Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Ars Pharmaceutica (Internet)
versión On-line ISSN 2340-9894
Ars Pharm vol.56 no.2 Granada 2015
https://dx.doi.org/10.4321/S2340-98942015000200005
Prescribing pattern of antihypertensive drugs in diabetic patients of Southern Province, Kingdom of Saudi Arabia
El patrón de prescripción de los fármacos antihipertensivos en los pacientes diabéticos de la Provincia del Sur, Reino de Arabia Saudita
Sirajudeen Shaik Alavudeen, Khaled Mohammed Alakhali, Shaik Mohammad Asif Ansari and Noohu Abdulla Khan
Department of Clinical Pharmacy, College of Pharmacy, King Khalid University, Abha, Kingdom of Saudi Arabia
ABSTRACT
Background: Hypertension is extremely prevalent in patients with diabetes. Limited data exist on utilization patterns of antihypertensive in this population are consistent with evidence-based practice guidelines.
Objective: To evaluate utilization patterns of antihypertensive agents among diabetic patients with hypertension.
Design: Retrospective descriptive cross sectional.
Patients / Participants: 149 patients with diabetes and hypertension from outpatient department at Family Medicine Hospital, Ahaderfieda. Khamis Mushait, K.S.A.
Results: Over 43% of patients were receiving calcium channel blockers (CCB), 36.2 % of received angiotensin converting enzyme inhibitors (ACEI), followed by angiotensin receptor blockers (ARBs) (34.9%), diuretics (34.2%) and β -blockers (16.2%). Patients on monotherapy were mostly receiving CCB (34.3%) and ACEI (29.9%). The majority (55.03%) of treated patients were on multidrug regimens. In patients with coronary artery disease (CAD), a diuretic with ACEI (25%) and calcium channel blocker with angiotensin receptor blocker (25%) was most commonly prescribed.
Conclusions: Patterns of antihypertensive therapy were generally consistent with international guidelines. Areas of improvement include increasing ACEI/ARB and diuretic use, decreasing the number of untreated patients, and increasing the proportion of patients with controlled BP in this population.
Key words: Hypertension, Diabetes, Antihypertensive agents.
RESUMEN
Antecedentes: La hipertensión es muy frecuente en los pacientes con diabetes. Existen datos limitados sobre los patrones de utilización de antihipertensivos en esta población consistentes con las guías de práctica basadas en la evidencia.
Objetivo: Evaluar los patrones de utilización de antihipertensivos en los pacientes diabéticos con hipertensión.
Diseño: Estudio retrospectivo descriptivo transversal.
Pacientes / Participantes: 149 pacientes con diabetes e hipertensión, del departamento de pacientes ambulatorios en el Hospital de Medicina Familiar, Ahaderfieda. Khamis Mushait, K.S.A.
Resultados: Más del 43% de los pacientes estaban recibiendo bloqueadores del canal de calcio (CCB), el 36,2% recibían inhibidores de la enzima convertidora de angiotensina (IECA), seguido de los bloqueadores de los receptores de angiotensina (BRA) (34,9%), diuréticos (34,2%) y bloqueadores β (16,2 %). Los pacientes en monoterapia fueron la mayoría recibiendo CCB (34,3%) e IECA (29,9%). La mayoría (55,03%) de los pacientes tratados se encontraban en regímenes de múltiples fármacos. En los pacientes con enfermedad de la arteria coronaria (CAD), se les prescribió con mayor frecuencia diurético con IECA (25%) y bloqueador de canales de calcio con bloqueador del receptor de angiotensina (25%).
Conclusiones: Los patrones de utilización de antihipertensivos fueron generalmente consistentes con las directrices internacionales. Las áreas de mejora incluyen el aumento de IECA / ARB y el uso de diuréticos, disminuyendo el número de pacientes no tratados, y el aumento de la proporción de pacientes con PA controlada en esta población.
Palabras clave: hipertensión, diabetes, agentes antihipertensivos.
Introduction
Diabetes mellitus and hypertension are interrelated diseases that strongly predispose an individual to atherosclerotic cardiovascular disease 1. The prevalence of coexisting hypertension and diabetes appears to be increasing in Saudi Arabia. The World Health Organization estimates that the number of people with diabetes mellitus is projected to increase almost threefold in Saudi Arabia, from 890,000 in 2000 to a staggering 2,523,000 in 2030 2. Hypertension (HTN), affects about 21% of all Saudi adults between the ages of 18 and 64 years, is an important modifiable risk factor for cerebrovascular disease (CVD) 3. Studies such as Framingham heart study, United Kingdom Prospective Study-39 (UKPDS), Hypertension Optimal Treatment (HOT), Systolic Hypertension in the Elderly Programme (SHEP), Systolic hypertension in Europe (SYST-Eur), Hypertension in the Very Elderly Trial (HYVET-Pilot) indicated that reduction in either isolated systolic or systolic-diastolic hypertension significantly reduces the risk of micro and macro vascular complications and cardiovascular (CV) death or diabetes-related death 4. The Seventh Joint National Committee (JNC 7) and American Diabetes Association (ADA) recommends that blood pressure (BP) in diabetics be controlled to levels of 130/80 mmHg or lower 5. Whatever the goal level, rigorous control of BP is paramount for reducing the progression of diabetic nephropathy to end stage renal disease 6. However, studies consistently demonstrate that most diabetic patients do not achieve recommended levels of BP control, and the majority have a BP of >140/90mmHg 7. Saudi Hypertension Management Guidelines recommend either an ACE-I or an ARB, if ACE-I is not tolerated. If BP targets are not achieved, a thiazide diuretic should be added to those with an e Glomerular Filtration Rate ≥ 30 or a loop diuretic for those with an estimated Glomerular Filtration Rate < 30 8. Some studies have demonstrated the beneficial effects of beta blockers and calcium channel blockers in diabetic hypertensive patients 9. On contrary to above studies, some studies indicate that majority of diabetic patients will require two or more drugs to achieve BP control 8,10,11. The resulting changes in drug use in time and place may have medical, social and economic implications both for the individual patient for populations. These differences need to be identified, explained and corrected if needed. Drug utilization studies are necessary to this effect with a particular focus on socio- demographic characteristics, co-morbid conditions and pattern of anti- hypertensive drugs usage 12. Thus in this context, the present study was conducted to examine the utilization pattern of antihypertensive in hypertensive diabetic patients and also to explore the adherence of prescribing pattern with existing guidelines.
Materials and methods
This study is a retrospective descriptive cross sectional drug utilization study conducted in the outpatient department at Family Medicine Hospital, Ahaderfieda. Khamis Mushait, K.S.A. A total of 149 prescriptions of hypertensive outpatients with diabetes above 18 yrs of age were randomly selected employing systematic sampling. The demographic and medication history of the diabetic hypertensive patients were collected to address the following questions:
1. Which antihypertensive drug classes and combinations, respectively, are applied by general physicians in hypertensive diabetic patients?
2. Did drug treatments differ with respect to certain patient characteristics such as age, gender?
Data analysis
Data analysis was carried out using Microsoft excel. Data were expressed as mean (standard deviation) for continuous variables and as frequency for categorical variables.
Results
One hundred forty nine prescriptions belonging to 81 (54.4 %) females and 68 (45.6%) males were studied. The mean age of the male patients included in the study was found to be 55.2±8.5 years and the mean age of the female students included in this study was found to be 58.1 ± 12.9.
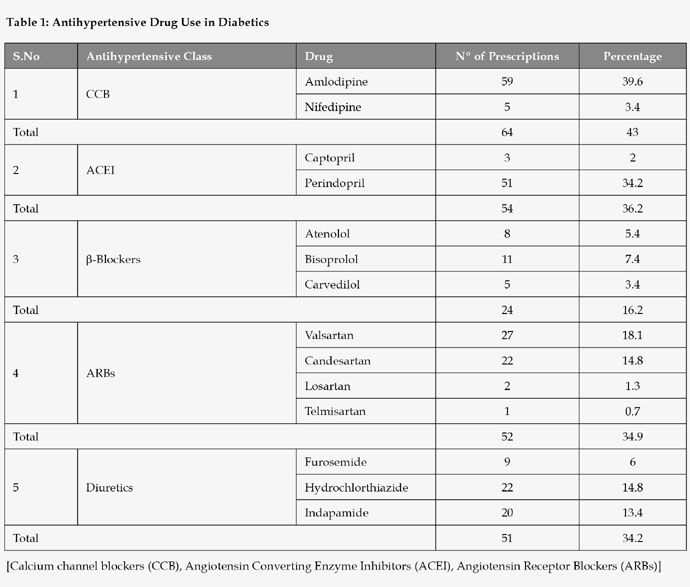
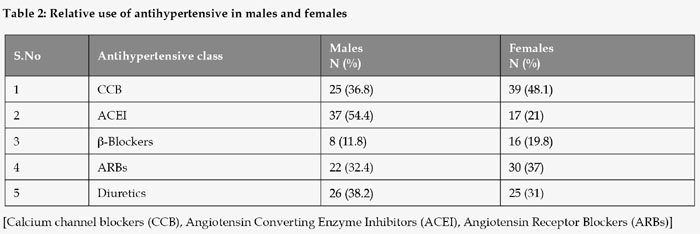
The overall use of antihypertensive in diabetes is shown in Table 1. The utilization of the calcium channel blockers supersedes all other groups of antihypertensive in diabetes with hypertension. Use of the calcium channel blockers is around 43% in hypertensive diabetic patients. Amlodipine is the predominantly used CCB. The ACE inhibitors are the antihypertensive class used the most following the CCB's (36.2%). The use of angiotensin II receptor blockers were also nearly the same as ACE inhibitors among the diabetes patients with diabetes (34.9%). Next to the ARBs, diuretics were used widely among these patients (34.2%) and the loop diuretic furosemide is the least prescribed diuretic in diabetes with hypertension. β-Blockers are the least prescribed antihypertensive in diabetes with hypertension. Table 2 shows the relative use of antihypertensive in both genders. Marked gender based differences have been found to be there between the two groups of diabetes. The utilization of ARBs, β-Blockers and CCBs are more among the female patients whereas the utilization of ACE inhibitors and diuretics are high among the male patients.
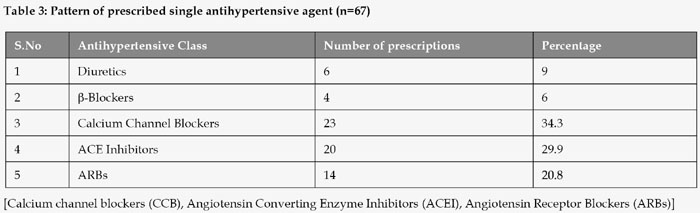
In Table 3 the various antihypertensive drugs and the number of patients in whom they were used under the class of monotherapy revealed that, out of 67 patients who underwent monotherapy for the treatment of hypertension, 23 (34.3%) of the patients were prescribed with CCBs, followed by 20 (29.9 %) with ACE inhibitors, 14 (20.8%) of the patients with ARBs, 6 (9%) of the patients with diuretics and 4 (6%) of the patients with β-blockers.
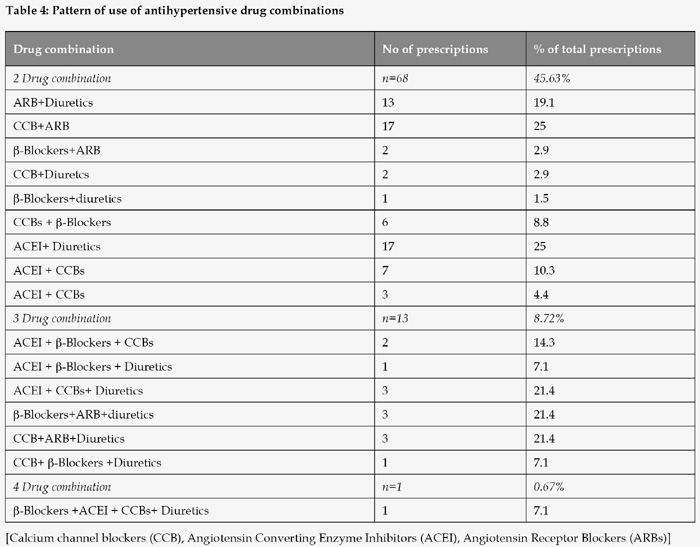
Table 4 reveals that, out of 68 patients in whom two antihypertensive were prescribed, 17(25%) patients were prescribed with a combination of Diuretics & ACE inhibitors and another 17(25%) patients were prescribed with a combination of CCB & ARBs followed by 13 (19.1%) of patients with Diuretics and ARBs, 7(10.3% ) patients with ACE inhibitors, 3 (4.4%)patients with ACE inhibitors and β-Blockers, 2 (2.9%) patients were prescribed with β-Blockers+ARB, another 2 (2.9 %) patients were prescribed with CCB+Diuretcs and 1 (1.5%) was prescribed with β-Blockers+diuretics.
Discussion
We studied patterns of antihypertensive use in patients with diabetes and hypertension, to evaluate whether they were consistent with evidence-based practice guidelines. In present study, ACEI, ARBs and calcium channel blocker were more commonly prescribed drugs, followed by, diuretics and beta-blockers irrespective of mono or poly therapy. Majority of patients were on polytherapy in the present study. As the hypertensive patients were diabetic increased utilization of ACE inhibitors was observed which was in accordance with JNC-7 guidelines which recommend its use for renoprotection in the hypertensive diabetic patients 13. Among all the ACEI, perindropirl (34.2%) was widely prescribed than any other ACEI. This finding is supported by the EUROPA study which indicated that among patients with stable coronary heart disease without apparent heart failure, perindopril can significantly improve outcome14. We found that men were significantly more likely to be prescribed an ACE inhibitor as initial antihypertensive therapy than women (54.4 vs. 21%) this may be due to the fact that men are at high risk of developing atherosclerosis compared to women and also because of the teratogenic risk of ACEI and also reports from clinical trials have consistently documented that women are at higher risk of ACE inhibitor-induced cough than men 15. Though 34.3% of patients received calcium channel blockers as monotherapy, some studies have shown an excess of selected cardiac events in patients treated with dihydropyridine calcium channel blockers (DCCBs) compared with ACEI 16.
In a meta-analysis of 42 trials published by Wald, et al., it was found that combining antihypertensive drugs from two different classes lowered blood pressure five times more than doubling the dose of a single agent 17. In addition to synergistic blood pressure lowering, combination therapy allows for lower dosage requirements of each individual agent. This, in turn leads to decreased side effects, thereby improving compliance 18. In our present study use of multiple drug combinations for controlling blood pressure was also high at 55% compared to those using single drug 44.9% in these patients. Our finding is similar to those observed by Anand et al. 19 and Gu, et al. 20 who indicated that the increased use of multiple antihypertensive drugs apparently has contributed to substantial improvement in BP control in the treated hypertensive population. A combination of diuretics and ACE inhibitor (ACEI) were the important drug combination to be most commonly prescribed in our study and also diuretics were used more often as component of multidrug therapy. This is supported by a previous report which indicated that ACEI-diuretic combinations achieve blood pressure control in approximately 80 percent of patients 21.
In the present investigation, two-drug combinations were mostly prescribed (45.63%), followed by three-drug combinations (8.27%) and four drug combinations (0.67%) (Table 4). In two-drug combinations, a diuretic with ACEI (25%) and calcium channel blocker with angiotensin receptor blocker (25%) was most commonly prescribed as it is a choice for the treatment of the majority of patients with hypertension, particularly those at high risk of a secondary event 22, the combined therapy with an ARB and a CCB has a potentially useful antiproteinuric effect in patients with type 2 diabetic nephropathy, even when their renal function is reduced 23 followed by an ARB with a diuretic (19.1 %). ONEAST study results confirm that ARB / diuretic combinations reduce BP further than monotherapies in hypertensive diabetic subjects with an acceptable safety profile 23.
Conclusions
Although this study lacks both breadth and depth, however it provides a reasonable indication of the prescription patterns of antihypertensive agents in diabetic hypertensive population. Our findings suggest that CCBs and ACE inhibitors were used in large proportion of diabetic hypertensive patients and the pattern of antihypertensive therapy was generally consistent with JNC 7 guidelines, those being the current guidelines at the time of our study. However, there remains potential room for improvement in drug utilization and a critical need for better blood pressure control. Further research is needed to qualify rationale for choice of drug based on demographic data, economic status, concomitant conditions and complications to give additional insight into prescribing patterns of antihypertensive in diabetic patients of Aseer region of Saudi Arabia.
Competing interest: There is no conflict of interest.
Fundings: This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
References
1. El-Hazmi MA, Warsy AS. Association of hypertension and non-insulin-dependent diabetes mellitusin the Saudi population. Ann Saudi Med. 2001;21(1-2):5-8. [ Links ]
2. Al-Baghli NA, Al-Ghamdi AJ, Al-Turki KA, Al Elq AH, El-Zubaier AG, Bahnassy A. Prevalence of diabetes mellitus and impaired fasting glucose levels in the Eastern Province of Saudi Arabia: results of a screening campaign. Singapore Med J. 2010; 51(12):923-30. [ Links ]
3. Preliminary Report on the Results of Monitoring of Risk Factors for Non-Communicable Diseases in the Kingdom of Saudi Arabia. Riyadh: King Fahad National Library; 2005. [ Links ]
4. Dhanaraj E, Raval A, Yadav R, Bhansali A, Tiwari P. Prescription Pattern of Antihypertensive Agents in T2DM Patients Visiting Tertiary Care Centre in North India. Int J Hypertens. 2012; 2012:520915. doi: 10.1155/2012/520915. [ Links ]
5. Chobanian AV, et al.. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289(19):2560-72. [ Links ]
6. Shah J, Khakhkhar T, Bhirud S, Shah RB, Date S. Study of utilization pattern of anti-hypertensive drugs in hypertensive diabetic patients with or without reduced renal function at tertiary care teaching hospital. Int J Med Sci Public Health. 2013;2(2):175-180. [ Links ]
7. Berlowitz DR1, Ash AS, Hickey EC, Glickman M, Friedman R, Kader B. Hypertension management in patients with diabetes: the need for more aggressive therapy. Diabetes Care. 2003; 26(2):355-9. [ Links ]
8. Saudi Hypertension Management Guidelines, Saudi Hypertension Management Society, 2011. [ Links ]
9. Arauz-Pacheco C, Parrott MA, Raskin P. The treatment of hypertension in adult patients with diabetes. Diabetes Care. 2002;25(1):134-47. [ Links ]
10. Sowers JR, Haffner S. Treatment of cardiovascular and renal risk factors in the diabetic hypertensive. Hypertension 2002;40:781-8. [ Links ]
11. Sowers JR, Reed J. 1999 Clinical Advisory Treatment of Hypertension and Diabetes. J Clin Hypertens (Greenwich) 2000;2:132-3. [ Links ]
12. Sharminder Kaur S , Gupta S , Kumar D , Lal M , Gilani Z. Prescribing pattern of antihypertensive drugs in a tertiary care hospital in Jammu- A Descriptive study. JK-Practitioner 2012;17(4): 38-41. [ Links ]
13. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program. Source Bethesda (MD): National Heart, Lung, and Blood Institute (US); 2004. Report No.:04-5230. [ Links ]
14. Fox KM; EURopean trial On reduction of cardiac events with Perindopril in stable coronary Artery disease Investigators. Efficacy of perindopril in reduction of cardiovascular events among patients with stable coronary artery disease: randomised, double-blind, placebo-controlled, multicentre trial (the EUROPA study). Lancet. 2003;362(9386):782-8. [ Links ]
15. McAlister FA, Campbell NR, Duong-Hua M, Chen Z, Tu K. Antihypertensive medication prescribing in 27,822 elderly Canadians with diabetes over the past decade. Diabetes Care. 2006;29(4):836-41. [ Links ]
16. Richards M. The Safety of Calcium Antagonists: An Update. Prescriber Update. 2000;19: 4-13. [ Links ]
17. Wald DS, Law M, Morris JK, et al.. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med. 2009; 122:290-300. [ Links ]
18. Vogel Anderson KL, Combination Therapy in Hypertension Management. US Pharm. 2012;37(6):46-50. [ Links ]
19. Kale A, Maniyar YA. Prescribing patterns of antihypertensive drugs in a tertiary care hospital. Sch Acad J Pharm. 2013; 2(5):416-418. [ Links ]
20. Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health and Nutrition Examination Survey, 2001 to 2010. Circulation. 2012; 126(17):2105-14. [ Links ]
21. Skolnik NS, Beck JD, Clark M. Combination antihypertensive drugs: recommendations for use. Am Fam Physician. 2000; 61(10):3049-56. [ Links ]
22. Escobar C, Barrios V. Calcium channel blocker-based combination therapy. The best approach in the treatment of high-risk hypertension? Int J Clin Pract. 2008; 62(5):670-2. [ Links ]
23. Kalra S, Kalra B, Agrawal N. Combination therapy in hypertension: An update. Diabetol Metab Syndr. 2010; 2(1):44. doi: 10.1186/1758-5996-2-44. [ Links ]
![]() Correspondence:
Correspondence:
Dr. Shaik Mohammad Asif Ansari
Department of Clinical Pharmacy
College of Pharmacy
King Khalid University
Abha, Kingdom of Saudi Arabia
Email: dr.maas@yahoo.com
Received: 20.10.2014
Accepted: 06.03.2015