Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Osteoporosis y Metabolismo Mineral
versión On-line ISSN 2173-2345versión impresa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.12 no.3 Madrid jul./sep. 2020 Epub 25-Ene-2021
https://dx.doi.org/10.4321/s1889-836x2020000300002
ORIGINALS
Effect of frailty and sarcopenia on the risk of falls and osteoporotic fractures in an unselected population
2Central University Hospital of Asturias. University of Oviedo, Institute of Health Research of the Principality of Asturias (ISPA). Renal Research Network of the Carlos III Health Institute (ISCIII). Oviedo (Spain)
Objetive
Assess whether grip strength and difficulty in carrying out daily activities could be predictors of falls and osteoporotic fractures.
Material and methods
624 men and women over 50 years of age were randomly selected and followed for 8 years to determine the incidence of falls and non-vertebral osteoporotic fractures. At the beginning, the grip strength in the hands was measured and a questionnaire was filled out with clinical variables, risk factors related to osteoporosis, and questions related to difficulty or inability to perform daily activities.
Results
Grip strength in the hands was not associated with the incidence of falls and fractures. However, the impossibility or difficulty of “sitting for more than 1 hour in a hard chair”, “taking off socks or stockings” and “leaning from a chair to pick up an object from the floor” were associated with falls: 1.83 (1.16-2.89); 1.85 (1.14-3.00) and 1.68 (1.04-2.70), respectively. Similarly, the impossibility or difficulty of “carrying a 10-kilogram object for 10 meters” and “lifting a box with 6 bottles and putting them on a table” was associated with fracture: 2.82 (1.21-6.59) and 2.54 (1.12-5.81) respectively.
Conclusions
No association was found between grip strength and incidence of falls and osteoporotic fractures, but it was found with difficulty or inability to perform daily activities. Those related to greater strength were associated with fracture, while those related to functional capacity were associated with falls. Taking simple questionnaires could help predict events before they happen.
Key words osteoporotic fracture; sarcopenia; frailty; falls; daily activities
INTRODUCTION
Life expectancy has increased rapidly in the last century due to economic growth. This has led to reduced mortality, improved quality of life, as well as greater availability of health care. In fact, there are more elderly people than at any other time in our history, and it is anticipated that within the next few years there will be more older adults than children. This forecast makes it essential for people to reach this age in good health, to avoid increased healthcare costs due to longer hospital stays, readmissions and demand for healthcare resources. One of the most common disorders associated with aging is osteoporosis, the most fatal consequence of which is fracture. Approximately half of the clinical fractures that occur in postmenopausal women do not present criteria for osteoporosis according to their bone mineral density1. In fact, the highest percentage of fractures occur in osteopenic women. Thus, other variables or tools are needed that allow the identification of people at high risk of fractures, a determining factor of morbidity and mortality in the elderly population.
Frailty is a geriatric syndrome characterized by weight loss, tiredness, weakness, slow gait and decreased physical activity. It is secondary to endocrine dysregulation and a proinflammatory and prothrombotic state. Sarcopenia, characteristic of frailty, is a disorder associated with aging that involves a loss of muscle mass and muscle weakness, limiting the mobility of the person and increasing the risk of falls, fragility and fractures2.
In addition to the natural aging process, other factors, such as genetic factors, inadequate diet, physical inactivity, sedentary lifestyle, excessive bed rest, chronic diseases and/or certain pharmacological treatments, can favor the development of sarcopenia, contributing to the fragility and fractures, which has led to the term osteosarcopenia3.
A quick way to identify subjects at risk of sarcopenia is by using tools that allow us to assess muscle strength through an evaluation and scoring system in which records strength, ability to walk, get up from a chair, climb stairs and frequency of falls4.
Our study aims to assess the role that the muscle strength of "grip in the hands" and certain activities of daily life could have as instruments to predict the incidence of falls and osteoporotic fractures. In clinical practice, having simple tools that reveal the degree of sarcopenia and frailty could help to establish preventive measures before falls and fractures occur.
MATERIAL AND METHODS
The initial protocol of the study was designed to determine the prevalence of vertebral fracture at the European level (EVOS study), in which 4 centers initially participated from Spain, including our own. To do this, 624 men and women over 50 years of age were randomly selected from the Oviedo city registry. This same cohort was included in a prospective study that involved measurements of muscle grip strength in both hands with a dynamometer, on a scale ranging from 0 to 300 mmHg. They were also asked to fill in a questionnaire, specifically designed for the EVOS study, which had a good reproducibility index5,6. This survey contained questions on clinical variables (weight and height, among others, to calculate BMI), risk factors related to osteoporosis and a series of questions related to the difficulty or not to carry out certain daily life activities.
These activities were based on a questionnaire that measures functional disability ("Funktionsfragebogen Hannover, FFbHR")7 and that has several items with three possible answers: you can do it without difficulty, you can do it with some difficulty and you are unable to do it or can only do it with assistance. Likewise, the entire cohort underwent two lateral radiographs (the radiographic study was not completed in only 2 cases) and the collection of anthropometric measurements, such as height and weight to determine BMI. All subjects had sufficient ambulatory capacity to go up two floors without an elevator and 99% lived in their own home.
After measuring muscle strength and administering the questionnaire, this cohort was followed up prospectively for 8 years using 4 postal questionnaires in order to investigate the frequency of falls and the incidence of non-vertebral osteoporotic fracture during that period. All osteoporotic fractures, excluding skull and limb fractures, were confirmed by radiography or medical report. The total number of people who participated in the last follow-up was 427, with a participation percentage in the eighth year of 81.3% (excluding deaths), the percentages of the 3 previous postal follow-ups being 87.1, 87.5 and 82.4%, respectively.
All the studies carried out followed the principles set forth in the Declaration of Helsinki and were formally approved by the Committee for Clinical Trials of the Principality of Asturias.
Statistic analysis
Data analysis was carried out using SPSS version 17.0 for Windows. Quantitative variables were analyzed using Student's t test. The qualitative variables were analyzed using the chi square.
To analyze, at a multivariate level, the effect of the difficulty or inability to carry out certain activities of daily life without help on the incidence of falls and non-vertebral osteoporotic fracture, a logistic regression adjusted for age, sex, BMI, active smoker, previous fracture and family history of hip fracture. As a reference or comparison value, not having difficulty to carry out these activities was used.
RESULTS
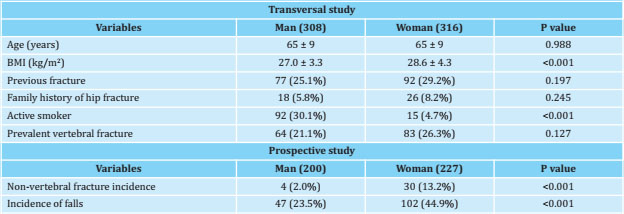
Table 1 shows the baseline characteristics of the study population. The age in both sexes was similar, with a statistically higher BMI in women. The history of previous fractures, the family history of hip fracture in parents or siblings, as well as the prevalence of vertebral fracture, were slightly higher in women than in men, but without statistically significant differences. Smoking habit was significantly higher in men. The incidence of non-vertebral osteoporotic fractures and the incidence of falls was markedly higher in women than in men.
Table 2 shows the muscle strength values in both hands as a function of the presence of falls during the follow-up period. The strength of the hands was lower in those who suffered falls, this effect being similar in both hands. The logistic regression analysis adjusted for age, sex, BMI, active smoker, previous fractures and family history of hip fracture, did not show a protective effect of muscle strength (every 10 mmHg increase), neither in the right hand: 0, 97 (0.90-1.03), nor on the left: 0.99 (0.92-1.05), on the incidence of falls.
Table 2. Effect of muscle strength and difficulty or inability to perform daily activities on the incidence of falls
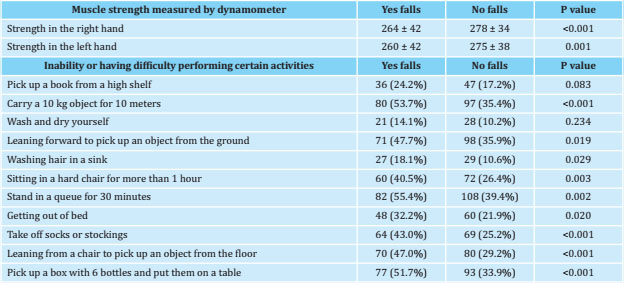
Table 2 shows the percentages of people who present inability or difficulty to carry out daily activities according to the incidence of falls. Regarding the subjects who did not have any difficulty, those who had falls presented an impossibility or difficulty in carrying out the following activities: "carrying a 10-kilo object for 10 meters (p<0.001)"; "lean forward to pick up an object from the ground (p=0.019)"; "wash hair in a sink (p=0.029)"; “sitting for more than 1 hour on a hard chair (p=0.003)”; "stand in a queue for 30 minutes (p=0.002)"; "get up from bed (p=0.020)"; “take off socks or stockings (p<0.001)”; "leaning from a chair to pick up an object from the floor (p<0.001)"; and “lift a box with 6 bottles and put them on a table (p<0.001)”.
The logistic regression analysis adjusted for age, sex, BMI, smoking, previous fractures and family history of hip fracture showed that the impossibility or difficulty of “sitting more than 1 hour on a hard chair” was significantly associated with an increase in the presence of falls: 1.83 (1.16-2.89). Difficulty or inability to “remove socks or stockings”, as well as “leaning from a chair to pick up an object from the floor” was significantly associated with an increase in the presence of falls: 1.85 (1.14-3, 00) and 1.68 (1.04-2.70), respectively. The multivariate analysis by sex showed associations in both sexes between the difficulty or inability to carry out certain daily activities with the incidence of falls. Specifically, in women, “sitting for more than 1 hour on a hard chair: 1.74 (1.01-3.02)” was associated with the incidence of falls; "stand in a queue for 30 minutes: 2.45 (1.41-4.25)"; and "take off the stockings”: 2.04 (1.183.55). On the contrary, in men, an association was only found with “leaning from the chair to pick up something from the ground: 2.57 (1.27-5.21)”.
Table 3 shows the muscle strength values in both hands as a function of the presence of incident non-vertebral osteoporotic fractures. The strength of the hands was lower in those who subsequently fractured, this effect being more pronounced in the strength of the right hand. The logistic regression analysis adjusted for age, sex, BMI, active smoker, previous fractures, and family history of hip fracture showed a slight tendency to a protective effect of muscle strength (every 10 mmHg increase) on the incidence of osteoporotic fracture. non-vertebral, although the differences were not statistically significant neither in the right hand: 0.95 (0.86-1.03) nor in the left: 0.97 (0.88-1.06).
Table 3. Effect of muscle strength and difficulty or inability to carry out daily activities on the incidence of non-vertebral osteoporotic fractures
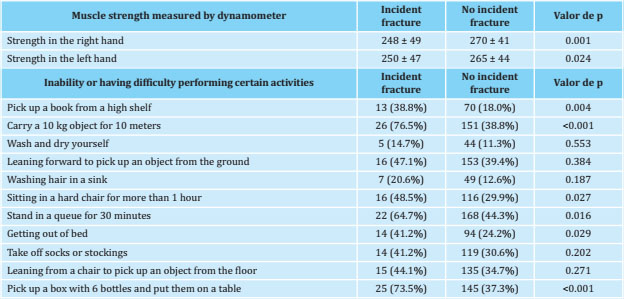
Table 3 also shows the percentages of people who were unable or difficult to perform daily activities based on the presence of incident non-vertebral osteoporotic fractures. In relation to the subjects who did not have any difficulty, those individuals with incident fracture presented an impossibility or difficulty in carrying out the following activities: “picking up an object from a high shelf (p=0.004)”; "carry a 10-kilo object for 10 meters (p<0.001)"; “sitting for more than 1 hour in a hard chair (p=0.027)”; "stand in a queue for 30 minutes (p=0.016)"; "getting up from bed (p=0.029)"; and “lift a box with 6 bottles and put them on a table (p<0.001)”.
All these univariate associations were analyzed by multivariate analysis. The logistic regression analysis adjusted for age, sex, BMI, active smoker, previous fractures, and family history of hip fracture showed that the impossibility or difficulty of “carrying a 10-kilogram object for 10 meters” was significantly associated with an increase in the presence of incident non-vertebral osteoporotic fracture: 2.82 (1.21-6.59). Similarly, the inability or difficulty to “lift a box with 6 bottles and put them on a table” was significantly associated with an increase in the presence of incident non-vertebral osteoporotic fracture: 2.54 (1.12-5.81). The multivariate analysis separately by sex only showed associations between the difficulty or inability to carry out daily activities with the incidence of non-vertebral osteoporotic fractures in women. Specifically, "take an object from a high shelf: 2.25 (1.00-5.05)"; "carry an object weighing 10 kilos for 10 meters: 3.47 (1.34-9.00)"; “sitting for more than 1 hour in a hard chair: 2.58 (1.11-6.00)”; and “lift a box with 6 bottles and put them on a table: 3.03 (1.237.49)”.
DISCUSSION
The concept of frailty in relation to osteoporosis is an increasingly accepted concept in the elderly as a predictor of osteoporotic fractures. It is estimated that between 25 and 50% of those over 85 years of age present frailty8, determined by genetic, epigenetic and environmental factors. Sarcopenia involves the loss of muscle mass and strength related to aging, which is a key component of frailty. Strategies aimed at improving muscle strength and mass, such as increased protein intake and resistance and muscle strength training, have reportedly decreased the prevalence of sarcopenia and frailty, as well as improve strength and physical performance9-11.
Several plausible mechanisms have been proposed between sarcopenia and the risk of fractures. On the one hand, small changes in muscle mass in muscle proteins such as myokines associated with abnormal glucose metabolism have a great impact on bone metabolism12. On the other hand, sarcopenic individuals have a high risk of falls, which leads to a higher incidence of fractures13. Therefore, sarcopenia is considered an effective predictor of fracture risk in the elderly14. However, the prevalence of sarcopenia is difficult to establish.
A meta-analysis found a great variability in the prevalence in elderly patients admitted to nursing homes from 1% to 29%15. In our study, although lower muscle strength was associated with the risk of falls and fractures at the univariate level, the multivariate analysis did not show significant differences. However, there was a modest trend that a 10 mmHg increase in muscle strength in the hands was capable of reducing the incidence of non-vertebral osteoporotic fracture by up to 5%. In reality, the study only collected the grip strength in the hands without any other measurable parameter of strength or muscle mass, so we believe that this instrument alone is not useful to assess the degree of sarcopenia if it is not accompanied by other complementary tests.
There is evidence that the frailty index is predictive of osteoporotic fractures independent of chronological age in patients16-19. In fact, a study with data from the Canadian Multicenter Osteoporosis Study (CaMos) conducted in 9,423 adults with a mean age of 62 years and a follow-up of 10 years showed a hazard ratio of 1.18 and 1.30 for hip fractures and clinical vertebral fractures for each 0.10 increase in the frailty index19. There are authors who indicate the need to validate fragility instruments before they can serve as a guide when making clinical decisions20.
In our study, the incidence of falls was not associated with a decrease in muscle strength, but it was associated with daily activities that reflect stability and adequate physical condition, such as being able to remain “sitting for more than 1 hour in a hard chair”, “taking an object on the floor from a chair and “being able to remove stockings or socks ”. Other authors have also observed that frailty affects the incidence of falls21.
In this study, frailty was evaluated based on a validated questionnaire that measures functional grade in people with back pain7. This questionnaire contains questions that relate to the activities of daily life that are part of many of the instruments for measuring frailty. It is interesting to note that the loss of strength (lifting objects and carrying them a few meters) were the factors that were best associated with increases in the incidence of fracture (up to 2.5 times). The analysis separated by sex showed only positive associations in women, with these activities, as well as others (stretching to pick up an object or sitting in a hard chair for 1 hour), predictive of the incidence of fractures. In men, no effect was observed, contrary to what other authors refer to22. This discrepancy could be related to the low number of incident fractures in males (n=4) found in our study. It is worth mentioning that during the 8-year follow-up there were 6 other incident osteoporotic fractures in men, but these subjects were excluded from the analysis as they did not reach the end of the indicated follow-up period.
A subsequent analysis was carried out (data not shown in the results), using a score to grade the difficulties in carrying out the 11 activities of daily life included in the functional disability questionnaire, with a minimum of 0 (those who had no difficulty in carry out them) up to a maximum of 22 (those unable to do these activities by themselves). It was observed that, when categorizing the score into quartiles, those with the worst condition (quartile 4) had an increase in the incidence of falls in the multivariate analysis of 2.37 (1.25-4.52) compared to those who were in better condition (quartile 1). This effect could not be observed for the incidence of fracture, which may indicate that worse physical condition would be a predictor of the appearance of falls, but not of fractures, although falls are a risk factor for the appearance of fracture. On the contrary, those activities most related to loss of strength, such as lifting objects and carrying them a few meters, were those that were best associated with the incidence of fracture, up to more than 3 times in the case of women.
Based on these results, the information on the evaluation of frailty and sarcopenia can, together or in parallel, be another tool for osteoporosis assessment, providing a more comprehensive view of the risks that these patients may present23.
This study has limitations in that the muscle fragility or strength was measured at the beginning of the followup, so we cannot rule out that the result obtained during a prolonged follow-up period of 8 years has been underestimated. The questions that contained questions related to difficulties in carrying out daily living activities were not self-administered, but administered by an interviewer, which could have biased the participants’ responses, especially in those questions related to difficulties for the self. personal cleanliness. The questionnaire used to measure difficulties in carrying out daily activities was focused on evaluating functional disability in people with back pain. However, despite this, we believe its questions give an idea of the degree of the individual’s physical and functional deterioration. Information on how the falls were to related to the fracture that occurred would have been very valuable. Unfortunately, this possibility was not included in the EVOS-EPOS study guidelines.
Despite these limitations, we believe our study has important strengths. On the one hand, the analyzed cohort participated in the EVOS-EPOS study, ours being one of the 5 centers that completed all the study guidelines. Furthermore, the response in the four postal follow-ups carried out during the 8 year period showed a greater than 80% response, which broadly supports the representativeness of the analyzed sample.
In summary, we have been able to verify that difficulties in carrying out certain activities of daily or daily life can presage a deterioration in physical capacity and functional status, being able to constitute another tool in the patient's anamnesis that helps to predict and probably avoid falls and osteoporotic fractures.
As conclusions of this work, we can affirm that no associations were found between grip strength and incidence of falls and osteoporotic fractures. Those activities more related to greater strength were associated with fracture, while those related to greater functional capacity were associated with falls.
Funding: This work has been partially funded by the European Study on Vertebral Osteoporosis (EVOS), European Union (1991–1993); European Prospective Osteoporosis Study (EPOS), European Union (BIOMED 93–95), BMHI-CT 092-0182 (1993–1997); Health Research Fund (FIS 94/1901-E); Retic REDin-REN of ISCIII (RD06/0016/1013, RD12/0021/0023 and RD16/0009/0017); National R + D + I Plan 2008-2011, State R + D + I Plan 2013-2016, European Regional Development Fund (ERDF), Science, Technology and Innovation Plan 2013-2017 and 2018 -2022 of the Principality of Asturias (GRUPIN14-028, IDI-2018-000152), Fundación RenalÍñigo Álvarez de Toledo (FRIAT). Sara Fernández-Villabrille has been funded by IDI-2018-000152; Julia Martín-Vírgala for a scholarship from the University of Oviedo, Beatriz Martín Carro for ISCIII-FINBA (PI17/00384) and Javier Rodriguez-Carrio for a Juan de la Cierva and Sara Borrell contract.
REFERENCES
1 Siris ES, Brenneman SK, Barrett-Connor E, Miller PD, Sajjan S, Berger ML, et al. The effect of age and bone mineral density on the absolute, excess, and relative risk of fracture in postmenopausal women aged 50-99: results from the National Osteoporosis Risk Assessment (NORA). Osteoporos Int. 2006;17:565-74. [ Links ]
2 Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. European Working Group on Sarcopenia in Older People. European working group on sarcopenia in older people. Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing. 2010;39:412-23. [ Links ]
3 Paintin J, Cooper C, Dennison E. Osteosarcopenia. Br J Hosp Med (Lond). 2018;79(5): 253-8. [ Links ]
4 Parra-Rodríguez L, Szlejf C, García-González AI, Malmstrom TK, Cruz-Arenas E, Rosas-Carrasco O. Cross-cultural adaptation and validation of the Spanish-language version of the SARC-F to assess sarcopenia in Mexican community-dwelling older adults. J Am Med Dir Assoc. 2016;17:1142-6. [ Links ]
5 O'Neill TW, Cooper C, Algra D, Pols HAP, Agnusdei D, Dequeker J, et al, on behalf of the European Vertebral Osteoporosis Study Group. Design and development of a questionnaire for use in a multicentre study of vertebral osteoporosis in Europe: The European vertebral osteoporosis study (EVOS). Rheumatology in Europe. 1995;24:75-81. [ Links ]
6 O'Neill TW, Cooper C, Cannata JB, Diaz Lopez JB, Hoszowski K, Johnell O, et al, on behalf of the European Vertebral Osteoporosis Study (EVOS) Group. Reproducibility of a questionnaire on risk factors for osteoporosis in a multicentre prevalence survey: the European Vertebral Osteoporosis Study. Int J Epidemiol. 1994;23: 559-65. [ Links ]
7 Kohlmann T, Raspe H. Der Funktionsfragebogen Hannover zur alltagsnahen Diagnostik der Funktionsbeeinträchigung durch Rückenschmerzen (FFbHR). Rehabilitation. 1996;35:I-VIII. [ Links ]
8 Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752-62. [ Links ]
9 Robinson SM, Reginster JY, Rizzoli R, Shaw SC, Kanis JA, Bautmans I, et al. ESCEO working group. Does nutrition play a role in the prevention and management of sarcopenia? Clin Nutr. 2018;37:1121-32. [ Links ]
10 Nascimento CM, Ingles M, Salvador-Pascual A, Cominetti MR, Gomez-Cabrera MC, Viña J. Sarcopenia, frailty and their prevention by exercise. Free Radic Biol Med. 2019;132:42-9. [ Links ]
11 Naseeb MA, Volpe SL. Protein and exercise in the prevention of sarcopenia and aging. Nutr Res. 2017;40:1-20. [ Links ]
12 Kawao N, Kaji H. Interactions between muscle tissues and bone metabolism. J Cell Biochem. 2015;116: 687-95. [ Links ]
13 Ormsbee MJ, Prado CM, Ilich JZ, Purcell S, Siervo M, Folsom A, et al. Osteosarcopenic obesity: the role of bone, muscle, and fat on health. J Cachexia Sarcopenia Muscle. 2014;5:183-92. [ Links ]
14 Zhang Y, Hao Q, Ge M, Dong B. Association of sarcopenia and fractures in community-dwelling older adults: a systematic review and meta-analysis of cohort studies. Osteoporos Int. 2018;29:1253-62. [ Links ]
15 Cruz-Jentoft AJ, Landi F, Schneider SM, Zuniga C, Arai H, Boirie Y, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the international sarcopenia initiative (EWGSOP and IWGS). Age Ageing. 2014;43:748-59. [ Links ]
16 Ensrud KE, Ewing SK, Taylor BC, Fink HA, Stone KL, Cauley JA, et al. Frailty and risk of falls, fracture, and mortality in older women: the study of osteoporotic fractures. J Gerontol A Biol Sci Med Sci. 2007;62:744-51. [ Links ]
17 Tom SE, Adachi JD, Anderson Jr FA, Boonen S, Chapurlat RD, Compston JE, et al. Frailty and fracture, disability, and falls: a multiple country study from the global longitudinal study of osteoporosis in women. J Am Geriatr Soc. 2013;61:327-34. [ Links ]
18 Fang X, Shi J, Song X, Mitnitski A, Tang Z, Wang C, et al. Frailty in relation to the risk of falls, fractures, and mortality in older Chinese adults: results from the Beijing Longitudinal Study of Aging. J Nutr Health Aging. 2012;16 (10):903-7. [ Links ]
19 Kennedy C, Ioannidis G, Rockwood K, Thabane L, Adachi J, Kirkland S, et al. A frailty index predicts 10-year fracture risk in adults age 25 years and older: results from the Canadian multicentre osteoporosis study (CaMos). Osteoporos Int. 2014.;25:2825-32. [ Links ]
20 Rockwood K, Theou O, Mitnitski A. What are frailty instruments for? An overview of osteoporosis and frailty in the elderly. Age Ageing. 2015;44(4): 545-7. [ Links ]
21 de Vries OJ, Peeters GMEE, Lips P, Deeg JH. Does frailty predict increased risk of falls and fractures? A prospective population-based study. Osteoporos Int. 2013;24:2397-403. [ Links ]
22 Yu R, Leung J, Woo J. Incremental predictive value of sarcopenia for incident fracture in an elderly Chinese cohort: Results from the osteoporotic fractures in men (MrOs) Study. J Am Med Dir Assoc. 2014;15:551-8. [ Links ]
23 Li G, Thabane L, Papaioannou A, Ioannidis G, Levine MAH, Adachi JD. An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet Disord. 2017;18:46. [ Links ]
Received: August 05, 2020; Accepted: October 27, 2020











 texto en
texto en