Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Osteoporosis y Metabolismo Mineral
versión On-line ISSN 2173-2345versión impresa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.13 no.2 Madrid jun. 2021 Epub 16-Ago-2021
https://dx.doi.org/10.4321/s1889-836x2021000200006
REVIEW
Calcium and vitamin D supplementation in the management of osteoporosis. What is the advisable dose of vitamin D?
1Research Group on Osteoporosis and Bone Mineral Metabolism. University of Las Palmas de Gran Canaria. Las Palmas de Gran Canaria (Spain)
2Bone Metabolic Unit. Insular University Hospital. Las Palmas de Gran Canaria (Spain)
3Department of Medicine. Seville University. Seville (Spain)
The pathophysiological foundations justifying calcium and vitamin D supplements in osteoporosis are supported by extensive scientific evidence that has been obtained through several randomized clinical trials and subsequent meta-analyzes that have shown a statistically significant and clinically relevant reduction in the risk of osteoporotic fractures. This evidence has led to its recommendation by several scientific societies interested in the management of osteoporosis.
In order to optimize the efficacy and the benefit/risk balance of these, calcium and vitamin D should be administered together with the drugs that are prescribed for the treatment of osteoporosis, since calcium and vitamin D have been used in all these reference studies, both in the arm that receives the drug and also in the placebo arm. The most commonly used calcium salt is carbonate and the metabolite of vitamin D, cholecalciferol or vitamin D3. There is no consensus or conclusive scientific evidence on the dose to be used in vitamin D deficiency associated with osteoporosis. However, the trend has always been to increase these amounts, from the 400 IU recommended 30 years ago to the 2,000 IU daily today. We will review in this article which recommendations are made by means of the clinical guidelines, as they collect the available scientific evidence.
Rationale for using calcium and vitamin D in osteoporosis
Osteoporosis is the most common bone metabolism disease1 and is characterized by a significant decrease in bone mineral density that is accompanied by alterations in the microarchitecture of the bone, which results in increased skeletal fragility and, consequently, an increase risk of fractures2. Clearly related to aging, its prevalence, which in women between 50 and 59 years of age has been estimated at 4%, increases to 52% in women older than 80 years2. Hip fracture in osteoporotic women produces an increase in mortality over the first two years post-fracture of between 12 and 20%, and more than 50% of survivors are not able to return to an independent life, many of them requiring long-term home help3.
Calcium is a mineral-type nutrient that plays key roles in human physiology. In relation to bone, it is a basic constituent of calcium hydroxyapatite crystals, a form that contains 99% of the body's calcium and a fundamental component of bones and teeth. Insufficient calcium accumulation leads to low bone mineralization and a decrease in peak bone mass, this being one of the key factors for the appearance of osteoporosis and associated osteoporotic fractures. In this sense, bone tissue acts as a calcium reservoir to guarantee the efficiency of all these physiological processes, regulating its exit from the bone through the bone remodeling process4.
Furthermore, vitamin D, hormone D, or 1,25 (OH)2 D (1,25 dihydroxycholecalciferol, or calcitriol) facilitates the intestinal absorption of calcium by regulating calcium transport proteins and the consequent promotion of transport of transcellular calcium at the level of the intestine5. The main function of the endocrine system of vitamin D at the bone level is to preserve serum calcium homeostasis. Therefore, vitamin D deficiency causes secondary hyperthyroidism that normalizes serum calcium through increased renal synthesis of hormone D from its immediate precursor, calcidiol or 25 (OH) D (25hydroxy cholecalciferol), increasing both the intestinal absorption of dietary calcium as compensatory bone resorption at the expense of increased bone turnover and consequent loss of bone mass5. Even moderate vitamin D deficiency can promote age-mediated physiological bone loss and thus accelerate the pathophysiological process of osteoporosis, significantly increasing the risk of osteoporotic fragility fractures6. Furthermore, the important impact of vitamin D on muscle biology cannot be ignored, since it has been observed that the increased risk of falls associated with hypovitaminosis D may lead to an increased risk of osteoporotic fractures5.
Calcium and vitamin D in randomized clinical trials and meta-analyzes
Meta-analysis with positive results
We have several meta-analyzes carried out with the many randomized, double-blind, placebo-controlled clinical trials (RCTs) in the treatment of osteoporosis. The vast majority of these studies have been carried out with calcium carbonate and with cholecalciferol as the metabolite of vitamin D, and, therefore, the most physiological form7, in patients with different levels of risk of osteoporosis and, even some of them, with objectively diagnosed osteoporosis.
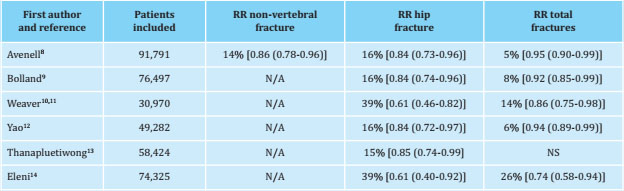
Most of the meta-analyzes of these RCTs have shown a reduction in the risk of fractures, both vertebral and non-vertebral, including hip fractures, the latter undoubtedly the most relevant from the point of view of morbidity and mortality and social health impact. As many of the RCTs mentioned were carried out in the 1980s and nineties, with perhaps different clinical research methodologies in bone mineral metabolism, we have focused our review mainly on the most recent meta-analyzes, that is, those published in the last decade.
Thus, in 2014 the data of a systematic review carried out according to the Cochrane methodology on the role of vitamin D in the prevention of fractures in postmenopausal women and elderly men were published. This work included data from 91,791 patients (including non-institutionalized, institutionalized, and even hospitalized) with different risks of osteoporotic fracture, from 53 RCTs. Selected 10 RCTs (n=49,976) in which joint supplementation of calcium and vitamin D was used (the majority carried out with cholecalciferol as the form of vitamin D used), the researchers concluded that calcium and vitamin D reduced the risk of fracture statistically significant (RR: 0.95; 95% CI -95% confidence interval-: 0.90-0.99). Furthermore, by type of fracture -good quality evidence again- they found statistically significant risk reductions for both hip fracture (9 RCTs; n=49,853; RR: 0.84; 95% CI: 0.73-0.96), as for other non-vertebral fractures (8 RCTs; n=10,380; RR: 0.86; 95% CI: 0.78-0.96). The analysis did not detect a statistically significant risk reduction associated with treatment with calcium and vitamin D in relation to vertebral fractures8, although it is known that this type of osteoporotic fracture usually has a better prognosis and fewer complications than the previous ones, sometimes even asymptomatically.
That same year, Bolland and Reid's research group in New Zealand, well known in the field of bone mineral metabolism for their unfavorable opinion of the need for calcium and vitamin D supplementation, published a sequential meta-analysis. In this paper, along with other extra-osseous health parameters, they analyzed the reduction in fracture risk appearance. According to their cut-off point of minimum risk reduction of 15% as a clinically significant limit, they did not find treatment with calcium and vitamin D relevant in reducing the risk of total fractures or hip fracture. However, according to the results of their own analysis, statistical significance was reached in total fractures, with a risk reduction of 8% (RR: 0.92; 95% CI: 0.85-0.99), and even more so in hip fracture, with a risk reduction that reached 16% (RR: 0.84; 95% CI: 0.74-0.96; p=0.009)9.
Another study was carried out with the support of the US NOF (National Osteoporosis Foundation), encompassing data from 30,970 individuals grouped in a total of 8 RCTs to analyze effects on the incidence of total fractures and 6 RCTs regarding only hip fracture. The results pointed to a positive effect of calcium and vitamin D treatment, again cholecalciferol in almost all RCTs, achieving a risk reduction of 14% (RR: 0.86; 95% CI: 0.75-0.98) for total fractures, and with a robust risk reduction of up to 39% (95% CI: 0.46-0.82) for hip fractures10,11.
Finally, 3 studies with positive results have recently been published: a meta-analysis of 6 RCTs grouping data from 49,282 patients that yielded a discrete, albeit statistically significant, risk reduction in favor of the combined calcium/vitamin D treatment of 6% of total fractures (RR: 0.94; 95% CI: 0.89-0.99), and more relevant in terms of hip fracture, reaching a 16% risk reduction (RR: 0.84; 95% CI % 0.72-0.97)12. Another that analyzed data from up to 47 RCTs (n=58,424) found a statistically significant reduction in risk of falls of 0.88 (95% CI: 0.821-0.945; p<0.01) for cholecalciferol and calcium and, additionally, reduction risk of total fractures of 0.85 (95% CI: 0.741-0.996; p=0.045)13. A third meta-analysis also concluded significant reductions in the risk of osteoporotic fractures, both total and hip14. Table 1 shows a summary of the results of the aforementioned meta-analyzes.
Meta-analysis with negative results
Probably the work with the greatest impact in this regard was that published by the group by Zhao et al., who carried out a meta-analysis with data from 33 RCTs that included 51,145 non-institutionalized adults over 50 years of age at risk of fracture. These investigators did not find statistically significant risk reductions from the combination of calcium and vitamin D in hip fractures (RR: 1.09; 95% CI: 0.85-1.39) or in other non-vertebral fractures (RR: 0.88; 95% CI: 0.75-1.03); neither in vertebral fractures (RR: 0.63; 95% CI: 0.29-1.40), nor in total fractures (RR: 0.90; 95% CI: 0.78-1.04)15. This meta-analysis has subsequently received some criticism, as it could have had some methodological biases such as: 1) the exclusion of RCTs of institutionalized patients, usually at higher risk of fracture than non-institutionalized patients and with lower 25(OH)D levels and, therefore, more sensitive to the effect of supplementation; 2) the inclusion of numerous RCTs with treatment follow-ups too short (less than 12 months) to detect positive effects; 3) the fact that in one of the most important RCTs included for data analysis (known as the WHI study -Women's Health Initiative-) adherence to supplementation was notably low16; and 4) the inclusion of several RCTs in which the form of vitamin D supplementation was by oral or intramuscular bolus mega-doses, which have been clearly relegated from routine clinical practice due to their demonstrated negative effect of increasing the risk of falls and fractures17.
Along the same lines, in 2019, another meta-analysis from another research group was published with also negative results18. In this meta-analysis, some of the methods criticized in the previous work were repeated, such as the non-inclusion of RCTs with institutionalized patients, as well as the inclusion of RCTs in which megadoses of vitamin D were used.
Calcium and vitamin D in combination with drugs used in the treatment of osteoporosis and clinical guidelines
The evidence on the need to combine these drugs
Apart from the intrinsic activity of calcium and vitamin D supplementation in the prevention of osteoporotic fractures, it should be noted that the large RCTs carried out for the regulatory approval of the drugs we use for the treatment of osteoporosis have been carried out by administering to all patients calcium and vitamin D supplements. Regardless of the pharmacological class, whether they are bisphosphonates, PTH analogues, RANK ligand inhibitors or any other mechanisms of action, it is of great importance that these drugs are accompanied by calcium and vitamin D so that they can produce an optimal benefit/risk balance in patients with osteoporosis.
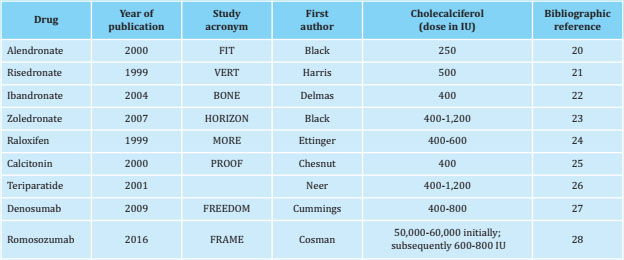
The form of vitamin D used to accompany these antiosteoporotic drugs in their respective reference RCTs was always cholecalciferol, and none of them used intermediate vitamin D metabolites such as calcifediol, nor hormone D (calcitriol)19. A summary of the different reference studies can be seen in table 2.
Recommendations of the clinical guidelines of the societies interested in osteoporosis
As far as Spain is concerned, the Spanish Society of Rheumatology (SER)29, the Spanish Society for Bone Research and Mineral Metabolism (SEIOMM)30, the Spanish Society of Endocrinology and Nutrition (SEEN)31, the SEMFYC (Spanish Society of Family and Community Medicine - rheumatological diseases working group)32 or the Spanish Association for the Study of Menopause (AEEM)33, just to mention some of those that we have found most relevant, recommend the use of calcium and vitamin D supplements in the therapeutic management of osteoporosis of different origin.
Similarly, at the international level, it is recommended by the following societies: European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) in conjunction with the advisory committees and national societies of the International Osteoporosis Foundation (IOF)34; British National Osteoporosis Guideline Group (NOGG )35; National Osteoporosis Foundation (NOF)36, and the joint American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE)3 in the USA; and Endocrine Society (ES), together with the European Society of Endocrinology (ESE)37.
In table 3 we summarize the recommendations made by the scientific societies mentioned above on the supplementation of calcium and, especially, vitamin D.
Table 3. List of recently published guidelines from national and international scientific societies specialized in the clinical management of osteoporosis that recommend supplementation with calcium and vitamin D
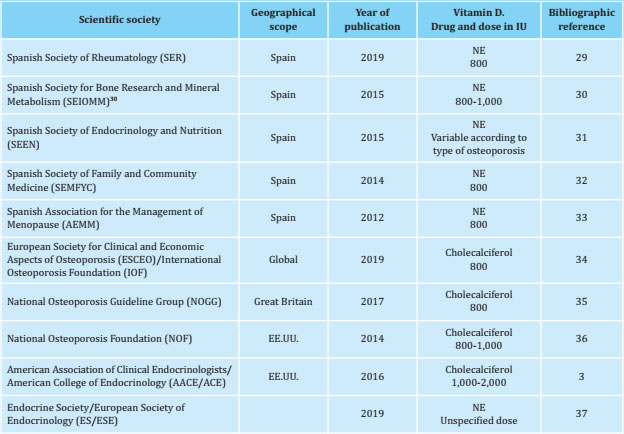
NE: vitamin D with unspecified drug.
Despite the fact that these scientific societies recommend the joint administration of calcium and vitamin D with the indicated treatment for osteoporosis, it is surprising and at the same time worrying that in our country there is still a significant proportion of patients, close to 40%, who start treatments for osteoporosis without the accompaniment of supplementation with calcium and vitamin D38.
Drugs of choice and future dosage trends
Although it seems quite evident that patients with osteoporosis and vitamin D deficiency should be treated with calcium and vitamin D, it is also true that there is no solid scientific evidence and, therefore, no consensus among scientific societies, regarding the dose to use. However, there is a clear trend in this regard:
Calcium
The most widely used form of calcium in our country is undoubtedly calcium carbonate39, a calcium salt with greater bio-availability of element calcium than others also available, but less common, such as calcium citrate40.
As for the appropriate amounts of calcium in the context of osteoporosis, since 2010 the most replicated and internationally accepted reference is the Food and Nutrition Board of the Institute of Medicine (IOM) guideline of the United States which recommends a daily intake (contained in the diet or through exogenous supplementation when the above is not possible) of 1,200 mg of calcium for men over 70 years old or women over 51 years old4. Unfortunately, the majority of the population at risk of osteoporosis do not ingest the 1,200 mg/day recommended by the IOM. This has recently been verified in the epidemiological study ANIBES (Anthropometry, Intake and Energy Balance in Spain), published in 2017. Carried out through surveys on nutritional habits of more than 2,000 individuals of a very wide age range in our country, it estimated that the average daily amounts of calcium ingested through the diet of women and men older than 65 years were 662 and 629 mg, respectively41. Therefore, if we were to reach the IOM guideline, we would have to supplement with about 600 mg of calcium daily in the form of exogenous calcium carbonate supplement to reach 1,200 mg/day.
Vitamin D
Cholecalciferol is the form of vitamin D most used in RCTs and therefore the metabolite specifically recommended in most of the aforementioned published clinical guidelines on the management of osteoporosis. We do not have conclusive scientific evidence that establishes the recommended daily doses in the treatment of osteoporosis in a consensual way. It is possible that the trend is to increase the daily 800-1,000 IU of vitamin D that is used mostly in routine clinical practice at higher doses, since this has been the norm up to now in the design of clinical trials.
Thus, more than 30 years ago, the reference trials with alendronate were designed with a supplement of vitamin D of 250 IU/day20, an amount that increased 4 years later to 400 IU/day with ibandronate22, and by 2009 reached 800 cholecalciferol IU/day in patients with baseline 25(OH) D levels of 12-20 ng/ml or 400 IU/day for levels greater than 20 ng/ml in the FREEDOM study with denosumab27 (average in the first month of 600 IU/day treatment). Thus, we observe that this upward trend is consolidated in the most recent reference study with romosozumab, published in 2016, and in whose design a loading dose of 50,000-60,000 IU/day of cholecalciferol was established (the use of vitamin D2 or ergocalciferol was also allowed) and then daily doses of 600-800 IU for patients with baseline levels of 25 (OH) D between 20 and 40 ng/ml28, which would mean an average in the first month of treatment of about 2,500 IU/day (see figure 1).
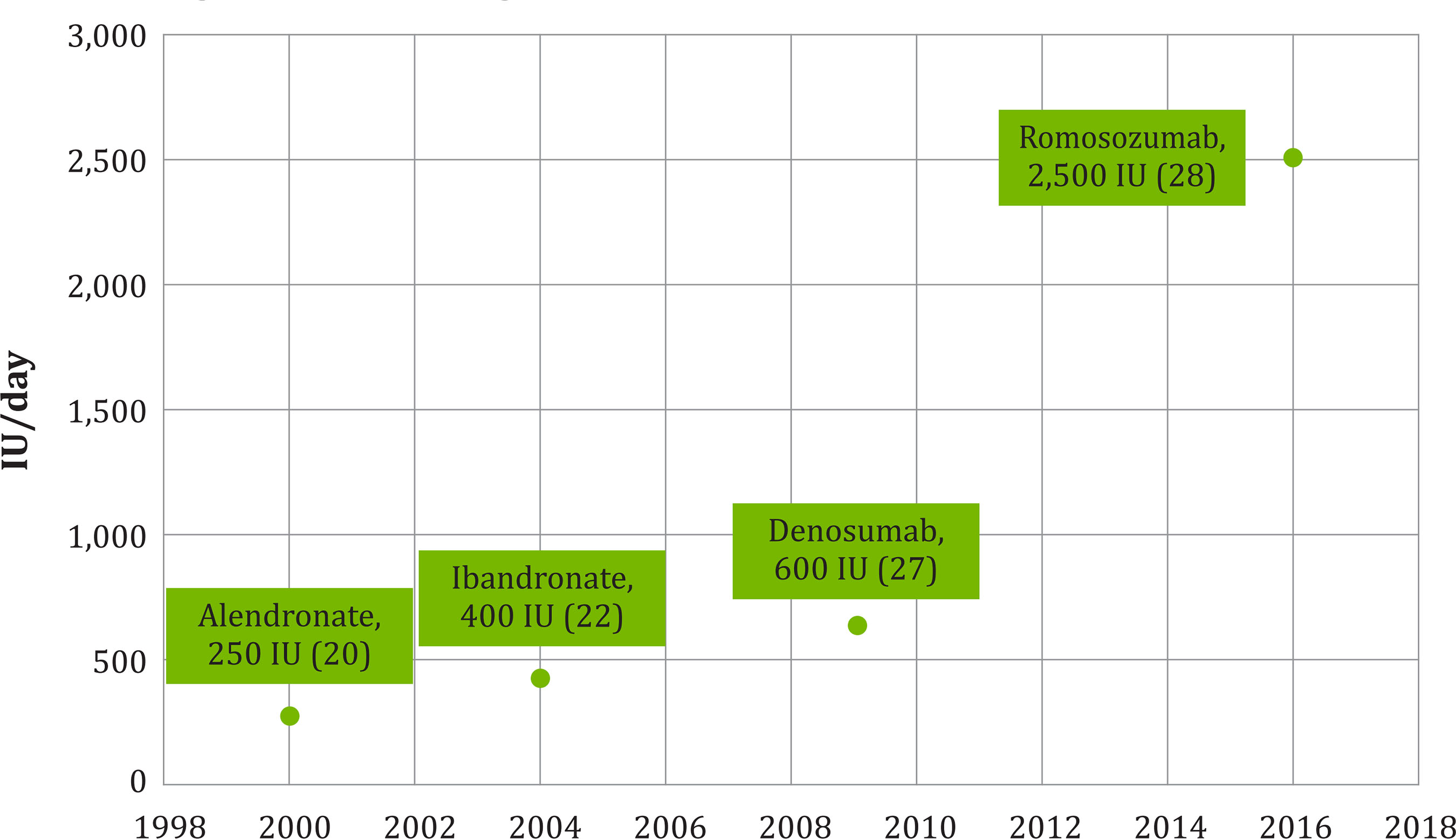
Figure 1. Evolution of the daily doses of the first month of treatment (IU/day) of cholecalciferol associated with anti-osteoporotic drugs. Year of publication, anti-osteoporotic drug, dose and bibliographic reference (in parentheses) are indicated
In our opinion, it would be advisable to transfer this trend of increasing the dose of cholecalciferol in drugs under development to our usual clinical practice of supplementation in patients with vitamin D deficiency and osteoporosis. Similarly, some renowned scientific societies, in their clinical guidelines and consensus documents, recommend a supplementation of up to 2,000 IU/day of cholecalciferol in patients with osteoporosis. Among these groups, the International Osteoporosis Foundation (IOF)42, the Endocrine Society (ES)43 or the American Association of Clinical Endocrinologists/American College of Endocrinology (AACE/ACE)3 stand out.
We will be better able to reach the optimal levels of 25(OH)D higher than 30 ng/ml widely recommended by the main scientific societies which manage osteoporosis if we treat patients with 2,000 IU/day than if we treat them only with 8001,000 IU/day, and that this can produce an additional clinical benefit in osteoporosis. In fact, there are already studies that provide some evidence that this could be the case. The Zurich Hip Fracture Trial carried out by the Dawson-Hugues and Bischoff-Ferrari groups, a clinical trial in which it was compared in a bi-factorial way the administration of 2,000 IU/day or 800 IU/day of cholecalciferol to 173 patients who had suffered a hip fracture, in combination or not with a physical exercise program for 12 months, concluding that the administration of 2,000 IU/day was associated to a more limited deterioration in the quality of life between months 6 and 12, evaluated by means of the EuroQol EQ-5D-3L scale scores44; also, a systematic review of the literature that analyzed 12 publications on different guidelines for supplementation with cholecalciferol in menopausal women at risk of osteoporosis with vitamin D deficiency, in which the authors observed that only daily doses of 2,000 IU/day increased 25 (OH) D levels consistently above 30 ng/ml45.
CONCLUSION
To date, scientific evidence confirms the need to treat all patients with osteoporosis and vitamin D deficiency with calcium and vitamin D (preferably cholecalciferol), regardless of their other osteoporosis treatment. The daily doses of cholecalciferol to be used should reach at least 2,000 IU.
Bibliografía
1 Shahnazari B, Moghimi J, Foroutan M, Mirmohammadkhani M, Ghorbani A. Comparison of the effect of vitamin D on osteoporosis and osteoporotic patients with healthy individuals referred to the Bone Density Measurement Center. Biomol Concepts. 2019;10(1):44-50. [ Links ]
2 Barrionuevo P, Kapoor E, Asi N, Alah-dab F, Mohammed K, Benkhadra K, et al. Efficacy of pharmacological therapies for the prevention of fractures in postmenopausal women: a network meta-analysis. J Clin Endocrinol Metab. 2019;104(5):1623-1630. [ Links ]
3 Camacho PM, Petak SM, Binkley N, Clarke BL, Harris ST, Hurley DL, et al. American Association of Clinical Endo-crinologisy and American College of Endocrinology. Clinical Practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis - 2016. En-docr Pract. 2016;22(Suppl 4):1-42. [ Links ]
4 Ross AC, Taylor CL, Yaktine AL, del Valle HB. Committee to Review Dietary Reference Intakes for Vitamin D and Calcium Food and Nutrition Board. Institute of Medicine (IOM). Washington DC: The National Academies Press; 2011. [ Links ]
5 Quesada Gómez JM, Nogués X, Sosa Henríquez M, Bouillon R. Vitamin D supplementation and musculoskeletal health. A controversial necessity. Med Clin (Barc). 2019;153(11):432-436. [ Links ]
6 Kuchuk NO, van Schoor NM, Pluijm SM, Chines A, Lips P. Vitamin D status, parathyroid function, bone turnover, and BMD in postmenopausal women with osteoporosis: global perspective. J Bone Miner Res. 2009;24(4):693-701. [ Links ]
7 Sosa-Henríquez M. Cholecalciferol and calcifediol for vitamin D supplementation. Osteoporos Int. 2020;31(2):391-392. [ Links ]
8 Avenell A, Mak JC, O'Connell D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst Rev. 2014;(4):CD 000227. [ Links ]
9 Bolland MJ, Grey A, Gamble GD, Reid IR. The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential metaanalysis. Lancet Diabetes Endocrinol. 2014;2(4):307-320. [ Links ]
10 Weaver CM, Alexander DD, Boushey CJ, Dawson-Hughes B, Lappe JM, Le-Boff MS, et al. Calcium plus vitamin D supplementation and risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27(1):367-376. [ Links ]
11 Weaver CM, Dawson-Hughes B, Lappe JM, Wallace TC. Erratum and additional analyses re: Calcium plus vitamin D supplementation and the risk of fractures: an updated meta-analysis from the National Osteoporosis Foundation. Osteoporos Int. 2016;27(8): 2643-2646. [ Links ]
12 Yao P, Bennett D, Mafham M, Lin X, Chen Z, Armitage J, et al. Vitamin D and Calcium for the Prevention of Fracture: A Systematic Review and Meta-analysis. JAMA Netw Open. 2019;2(12):e1917789. [ Links ]
13 Thanapluetiwong S, Chewcharat A, Takkavatakarn K, Praditpornsilpa K, Eiam-Ong S, Susantitaphong P. Vitamin D supplement on prevention of fall and fracture: A Meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99(34):e21506. [ Links ]
14 Eleni A, Panagiotis P. A systematic review and meta-analysis of vitamin D and calcium in preventing osteoporotic fractures. Clin Rheumatol. 2020;39 (12):3571-3579. [ Links ]
15 Zhao JG, Zeng XT, Wang J, Liu L. Association between calcium or vitamin D supplementation and fracture incidence in community-dwelling older adults: a systematic review and metaanalysis. JAMA. 2017;318(24):2466-2482. [ Links ]
16 Jackson RD, LaCroix AZ, Gass M, Wallace RB, Robbins J, Lewis CE, et al.; Women's Health Initiative Investigators. Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med. 2006;354(7):669-683. [ Links ]
17 Bischoff-Ferrari HA, Dawson-Hughes B, Willett WC. Issues of trial selection and subgroup considerations in the recent meta-analysis of Zhao and colleagues on fracture reduction by calcium and vitamin D supplementation in community-dwelling older adults. Osteoporos Int. 2018;29(9):2151-2152. [ Links ]
18 Hu ZC, Tang Q, Sang CM, Tang L, Li X, Zheng G, et al. Comparison of fracture risk using different supplemental doses of vitamin D, calcium or their combination: a network meta-analysis of randomized controlled trials. BMJ Open. 2019;9(10):e024595. [ Links ]
19 Reyes Domínguez AI, Gómez de Tejada Romero MJ, Sosa Henríquez M. La vitamina D. Fisiología. Su utilización en el tratamiento de la osteoporosis. Rev Osteoporos Metab Miner. 2017;9(Supl 1): S5-9. [ Links ]
20 Black DM, Thompson DE, Bauer DC, Ensrud K, Musliner T, Hochberg MC, et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85(11):4118-4124. [ Links ]
21 Harris ST, Watts NB, Genant HK, McKe-ever CD, Hangartner T, Keller M, et al. Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral Efficacy with Risedro-nate Therapy (VERT) Study Group. JAMA.1999;282(14):1344-1352. [ Links ]
22 Delmas PD, Recker RR, Chesnut CH 3rd, Skag A, Stakkestad JA, Emkey R, et al. Daily and intermittent oral iban-dronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int. 2004;15 (10):792-798. [ Links ]
23 Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, et al. Once-ye-arly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809-1822. [ Links ]
24 Ettinger B. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene. JAMA. 1999;282(7):637. [ Links ]
25 Chesnut CH, Silverman S, Andriano K, Genant H, Gimona A, Harris S, et al. A randomized trial of nasal spray salmon calcitonin in postmenopausal women with established osteoporosis: the Prevent Recurrence of Osteoporotic Fractures Study. Am J Med. 2000; 109:267-276. [ Links ]
26 Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster J-Y, et al. Effect of parathyroid hormone (1-34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med. 2001;344(19): 1434-1441. [ Links ]
27 Cummings SR, Martin JS, McClung MR, Siris ES, Eastell R, Reid IR, et al. Deno-sumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8): 756-765. [ Links ]
28 Cosman F, Crittenden DB, Adachi JD, Binkley N, Czerwinski E, Ferrari S, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375(16): 1532-1543. [ Links ]
29 Naranjo Hernández A, Díaz Del Campo Fontecha P, Aguado Acín MP, Arboleya Rodríguez L, Casado Burgos E, Castañeda S, et al. Recommendations by the Spanish Society of Rheumatology on Osteoporosis. Reumatol Clin. 2019;15 (4):188-210. [ Links ]
30 González-Macías J, Del Pino-Montes J, Olmos JM, Nogués X; en nombre de la Comisión de Redacción de las Guías de Osteoporosis de la SEIOMM. Clinical practice guidelines for postmenopausal, glucocorticoid-induced and male osteoporosis. Spanish Society for Research on Bone and Mineral Metabolism (3rd updated version 2014). Rev Clin Esp. 2015;215(9):515-526. [ Links ]
31 Reyes-García R, García-Martín A, Var-savsky M, Rozas-Moreno P, Cortés-Berdoncés M, Luque-Fernández I, et al.; en representación del Grupo de trabajo de osteoporosis y metabolismo mineral de la Sociedad Española de Endocrinología y Nutrición. Update of recommendations for evaluation and treatment of osteoporosis associated to endocrine and nutritional conditions. Working Group on Osteoporosis and Mineral Metabolism of the Spanish Society of Endocrinology. Endocrinol Nutr. 2015;62(5):e47-56. [ Links ]
32 Sociedad Española de Medicina de Familia y Comunitaria - grupo de trabajo de enfermedades reumatológicas. Osteoporosis. Manejo: prevención, diagnóstico y tratamiento. SEMFYC Ediciones. Barcelona, 2014. ISBN: 978-84-1503743-9. Depósito legal: B 9573-2014. [ Links ]
33 Asociación Española para el Manejo de la Menopausia. Menoguía. Osteoporosis. Barcelona. Primera edición: 2012. Depósito legal: B:18.824-2012. [ Links ]
34 Kanis JA, Cooper C, Rizzoli R, Reginster JY; Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30(1):3-44. [ Links ]
35 Compston J, Cooper A, Cooper C, Git-toes N, Gregson C, Harvey N, et al.; National Osteoporosis Guideline Group (NOGG). UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017;12(1):43. [ Links ]
36 Cosman F, de Beur SJ, LeBoff MS, Le-wiecki EM, Tanner B, Randall S, et al.; National Osteoporosis Foundation. Clinician's guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-2381. [ Links ]
37 Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2019; 104(5):1595-1622. [ Links ]
38 Carbonell C, Diez A, Calaf J, Caloto MT, Nocea G, Lara N. Initial treatment trends in patient with osteoporosis: use of antiresorptive agents and pharmacologic supplements (calcium and vitamin D) in clinical practice. Reuma-tol Clin. 2012;8(1):3-9. [ Links ]
39 CIMA (Centro de Información on-line de Medicamentos de la Agencia Española de Medicamentos y Productos Sanitarios). https://cima.aemps.es/cima/pu-blico/home.html. Consultado el 31 de mayo 2021. [ Links ]
40 Wang H, Bua P, Capodice J. A comparative study of calcium absorption following a single serving administration of calcium carbonate powder versus calcium citrate tablets in healthy premenopausal women. Food Nutr Res. 2014;58. [ Links ]
41 Olza J, Aranceta-Bartrina J, González-Gross M, Ortega RM, Serra-Majem L, Varela-Moreiras G, et al. reported dietary intake, disparity between the reported consumption and the level needed for adequacy and food sources of calcium, phosphorus, magnesium and vitamin d in the Spanish population: findings from the ANIBES Study. Nutrients. 2017;9(2). [ Links ]
42 Dawson-Hughes B, Mithal A, Bonjour JP, Boonen S, Burckhardt P, Fuleihan GE, et al. IOF position statement: vitamin D recommendations for older adults. Osteoporos Int. 2010;21(7):1151-1154. [ Links ]
43 Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al.; Endocrine Society. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-1930. [ Links ]
44 Renerts K, Fischer K, Dawson-Hughes B, Orav EJ, Freystaetter G, Simmen HP, et al. Effects of a simple home exercise program and vitamin D supplementation on health-related quality of life after a hip fracture: a randomized controlled trial. Qual Life Res. 2019;28(5): 1377-1386. [ Links ]
45 Tayem Y, Alotaibi R, Hozayen R, Has-san A. Therapeutic regimens for vitamin D deficiency in postmenopausal women: a systematic review. Prz Me-nopauzalny. 2019;18(1):57-62. [ Links ]





![Metástasis maxilar por tumor miofibroblástico pulmonar detectada en estudio [18F]FDG PET/TC](/img/es/next.gif)





 texto en
texto en