Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
REC: Interventional Cardiology
versión On-line ISSN 2604-7276versión impresa ISSN 2604-7306
REC Interv Cardiol ES vol.5 no.4 Madrid oct./dic. 2023 Epub 04-Mar-2024
https://dx.doi.org/10.24875/recic.m22000315
Clinical cases
Impella-Clip: a secure and effective strategy in cardiogenic shock due to acute severe mitral regurgitation. Case resolution
Servicio de Cardiología, Hospital Universitario La Paz, Madrid, Spain
CASE RESOLUTION
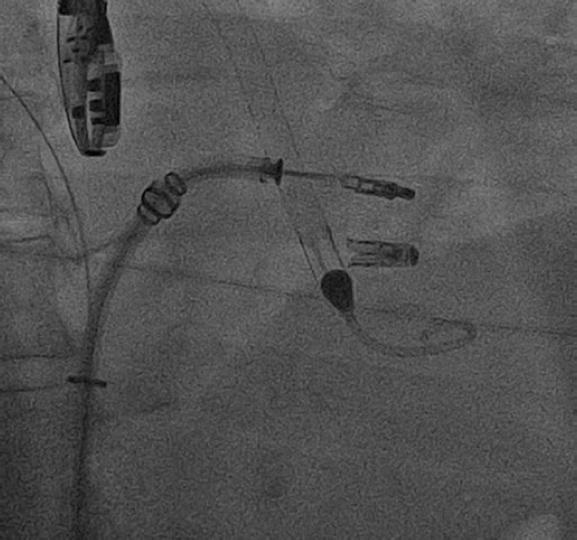
Given the impossibility to remove the Impella 5.0 device (figure 1) and due to the high surgical risk involved (EuroSCORE II, 48,9%; Society of Thoracic Surgeons score (STS), 16%), percutaneous mitral valve repair was attempted with a MitraClip device (Abbott Laboratories, United States).
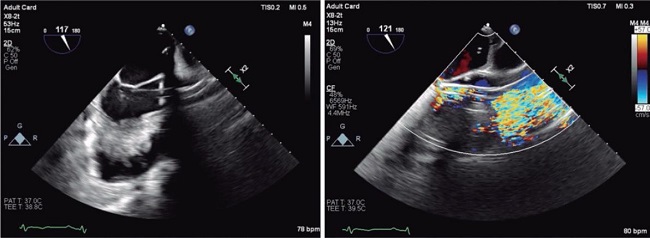
With support from an Impella 5.0 device at a rate of 2 L/min and under transesophageal echocardiography guidance the MitraClip NTW device was implanted at A3-P3 level (greater effective regurgitant orifice area), which resulted in a reduced regurgitant jet (videos 1 and 2 of the supplementary data), improved blood flow into the pulmonary veins, and a transmitral gradient of 4 mmHg. Result was reassessed by reducing hemodynamic support temporarily at 1 L/min. A grade III-IV central regurgitant jet was seen. A second MitraClip NT was implanted at A2-P2 level (videos 3 and 4 of the supplementary data). Difficulties during its positioning due to interference with the Impella 5.0 device were reported, which is why reversal maneuvers towards the atrium were performed. Finally, capture or grasping turned out effective, and the lack of residual mitral regurgitation was confirmed. However, although transmitral gradient increased up to 7 mmHg, after reducing hemodynamic support down to 0.5 L/min, the gradient dropped down to 5 mmHg. Since the presence of hemoglobin levels of 8.6 g/dL and heart rate of 90 bpm could make the gradient could go up slightly -overestimating the measurements- the second device was released with such gradient (figure 2). The patient was extubated and the Impella 5.0 device was removed 72 hours later with satisfactory disease progression.
Acute mitral regurgitation is one mechanical complication of infarction that leads to higher mortality rates (35% to 50%)1 because it is associated with cardiogenic shock (CS) with increased retrograde pressure and volume. Circulatory support and vasoactive drugs necessary here. The Impella device actively unloads the left ventricle, increases cardiac output,1 and is indicated in the acute phase.2
Traditional treatment has consisted of emergency heart valve replacement that is associated with significant perioperative mortality. Over the last few years, percutaneous mitral valve repair has proven beneficial in asymptomatic secondary mitral regurgitation despite optimal medical therapy.2 However, data are scarce on acute mitral regurgitation with secondary cardiogenic shock,1,3 which could be particularly beneficial in this setting.
This case describes how a combined strategy of Impella and MitraClip is both safe and effective. However, several technical considerations should be made at this point: a) the MitraClip device should be positioned carefully due to interference with the Impella device; b) hemodynamic support should be reduced to assess results since this support can overestimate the reduction of mitral regurgitation; and c) anemia and tachycardia are not rare, factors that could overestimate the residual gradient.
Long-term follow-up and more evidence are necessary to support this strategy. However, in the ischemic severe acute mitral regurgitation setting complicated with cardiogenic shock, complete percutaneous resolution (coronary revascularization, Impella and percutaneous mitral valve repair) could be the treatment of choice.
The case was published after obtaining the patient's verbal consent.
REFERENCES
1. Vandenbriele C, Balthazar T, Wilson J, et al. Left Impella-device as bridge from cardiogenic shock with acute, severe mitral regurgitation to MitraClip-procedure: a new option for critically ill patients. Eur Heart J Acute Cardiovasc Care. 2021;10:415-421. [ Links ]
2. McDonagh T, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599-3726. [ Links ]
3. Estévez-Loureiro R, Shuvy M, Taramasso M, et al. Use of MitraClip for mitral valve repair in patients with acute mitral regurgitation following acute myocardial infarction: Effect of cardiogenic shock on outcomes (IREMMI Registry). Catheter Cardiovasc Interv. 2021;97:1259-1267. [ Links ]
SEE RELATED CONTENT:
https://doi.org/10.24875/RECICE.M22000317https://doi.org/10.24875/RECICE.M22000318SUPPLEMENTARY DATA
https://doi.org/10.24875/RECICE.M22000317Supplementary data associated with this article can be found in the online version available at https://doi.org/10.24875/RECICE.M22000317.











 texto en
texto en