other ways would receive care in the RTA hospitals, or resume normal duty, with adjustments, if necessary. In 1998, another guideline was issued with regard to the assignment of work to HIV positive personnel that would not be physically or psychologically stressful. In the beginning, psychiatrists had been solely responsible for providing counseling on HIV/AIDS. When additional budgets on HIV/AIDS were allocated to the RTA in 1992, the RTAMD organized regular three-day training course for counselors. Those who attended were doctors, nurses, social workers and officers. The trainees were assigned to provide counseling services in their workplaces. In 1993, the course was developed into a five-day training session. Since 1992, antiretroviral medication has been provided for HIV-infected personnel and AIDS patients in the RTA medical facilities.
Role of the RTA in promoting HIV/AIDS research25-27
In 1991, the AFRIMS, in cooperation with Walter Reed Army Institute of Research, USA, started a project to conduct research on HIV/AIDS in the areas of epidemiology, virology and HIV/AIDS vaccine development, with an understanding that AFRIMS would concurrently receive assistance for personnel and infrastructure development. AFRIMS, in collaboration with the US Army, took a leading role in AIDS vaccine development in Thailand. The RTA undertook this project because its conscripts were considered one of the high-risk groups and HIV screening tests had already been administered at the time of enlistment. Hence, the epidemiological study of HIV infection among this group was already underway.
HIV/AIDS control programs for young men in the RTA
From the widespread campaigns to disseminate information on HIV/AIDS in 1989-1990, it was found that the RTA personnel had better knowledge of HIV/AIDS than before, while their attitudes and behavior still needed improvement29-31. Faster and more effective measures needed to be identified to curb their risky behavior. Two operational research projects were initiated in RTA forts in 1991-1994, one in Phitsanuloke and the other in Chiang Mai. Both models had conscripts as target groups and adopted the same peer education or friend-help-friend approach. In Chiang Mai, high-ranking officers up to the battalion level were assigned specific roles to support the project. The Phitsanuloke model only had a peer education component, without the knowledge and understanding of superior ranking personnel. The two models were later adjusted and incorporated into a third project in Prachuab Khiri Khan, where the involvement of the division level was added. This focus group approach has been well accepted by many expert groups, and has been applied to other target groups, such as teenagers in schools and workers in factories.
The fight against AIDS among army conscripts in Chiang Mai9,32
Fort Kawila Hospital, in Chiang Mai, had organized special HIV/AIDS talks by experts, set up exhibitions and worked with small groups since 1987. In 1993, the hospital cooperated with academic institutes conducting a project entitled Social Mobility, Sexual Behavior and HIV in Northern Thailand, or SOMSEX, aimed at curbing risky behavior among conscripts who had been with the RTA for two years. The project involved 3 stages: 1) In the first six months, a behavioral study was conducted, giving training to squad leaders, field medics, chaplain, non-formal-education teachers and conscripts with conducting in-depth behavioral interviews with conscripts. It was found that the conscripts did not have knowledge or clear understanding about HIV/AIDS; excessive consumption of alcohol led to brothel visits and unsafe sex; some conscripts used condoms, but incorrectly and inconsistently; and conscripts who had contracted an STD did not always obtain appropriate treatment; 2) In the subsequent 18 months, activities were organized to change the risky behavior of the conscripts. From the data gathered, workshops on knowledge, and attitude development towards HIV/AIDS were given to those who were influential with conscripts. Duties were specifically assigned according to rank, as follows: squad leaders as superiors and advisers; field medics as health supervisors; chaplains or assistants as advisors on morale, etiquette and quality of life; non-formal-education teachers as instructors; and conscript leaders as trainers. 3) From the evaluation after two years of operation, it was found that the conscripts had reduced their risky behavior after repeated exposure to HIV/AIDS information and the incidence of HIV subsided significantly, with no new cases reported.
The development of the friend-help-friend campaign in Phitsanuloke33,35
The friend-help-friend campaign against HIV/AIDS in Fort Naresuan, Phitsanuloke was designed to rapidly reduce risky behavior among the target groups. This was in response to an evaluation of the large-scale information dissemination begun in 1989, which showed that, although the level of knowledge improved satisfactorily among the target groups, behavior did not. Therefore, Fort Naresuan Hospital started to use a qualitative research technique of in-depth interviews and focus-group discussion with conscripts enlisted in May 1991. The results showed that conscripts needed a clear channel of information that was easy to understand, non-threatening and coming from someone they could trust. With these findings, the friendhelp-friend campaign was designed to provide practical knowledge to conscripts so that they become aware of HIV risks and can be effective in helping to prevent further spread of the virus. This will make the project be sustainable and replicable in other forts. The first component of this project was to select suitable conscripts to be instructors. The second component was to design a program to educate these leaders and build up the right attitude and skills to transfer their knowledge to others. The last component was to provide these peer educators with full support. This project was piloted and subsequently evaluated in June 1994. Its success allowed for scaling-up, beginning with the training of primary instructors who would train local RTA personnel as secondary instructors to train the conscripts. The model was prepared for nationwide implementation.
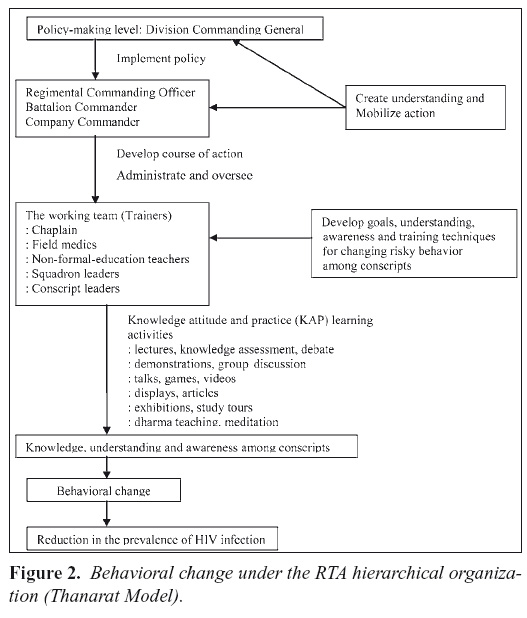
The thanarat model on behavioral change operations among conscripts36
The Thanarat Model was used in setting up activities to promote knowledge of HIV and its prevention to the conscripts in Prachuab Khiri Khan province. The format used in these activities was derived from the SOMSEX and friend-help-friend projects, both of which had conscripts as main targets. Moreover, it relied on the influence of the organization personnel structure and the RTA administration as key factors in behavioral change. The influential personnel were field medics, squadron leaders, chaplains and non-formal-education teachers. These peer educators had an important role, as they understood the behavior and problems their peers might be experiencing. In this model, the peer educators mainly worked to support influential RTA personnel. This model recognized the RTA command structure and administrative hierarchy was crucial to the success of the operation and policy implementation set by the MOD regarding the duties of its personnel and of the armed forces in HIV prevention and control (Fig. 2). The results of the projects showed the reduction in risky behaviors, i.e., fewer visits to sex workers, reduced alcohol drinking, and increased use of condoms. HIV screening of conscripts to assess the model's effectiveness revealed that the conscripts had a lower HIV incidence. No new infections were detected in their last six months of duty. This confirmed the success of the project in reducing the risky behaviors of the conscripts.
Research programs
There were a lot of research programs in the prevention and control of HIV/AIDS among army conscripts and Thai young men in the areas as follows: 1) peer education and counseling37, 2) prevalence studies and trends38-41, 3) incidence studies42-43, 4) natural history of HIV44-45, 5) risk factors, risk scale, risk behaviors and trends11,46-59, 6) education and prevention programs60-63, 7) co-infection64-65 and knowledge, attitude and practice66-67.
The benefit of HIV testing among Thai Army conscripts68-69
The conscripts who participate in HIV testing will be counseled, know their HIV serostatus and can plan to consult the physicians to check their conditions for appropriate highly active antiretroviral therapy (HAART) in case of HIV infection. This can prolong their lives and healthy conditions. In the present time, there is a prevention strategy of 'test and treat' that promotes HIV testing and initiating antiretroviral therapy (ART) upon HIV infection diagnosis to reduce HIV transmission. This method is believed to be able to eliminate the HIV epidemic and reduce ART costs in the long term.
Conclusion
The achievements of the RTA in HIV/AIDS control have been internationally recognized. Factors contributing to the RTA's success include the perception of the HIV/AIDS threat to the national security, commitment of policy-makers to finding solutions of the problems, strong organizational structure and management, implementation of effective strategies and measures, demonstration of long-term commitment, multi-sectoral coordination and collaboration and the uses of combination approaches in HIV prevention. The epidemiologic and public health approaches are important keys to the success. The greater the number of effective strategies employed, the greater the potential for achieving maximum overall impact. Because HIV/AIDS is a long-term problem, operational obstacles relating to budgetary and personnel limitations need to be resolved for the sustainability of the RTA's programs. The RTA HIV/AIDS prevention and impact-alleviation programs have met the criteria of effectiveness, efficiency, relevance, sustainability and ethical soundness. They have played a significant role in reducing the HIV/AIDS epidemic and related problems in Thailand, especially among young men. Its approach is considered to have been successful at the national level. HIV/AIDS, however, still poses many problems for Thailand and the response must be sustained by all sectors of Thai society.
Reference
1. Limsuwan A, et al. Acquired immune deficiency syndrome in Thailand: a report of two cases. J Med Assoc Thai 1986; 69: 164-169. [ Links ]
2. Weniger BG, et al. The epidemiology of HIV infection and AIDS in Thailand. AIDS 1991; 5 (Suppl 2): S71-S85. [ Links ]
3. AIDS Division, Department of Communicable Disease Control, MOPH, Projections for HIV/AIDS in Thailand: 2000-2020. Bangkok: Karnsassana Printing, 2001. [ Links ]
4. Bureau of Epidemiology, Department of Disease Control, MOPH. The Situation of AIDS in Thailand. Bureau of epidemiology, Department of Disease Control, MOPH, 2010.(in Thai) [ Links ]
5. Nelson KE, Celentano DD, Eiumtrakul S, et al. Changes in sexual behavior and a decline in HIV infection among young men in Thailand. N Engl J Med 1996; 35 (5): 297-303. [ Links ]
6. Park LS, Siraprapasiri T, Peerapatanapokin W, et al. HIV transmission rates in Thailand: evidence of HIV prevention and transmission decline. JAIDS 2010; 54: 430-436. [ Links ]
7. Sangkharomya S, Nitayaphan S, Eimtrakul S, Saengdidtha B, Sirisopana N, Kana K. HIV/AIDS prevention and control: an experience of the Royal Thai Army in Thailand. Copenhagen: UNAIDS Office on AIDS, Security and Humanitarian Response, 2004. (in Thai and English) [ Links ]
8. Saengdidtha B, Rangsin R. Roles of the Royal Thai Army Medical Department in supporting the country to fight against HIV/AIDS: 18 years of experience and success. J Med Assoc Thai 2005; 88 (Suppl 3): S378-87. [ Links ]
9. Celentano DD, et al. Epidemiological risk factors for incidence of sexually transmitted diseases in young thai men. Sex Trans Dis 1996;23(3):198-205. [ Links ]
10. Nopkesorn T et. al. Risk factors for HIV-1 infection in young Thai men in Northern Thailand, Meeting abstract Int. Conf. AIDS, Amsterdam, The Netherlands, 19-24 July 1992. [ Links ]
11. Saengdidtha B, Rangsin R, Wakai S, Sathityudhakarn O, Kaoaiem H. Development of risk assessment scale for HIVAIDS prevention among Thai army conscripts. 14th International AIDS Conference, July 7-12, 2002, Barcelona, Spain. [ Links ]
12. Saengdidtha B et al. Roles of Preventive Medicine Division of the Royal Thai Army Medical Department in the prevention and alleviation of HIV/AIDS between 1987 and 2001. RTA Med J 2001; 54: 179-89 (in Thai). [ Links ]
13. Rochananonda C, Supavit S, Srichaikul T, Showanasai A, Saengdidtha B, et al. Guidelines for prevention of AIDS in the Royal Thai Army military units. RTA Med J 1991; 44 (2): 69-74 (in Thai). [ Links ]
14. The Order issued by Ministry of Defense No. 81/43 on 29 May 2000 on Formation of Committee of Prevention and Alleviation of AIDS, Ministry of Defense, Thailand. (in Thai) [ Links ]
15. The Order issued by Ministry of Defense No. 227/40 on 7 October 1997 on Policy of Prevention and Alleviation of AIDS, Ministry of Defense, Thailand. (in Thai) [ Links ]
16. The Order issued by Ministry of Defense No. 125/38 on 14 August 1995 on Duties of administrative officers at every level in the Ministry of Defense and the Armed Forces in AIDS prevention and control measures, Ministry of Defense, Thailand. (in Thai) [ Links ]
17. The Order issued by the Royal Thai Army No. 917/42 on 20 August 1999 on Formation of a Committee of Prevention and Alleviation of AIDS, the Royal Thai Army, Thailand. (in Thai) [ Links ]
18. Memorandum RTA No. KH 0403/5667, 20 July 1999, on Request for Additions to AIDS Studies in the RTA Curriculum. Royal Thai Army, Thailand. (in Thai) [ Links ]
19. Torugsa K et al. GIS Mapping of HIV epidemic among young Thai men: 1991-2000. J Emerging Infectious Diseases 2003. 9(7): 881-3. [ Links ]
20. Sununtarod E, Kana K, Tabprasit S, Winitnaiphak N, Thongsen N, Saipin K, Saengdidtha B, et al. HIV- 1 seroprevalence in Royal Thai Army military recruits from 2000-2010. 13rd National Seminar on AIDS of Thailand, 29-31 March, 2011, Nonthaburi, Thailand. [ Links ]
21. Saengdidtha B, Wongba N, Lapparat G (ed.) Essentials for the prevention and alleviation of HIV/AIDS in the Royal Thai Army. Bangkok: Krung Siam Printing, 2000 (in Thai). [ Links ]
22. Saengdidtha B et al. HIV/AIDS counseling service in the Royal Thai Army hospitals. RTA Med J 1999; 52;247-51 (in Thai). [ Links ]
23. Saengdidtha B, Duangsawang K. Sexual behaviors of Thai army conscripts in Bangkok in 1991. Preventive Medicine Division of the RTA Medical Department (Unpublished paper), 1992. [ Links ]
24. Saengdidtha B, Sathityudhakarn O. Sexual behaviors of Thai army conscripts in Bangkok in 2009. Army Institute of Pathology (Unpublished paper), 2010. [ Links ]
25. Nitayaphan S, Brown A. Preventive vaccine development in Thailand. AIDS 1998, 12 (suppl B):S155-S61. [ Links ]
26. Nitayaphan S et al. A phase I/II Trial of HIV SF2 gp120/MF59 vaccine in seronegative Thais. Vaccine 2000; 18:1448-55. [ Links ]
27. Pitisuttithum P et al. the Thai AIDS Vaccine Evaluation Group. Safety and immunogenicity of combinations of recombinant subtype E and B HIV-1 envelope gp120 vaccines in healthy Thai adults. JID 2003; 188:219-27. [ Links ]
28. Carr JK Et al. Incidence of HIV-1 infection among military conscripts in Thailand. J Acquired Immune Defic Syndr 1994;7:1270-5. [ Links ]
29. Saengdidtha B, et al. The evaluation of the effectiveness of health education for the prevention of HIV/AIDS in the Royal Thai Army. Preventive Medicine Division of the RTA Medical Department (Unpublished paper), 1995. [ Links ]
30. Leelapattana B, Saengdidtha B, et al. Knowledge, attitude and reproductive experience of RTA students. RTA Med J 1993; 46: 21-20 (in Thai). [ Links ]
31. Leelapattana B, Saengdidtha B, et al. Knowledge, attitude and HIV/AIDS prevention experience of RTA students. RTA Med J 1995; 48:33-40 (in Thai). [ Links ]
32. Nelson KE et al. Behavioral dynamics of declining HIV-1 infection in young men in northern Thailand. N Eng J Med 1996; 335: 297-303. [ Links ]
33. Nopkesorn T, Mastro TD, Sangkharomya S. HIV-1 infection in young Thai men in northern Thailand. AIDS 1993, pp.1233-1239. [ Links ]
34. Nopkesorn T, Mastro TD, Sangkharomya S. HIV-1 seroconversion in a group of young male conscript in Northern Thailand. Int. Conf. AIDS, 6-11 June 1993. [ Links ]
35. Nopkesorn T, Sangkharomya S, Mastro TD. HIV/AIDS peer education for Thai military conscripts. [ Links ]
36. Jenkins RA et al. HIV risk behavior patterns among young Thai men. AIDS and Behavior 1999; 3:335-46. [ Links ]
37. Bubphasuwan U. The effectiveness of peer education program and higher commander reinforcement on sexually transmitted diseases preventive behavior among Thai army conscripts in Aranyaprathet border. Thesis for Master of Science (Public Health), Mahidol University, 1993. [ Links ]
38. Mason CJ, Kitsiripornchai S, Markowitz LE, et al. Nationwide surveillance of HIV-1 prevalence and subtype in young Thai men. J Acquir Immune Defic Syndr Hum Retrovirol 1998; 19(2): 165-73. [ Links ]
39. Nopkesorn T, Mastro TD, Sangkharomya S, et al. HIV-1 infection in young men in northern Thailand. AIDS 1993; 7 (9):1233-9. [ Links ]
40. Saengdidtha B, Lapparat G, Torugsa K, et al. Sexual behaviors and Human Immunodeficiency Virus infection among Thai army conscripts between 1992 and 1998. Mil Med 2002; 167 (4): 272-6. [ Links ]
41. Wongwaipanich S. Trends of HIV infection in Thai conscripts: Impacts on the Royal Thai Armed Forces and Thailand. Thesis for the National Defense College of Thailand, 2011. [ Links ]
42. Celentano DD, et al. Decreasing incidence of HIV and sexually transmitted diseaes in young Thai men: evidence for success of the HIV/AIDS control and prevention program. AIDS 1998; 12 (5): F29-F36. [ Links ]
43. Kana K, et al. HIV-1 incidence estimates among young Thai men using IgG-Capture BED- Enzyme Immunoassay (BED-CEIA) during 2005-2006. J Med Assoc Thai 2009; 92 (Suppl 1): S112-6. [ Links ]
44. Rangsin R, et al. The natural history of HIV-1 infection in young Thai men after seroconversion. J Acquir Immune Defic Syndr 2004; 36(1): 622-9. [ Links ]
45. Rangsin R, et al. The natural history of HIV-1 subtype E infection in young men in Thailand with up to 14 years of follow-up. AIDS 2007; 21 Suppl 6: S39-46. [ Links ]
46. Bhusal, Krishna. Assessment of sexual risk behavior regarding HIV/AIDS infection among Thai army conscripts in Bangkok. Thesis for Master of Primary Health Care Management, Mahidol University, 2001. [ Links ]
47. Hla Tun Oo. Safe sex behavior among conscripts in Royal Thai Military, Southern Thailand. Thesis for Master of Primary Health Care Management, Mahidol University, 2000. [ Links ]
48. Paranun Y, et al. Psychosocial factors associated with preventive behavior for HIV infection among conscripts. Journal of Psycho-Behavioral science: Thai behavioral system 2005; 2(2): 6-32. [ Links ]
49. Beyrer C, Eiumtrakul S, Celentano DD, et al. Same-sex behavior, sexually transmitted diseases and HIV risks among northern Thai men. AIDS 1995; 9: 171-6. [ Links ]
50. Celentano DD, Nelson KE, Suprasert S, et al. Behavioral and sociodemographic risks for frequent visits to commercial sex workers among northern Thai men. AIDS 1993; 7 (2): 1647-52. [ Links ]
51. Celentano DD, Nelson KE, Suprasert S, et al. Dynamics of risk behavior for HIV infection among young Thai men. J Acquir Immune Defic Syndr Hum Retrovirol 1995; 10 (4): 477-83. [ Links ]
52. Celentano DD, Nelson KE, Suprasert S, et al. Risk factors for HIV-1 seroconversion among young men in northern Thailand. JAMA 1996; 275 (2): 122-7. [ Links ]
53. Kitsiripornchai S, Markowitz LE, Ungchusak K, et al. Sexual behavior of young men in Thailand: regional differences and evidence of behavior change. J Acquir Immune Defic Syndr Hum Retrovirol 1998; 18: 282-8. [ Links ]
54. MacQueen KM, Nopkesorn T, Sweat MD, et al. Alcohol consumption, brothel attendance, and condom use: normative expectations among Thai military conscripts. Med Anthropol Q 1996; 10 (3): 402-23. [ Links ]
55. Saengdidtha B, Ungchusak K. Sexual behavior and sexually transmitted diseases among young Thai men in 1999. Venereology 2001; 14: 157-9. [ Links ]
56. Saengdidtha B, Suppadit W. HIV Risk behavior among young men in the Royal Thai Army: the challenge for military preventive medicine. 11th Asia Pacific Military Medicine Conference, Auckland, New Zealand on 7-10 June, 2001. [ Links ]
57. Saengdidtha B, et al. Addictive behaviors and prevalence of HIV risk-related behaviors among conscripted young Thai men: implications for surveillance and intervention. 8th National Seminar on AIDS of Thailand, July 11-13, 2001, Bangkok, Thailand. [ Links ]
58. Saengdidtha B, Sathityudhakarn O, Duangsawang K. Trends of sexual behaviors of Thai army conscripts in Bangkok. 12th IUSTI Asia-Pacific Congress on STI, HIV/AIDS, Beijing, China on October 24-27, 2002. [ Links ]
59. Saengdidtha B, Rangsin R, Sathityudhskarn O, Kaoaiem H. Risk factors for HIV infection among young Thai men. 15th International AIDS Conference, July 11-16, 2004, Bangkok, Thailand. [ Links ]
60. Kaoaiem H. The effect of squad leader mentors through short message services on mobile phone in promoting safe sex among First Army conscripts of Thailand. PhD (Public Health) dissertation, Chulalongkorn University, Bangkok, Thailand, 2011. [ Links ]
61. Celentano DD, Bond KC, Lyles CM, et al. Preventive intervention to reduce sexually transmittedinfections: a field trial in the Royal Thai Army. Arch Intern Med 2000; 160: 535-40. [ Links ]
62. Nanna P. The application of protection motivation theory and social support on AIDS preventive behavior among Thai army conscripts in the 11th Infantry Division, Chachoengsao province. Thesis for Master of Science (Public Health), Mahidol University, 2003. [ Links ]
63. Singtokham D. Health education program for behavioral change of HIV/AIDS preventive behavior among conscripts of the Infantry Battalion of the First Army Circle, Bangkok. Thesis for Master of Science (Public Health), Mahidol University, 2003. [ Links ]
64. Dobbins JG, et al. Herpes in the time of AIDS: a cmparison of epidemiology of HIV-1 and HIV-2 in young men in northern Thailand. Sex Transm Dis 1999; 26(2): 67-74. [ Links ]
65. Jatapai A, Nelson KE, Chuenchitra T, Kana K, Eiumtrakul S, Sunantarod E, Rangsin R. Prevalence and risk factors for hepatitis C virus infection among young Thai men. Am J Trop Med Hyg. 2010; 83(2): 433-9. [ Links ]
66. Sweat MD, Nopkesorn T, Mastro TD, et al. AIDS awareness among a cohort of young Thai men: exposure to information, level of knowledge, and perception of risk. AIDS Care 1995; 7 (5): 573-91. [ Links ]
67. Saengdidtha B, et al. HIV/AIDS knowledge, attitude and behaviors of conscripts in Phayao. Preventive Medicine Division of RTA Medical Department (Unpublished paper), 1993. [ Links ]
68. Saengdidtha B. The usefulness of HIV testing. Journal of AIDS and Preventive Medicine 2002; 1: 125-6. [ Links ]
69. Cambiano V, et al. 'Test and treat': the end of the HIV epidemic? Curr Opin Infect Dis 2011; 24(1): 19-26. [ Links ]
![]() Correspondence:
Correspondence:
Colonel Boonterm Saengdidtha.
Army Institute of Pathology.
Phramongkutklao Medical Center.
315 Ratchawithi Road, Ratchathewi.
Bangkok 10400, Thailand.
E-mail: boonterms@yahoo.com
Recibido: 28 de junio de 2011
Aceptado: 18 de noviembre de 2011