Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
REC: Interventional Cardiology
versión On-line ISSN 2604-7276versión impresa ISSN 2604-7306
REC Interv Cardiol ES vol.5 no.4 Madrid oct./dic. 2023 Epub 04-Mar-2024
https://dx.doi.org/10.24875/recic.m23000390
Scientific letters
Drug-eluting balloon angioplasty for bifurcated chronic total coronary occlusion
aÁrea de Gestión Clínica del Corazón, Hospital Universitario Central de Asturias, Oviedo, Asturias, Spain
bInstituto de Investigación Sanitaria del Principado de Asturias, Oviedo, Asturias, Spain
cDepartamento de Medicina, Facultad de Medicina, Universidad de Oviedo, Oviedo, Asturias, Spain
To the Editor,
This is the case of a 67-year-old woman admitted due to a 6-month history of exertional angina. Stress echocardiography showed severe anterior wall ischemia. The patient was referred for coronary angiography that revealed the presence of a chronic total coronary occlusion of the proximal left anterior descending coronary artery (LAD) immediately before the bifurcation with the first diagonal branch (D1) from the septal collaterals of the right coronary artery (figure 1A, video 1 of the supplementary data). The patient signed the written informed consent, and a chronic total coronary occlusion recanalization was performed 6 months after the index angiography.
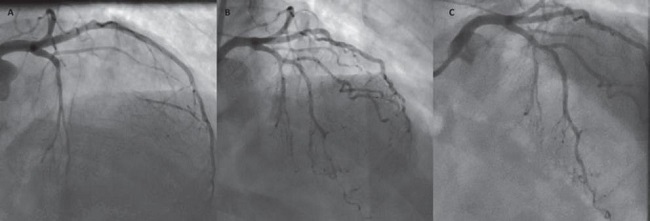
Figure 1. A: cranial view of chronic total coronary occlusion of proximal left anterior descending coronary artery (LAD). B: postoperative final angiographic result with a small non-flow limiting dissection in the mid-LAD treated conservatively. C: angiographic control at 6 months showed great outcomes using drug-eluting balloons. The distal vessel has increased its size with no signs of the small dissection whatsoever.
Initial antegrade acess was planned given the lesion's favorable characteristics (Japan-chronic total occlusion score of 1). An ultrasound-guided dual angiography was performed with a 7-Fr AL1 guiding catheter (Cordis, United States) via femoral access for the right coronary artery, and a 7.5-Fr PB 3.5 SheathLess guiding catheter (Asahi Intecc, United States) for the left main coronary artery. The procedure was started with a Caravel microcatheter (Asahi Intecc, United States) loaded with a SION wire (Asahi Intecc, United States) that crossed the distal LAD plus a second wire that crossed the D1. The lesion was not heavily calcified, which is why it was predilated with a 2 mm x 12 mm semi-compliant Emerge balloon (Boston Scientific, United States) at 12 atmospheres. Despite using vasodilators, a narrow distal bed in the LAD and D1 was seen, and the use of stenting was ill-advised. Drug-eluting balloon (DEB) angioplasty for the bifurcation was decided. A 2.5 mm x 20 mm SeQuent Please Neo DEB up to a nominal pressure was used for the LAD for 60 seconds (Braun Melsungen, Germany), and a 2 mm x 20 mm DEB up to a nominal pressure was used for the D1 for 60 seconds. A final TIMI grade-3 flow was obtained when the procedure was completed (figure 1B, video 2 of the supplementary data). A small non-flow limiting dissection was managed conservatively in the mid-LAD after the D1.
The patient was scheduled for angiography and optical coherence tomography. Six months later, the study showed patency of recanalization and significant improvement of the distal vessel with a TIMI grade-3 flow (figure 1C). The optical coherence tomography confirmed the excellent results, and the complete resolution of the dissection in the mid-LAD (figure 2A-C, and video 3 of the supplementary data). The patient was free from angina at this follow-up.
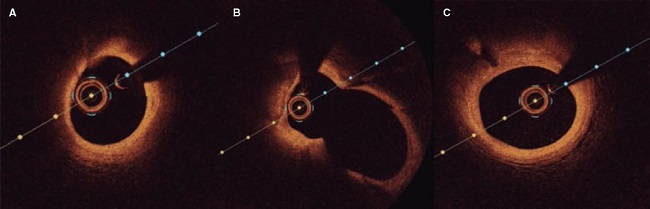
Figure 2 A: distal left anterior descending coronary artery (LAD) showing no signs of the previous dissection. B: LAD at the carina. C: proximal LAD before the bifurcation without any evidence of dissection by optical coherence tomography.
The main reasons to avoid stenting were the size of both vessels, the possibility of side branch occlusion using provisional stenting, and the high probability of in-stent restenosis with a 2-stent technique considering the localization of the lesion. Arguably, good mid-term results were expected if a TIMI grade-3 flow was obtained in both branches, thus avoiding multiple layers of stents. For this reason, we corroborated this hypothesis in a 6-month angiographic and optical coherence tomography follow-up.
The BASKET-SMALL 2 randomized control trial proved to be non-inferior to DEB compared to second-generation drug-eluting stents for a composite endpoint of cardiac death, non-fatal myocardial infarction, and target vessel revascularization in de novo lesions for vessels < 3 mm.1 Even better results were obtained in the randomized control trial PICCOLETO II where a DEB was compared to an everolimus-eluting stent showing less in-lesion late lumen loss at 6 months (0.04 vs 0.17 mm; P = .03).2
Several studies have evaluated different approaches to DEB in bifurcations. However, no randomized control trial has ever compared the use of DEB for the left main coronary artery and side branches to another strategy.3 Observational analyses of 39 and 127 patients conducted by Shulz et al. and Bruch et al., respectively, concluded that a DEB-only approach was safe and effective to treat selected bifurcations (namely a side branch ≥ 2 mm) with low rates of restenosis and target lesion revascularization. Stenting as a bailout strategy was advised when flow-limiting dissection or excessive recoil occurred.4,5
Only a few cases describe the treatment of complex lesions such as a chronic total coronary occlusion with a DEB. Our case seems especially relevant considering that the occlusion involved a bifurcation and a small distal bed. This case highlights the feasibility of treating a bifurcated chronic total coronary occlusion when a narrow vessel is found with a DEB.
REFERENCES
1. Jeger RV, Farah A, Ohlow MA, et al. Drug-coated balloons for small coronary artery disease (BASKET-SMALL 2): an open-label randomised non-inferiority trial. Lancet. 2018;392:849-856. [ Links ]
2. Cortese B, Di Palma G, Guimaraes MG, et al. Drug-Coated Balloon Versus Drug-Eluting Stent for Small Coronary Vessel Disease: PICCOLETO II Randomized Clinical Trial. JACC Cardiovasc Interv. 2020;13:2840-2849. [ Links ]
3. López-Mínguez JR, Navarro Romero R. Current state of knowledge on the use of drug-coated balloon in coronary bifurcation lesions. REC Interv Cardiol. 2023;5:1-4. [ Links ]
4. Bruch L, Zadura M, Waliszewski M, et al. Results From the International Drug Coated Balloon Registry for the Treatment of Bifurcations. Can a Bifurcation Be Treated Without Stents?J Interv Cardiol. 2016;29:348-356. [ Links ]
5. Schulz A, Hauschild T, Kleber FX. Treatment of coronary de novo bifurcation lesions with DCB only strategy. Clin Res Cardiol. 2014;103:451-456. [ Links ]
SUPPLEMENTARY DATA
https://doi.org/10.24875/RECICE.M23000390Supplementary data associated with this article can be found in the online version available at https://doi.org/10.24875/RECICE.M23000390.











 texto en
texto en 


