Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Osteoporosis y Metabolismo Mineral
versión On-line ISSN 2173-2345versión impresa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.13 no.2 Madrid jun. 2021 Epub 16-Ago-2021
https://dx.doi.org/10.4321/s1889-836x2021000200005
BRIEF ORIGINAL
Humeral fragility fractures in a tertiary referral hospital. Clinical and epidemiological characteristics
1Bone Metabolism Unit. Internal Medicine Service. Marqués de Valdecilla University Hospital - Medical Research Institute Valdecilla (IDIVAL). Santander (Spain)
2Department of Medicine and Psychiatry. University of Cantabria. Santander (Spain)
Objetive
Humeral fragility fractures represent an important complication of osteoporosis as they rank the third most prevalent in individuals over sixty years old. Our study aims to analyze the prevalence and treatment of the humeral fragility fractures in a tertiary referral hospital.
Material and methods
Retrospective study of those patients presenting humeral fragility fractures who attended a tertiary referral hospital during 2013. Clinical and epidemiological variables were collected, and the incidence of new fractures and that of mortality was analyzed over a three-year period.
Results
248 humeral fragility fractures were analyzed. 81% of the patients were women whose average age was 71 years. 28.2% of the patients have suffered a previous fracture and 20.2% of them suffered one at a later time. 12.5% had been previously diagnosed with osteoporosis and only 9.2% got this bone metabolic condition diagnosed after fracturing the humerus. 18% of patients passed away during the follow-up period.
Conclusions
In our area of expertise, humeral fragility fractures are followed by a low percentage of underlying osteoporosis cases being diagnosed and treated, what may be the trigger to a rise in the risk of new fractures.
Key words fractura humeral; osteoporosis; mortalidad
INTRODUCTION
The humeral fragility fracture is an important consequence of osteoporosis. It constitutes 5% of all osteoporotic fractures and is the third most frequent non-vertebral fracture in individuals over 60 years of age after hip fractures and those of the distal radius1. Compared with the general population, patients with a proximal humeral fracture present a higher mortality rate in the first year, the risk being five times higher during the first month after the fracture2.
Several studies have been published into the risk factors linked to vertebral or hip fractures while the lack of studies about humeral fractures as indicators of osteoporosis stands out. Thus, in the Reykjavik Study Fracture Register, 9,504 osteoporotic fractures were analyzed and 3,616 patients who showed new major fragility fractures were screened. This led the researchers to propose that the risk of suffering a recurring fracture changed according to age, gender and the place where the previous fracture was located, therefore posing a higher risk of suffering vertebral and hip fractures than that of humeral or wrist fracture3. Humeral fracture is not usually related to osteoporosis in standard clinical practice. So a limited of antiosteoporotic drugs are prescribed post fracture, as some retrospective studies report4,5.
The aim of the present study was to analyze the clinical and epidemiological characteristics, and management, of the patients presenting humeral fragility fractures and the incidence of new clinical fractures. We also report their mortality rate over the three-year follow-up period.
PATIENTS AND METHODS
A retrospective and descriptive cohort study was carried out of all patients aged 45 or over, diagnosed with humeral fragility fractures at the Marqués de Valdecilla University Hospital (HUMV) during 2013. It is a tertiary referral university hospital assisting a population of 350,000 inhabitants in Cantabria. Humeral fractures were identified through the center's Clinical Documentation and Admission Service database, using the code CIE9-MC 812 (812.0; 812.1; 812.2; 812.3). In addition, a follow-up of the cases was carried out, through medical records, from the moment of the humeral fracture until December 31, 2016, to analyze the development of new fractures and all-cause mortality.
Initially 337 patients with humeral fractures were identified. Of this group, 89 were excluded from the analysis because they presented high-energy traumatic fractures (n=79) or because of the absence or loss of clinical data in the first episode or during follow-up (n=10).
The following variables were analyzed: age, gender, age at menopause, body mass index (BMI) (kg/m2), smoking habit (smoker, non-smoker or ex-smoker), alcohol habit (consumption of more than 30 g of ethanol per day, less than 30 g or ex-drinker), diseases with influence over or related to bone metabolism (hyperthyroidism, hyperparathyroidism, malabsorptive syndromes such as celiac disease or inflammatory bowel diseases, rheumatoid arthritis, metastatic neoplastic disease or hematological neoplasms), chronic treatment with corticosteroids (≥7.5 mg per day for more than 3 months), risk factors associated with falls, both intrinsic (visual, gait and balance disturbances) and extrinsic (use of benzodiazepines or hypotensive drugs), existence of previous fractures unrelated to the skull or face (vertebral fracture, in the hip, radius or other locations), existence of previous multiple fractures, history of hip fracture in a first-degree relative or, previous diagnosis of osteoporosis, previous treatment for osteoporosis (calcium and vitamin D supplements, bisphosphonates, selective estrogen receptor modulators -SERM-, teriparatide, denosumab, strontium ranelate), date of the humeral fracture, location of the humeral fracture (proximal or diaphyseal), treatment of the fracture (surgical or orthopedic), subsequent diagnosis of osteoporosis, performance of bone densitometry and result if affirmative (bone mineral density -BMD- in g/cm2 and T index), subsequent treatment for osteoporosis, new fractures after the humeral fracture (vertebral fracture, in the hip, radius or other locations), refracture of the same humerus, and finally, death within 3 years after the initial fracture and date of the same.
For the statistical data analysis, a descriptive study was carried out. Qualitative variables were expressed as frequencies, number and percentage, and quantitative variables as mean and standard deviation (SD). The data were collected anonymously through an individualized registration code. A level of p<0.05 was considered significant.
RESULTS
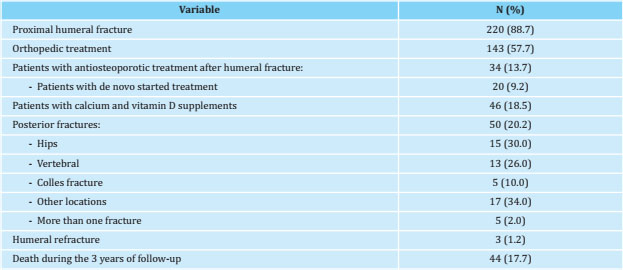
248 patients with humeral fragility fractures were included in the analysis. Table 1 summarizes the main clinical and epidemiological characteristics of the cases analyzed.
Table 1. Clinical and epidemiological characteristics of patients with humeral fragility fractures (n=248)
The mean age was about 71 years and 81% of the fractures occurred in women. The mean age at menopause was 49 years and the mean BMI was 28 kg/m2, indicator of overweight.
It should be noted that a high percentage of the patients took drugs associated with an increased risk of falls, benzodiazepines being the most common, followed by antihypertensive drugs. Diseases with an effect on bone metabolism were also evaluated, finding that 11% suffered from any of them.
Almost a third of the patients had suffered previous fractures (excluding skull, facial, or hand and foot fractures), the most frequent being those of the hip and the distal radius. In addition, about 14% had presented fractures in more than one location. It is noteworthy that in only 0.4% of the cases' medical history a hip fracture in a first-degree relative was registered.
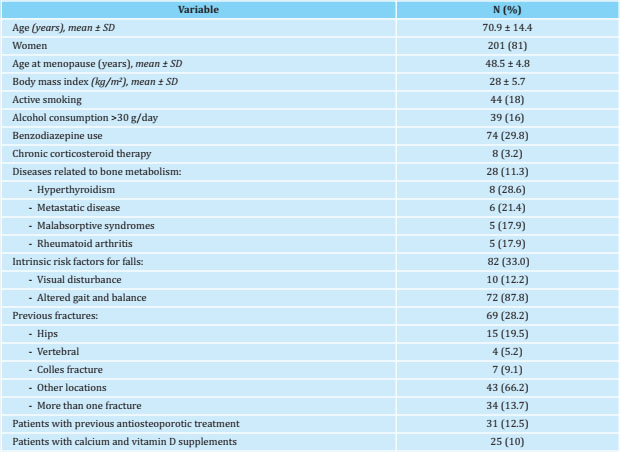
Table 2 shows the management of patients with humeral fracture and the follow-up variables analyzed. During this follow-up period, one fifth suffered a new fracture and about 18% died within 3 years after the initial humeral fracture.
The changes in antiosteoporotic treatments after humeral fracture are shown in table 3. 31 patients had a previous diagnosis of osteoporosis and had received treatment, 23 patients had been treated with bisphosphonates, 3 with denosumab, 2 with teriparatide, 2 with strontium ranelate and 1 with a SERM. It is worth noting that out of the 31 patients previously treated for osteoporosis, in 17 of them (more than half) it was interrupted or not restarted after the humeral fracture. It was observed that in 7 patients who had received a treatment with oral bisphosphonates for 10 years, it was suspended, without restarting, after suffering the humeral fracture. In addition, 2 patients under treatment with bisphosphonates died during follow-up, 1 patient had received full treatment with teriparatide for two years, and 1 patient had been treated for one year with denosumab without specifying the reason for its suspension. In 6 patients, the reason why the previous treatment had been suspended was not reflected. In none of these 17 patients was the need to initiate treatment for osteoporosis raised in their medical records at the time of the humeral fracture despite being all of them diagnosed with osteoporosis.
Table 3. Changes in antiosteoporotic treatment in patients previously diagnosed with osteoporosis and initial treatment in patients without a prior diagnosis
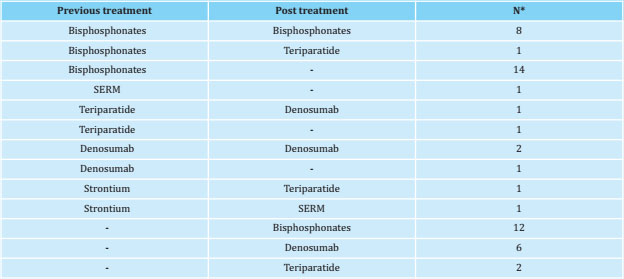
*: number of patients receiving treatment before and after the humeral fracture; SERM: selective estrogen receptor modulators.
Treatment was restarted after the humeral fracture in 20 patients (12 with bisphosphonates, 6 with denosumab and 2 with teriparatide). Besides, calcium in combination with vitamin D was prescribed to 46 patients.
DISCUSSION
We have analyzed a retrospective cohort of 248 patients with humeral fragility fracture, who had a 3-year followup. After the humeral fracture, a low percentage of them were diagnosed and treated for underlying osteoporosis.
More than 80% of all humeral fractures occurred in women. In this sense, Chu et al.6 observed that humerus fractures are 3 to 4 times more common in women, findings similar to those published by Clinton et al.7 The patients' mean age (71 years) is similar to that published in previous studies reporting age ranges between 64 and 79 years8-11.
Mean BMI of 28 kg/m2 describes an overweight population. This is an interesting fact, since overweight and obesity represent a risk factor for suffering a humeral fracture, but their relation with other osteoporotic fractures, such as that of the hip, is less clear as hip fractures are usually linked to low weight12. Regarding toxic habits, nearly 20% of the patients were active smokers and consumed more than 30 g of ethanol per day (maximum limit recommended by the World Health Organization in men, being 20 g that in women). These proportions were very similar to the 28% and 15%, respectively, reported by Roux et al.13, which highlights the need to spend time and resources on promoting health and healthy habits as a fundamental part of the treatment of osteoporosis.
Regarding the consumption of drugs at the time of the humeral fracture, the high percentage of people under treatment with benzodiazepines is surprising. This pharmacological group is widely prescribed in standard practice, and its use has been related to an increased risk of falls, and consequently, of fractures14.
A relevant percentage of patients with humeral fractures, nearly a third, had already presented a previous fracture and 20% suffered a subsequent fracture. In terms of distribution, 15 patients had already had a hip fracture, while another 15 had a hip fracture in the follow-up period. 47% of these occurred during the first year after the initial humeral fracture. About this, Clinton et al.7 have reported that a fracture of the proximal limb of the humerus increases the risk of hip fracture in more than 5 times during the first year, but it does not seem to be linked to a significant increase in subsequent years. These data are interesting since the humeral fracture is presented as an opportunity to optimize prevention of subsequent fractures in these patients.
Treatment and diagnosis of osteoporosis prior to the humeral fracture was limited (12.5%). This figure is consistent with the 19% published by Piple et al.4, who studied a retrospective cohort of 1,700 patients aged 50 or over with humeral fracture between 2008 and 2014. However, it should be emphasized that only 20 of the 217 of our patients who did not receive antiosteoporotic treatment, 9.2%, were diagnosed with osteoporosis and treated after the initial humeral fracture. This percentage is somewhat higher than the 5.5% reported in a retrospective national study in which 11,609 patients aged 50 or over with a humeral fracture were analyzed5. This reflects that, in standard clinical practice, this type of fracture continues to be a poorly considered entity when it comes to prescribing a treatment for osteoporosis. Furthermore, it is far behind other major fractures, such as vertebral or hip fractures, which are also often undertreated5,15.
Regarding mortality, in a study carried out in patients over 16 years of age presenting humeral fractures, an even greater risk of mortality in men was observed than that reported after a hip fracture16. We cannot compare these data with our study as the age group and the gender distribution were different. A study carried out in Korea in individuals over 50 years of age with a proximal humeral fracture during the period 2008-2012, showed an annual percentage of mortality in men of between 8.5% and 10.8%, and in women of between 6.4% and 7%17.
Limitations of the study are its retrospective design, the study scope restricted to a single center, the lack of data into the causes of mortality and the influence of comorbidities on it.
In conclusion, humeral fragility fractures are followed, in our field of expertise, by a low percentage of diagnosis and treatment for underlying osteoporosis, which may trigger an increased risk of new fractures. The humeral fragility fracture is a major osteoporotic fracture and specific antiosteoporotic treatment should be initiated to minimize it.
Bibliografía
1 Court-Brown CM, Garg A, McQueen MM. The epidemiology of proximal humeral fractures. Acta Orthop Scand. 2001;72(4):365-371. [ Links ]
2 Bergdahl C, Wennergren D, Ekelund J, Moller M. Mortality after a proximal humeral fracture. Bone Joint J. 2020; 102-B:1484-1490. [ Links ]
3 Kanis JA, Johansson H, Harvey NC, Gudnason V, Sirgurdsson G, Siggeirs-dottir K, et al. The effect on subsequent fracture risk of age, sex, and prior fracture site by recency of prior fracture. Osteoporos Int. 2021 Feb 4. Online ahead of print. [ Links ]
4 Piple A, Smith CT, Barton DW, Carmou-che JJ. Proximal humerus fractures in the geriatric population present an opportunity to improve recognition and treatment of osteoporosis. Geriatr Orthop Surg Rehabil. 2020;11:1-6. [ Links ]
5 Kim TI, Choi JH, Kim SH, Oh JH. The adequacy of diagnosis and treatment for osteoporosis in patients with proximal humeral fractures. Clin Orthop Surg. 2016;8(3):274-279. [ Links ]
6 Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP, et al. Risk factors for proximal humerus fracture. Am J Epidemiol. 2004;160[4):360-367. [ Links ]
7 Clinton J, Franta A, Polissar NL, Neradilek B, Mounce D, Fink HA, et al. Proximal humeral fracture as a risk factor for subsecuent hip fractures. J Bone Joint Surg Am. 2009;91:503-511. [ Links ]
8 Navarro J, López-Vázquez E, Juan A, Recalde E. Tratamiento de las fracturas de tercio proximal de húmero mediante osteosíntesis con placa. Rev Esp Cir Ortop Traumatol. 2010;54(6): 372-377. [ Links ]
9 Schousboe JT, Fink HA, Lui L, Taylor BC, Ensrud KE. Association between prior non-spine non-hip fractures or prevalent radiographic vertebral deformities known to be at least 10 years old and incident hip fracture. J Bone Miner Res. 2006;21:1557-1564. [ Links ]
10 Nguyen TV, Center JR, Sambrook PN, Eisman JA. Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women. Am J Epidemiol. 2001;153:587-595. [ Links ]
11 Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, et al. Fracture risk following an osteioporo-tic fracture. Osteoporos Int. 2004; 15:175-179. [ Links ]
12 Fassio A, Idolazzi L, Rossini M, Gatti D, Adami G, Giollo A, et al. The obesity paradox and osteoporosis. Eat Weight Disord. 2018;23(3):293-302. [ Links ]
13 Roux A, Decroocq L, El Batti S, Bonne-vialle F, Moineau G, Trojani C, et al. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012; 98:715-719. [ Links ]
14 San José A, Agustí A, Vidal X, Formiga F, Gómez-Hernández M, Barbé J. Inappropriate prescribing to the oldest old patients admitted to hospital: prevalence, most frequently used medicines, and associated factors. BMC Geriatr. 2015;15:42. [ Links ]
15 Chau YT, Nashi N, Law LS, Goh RKH, Choo SX, Seetharaman SK. Undertreatment of osteoporosis following hip fracture: a retrospective, observational study in Singapore. Arch Osteoporos. 2020;15(1):141. [ Links ]
16 Somersalo A, Paloneva J, Kautiainen H, Lonnroos E, Heinanen M, Kiviranta I. Increased mortality after upper extremity fracture requiring inpatient care. Acta Orthopaedica. 2015;86(5):533-557. [ Links ]
17 Park C, Jang S, Lee A, Kim HY, Lee BY, Kim TY, et al. Incidence and mortality after proximal humerus fractures over 50 years of age in South Korea: national claim data from 2008 to 2012. J Bone Metab. 2015;22:17-21. [ Links ]
Received: December 30, 2020; Accepted: April 11, 2021











 texto en
texto en