INTRODUCTION
The digestive manifestations of systemic lupus erythematosus (SLE) are frequent and very polymorphic. They remain by far dominated by intestinal pseudo-obstructions, peritonitis, ascites, and lupus enteritis [1, 2]. Other rarer complications have been reported: pancreatitis, mesenteric vasculitis, gastrointestinal necrosis and/or perforation, hepatitis, splenic infarction, mesenteric vessel thrombosis, and mesenteric panniculitis [3]. Abdominal symptoms can be the primary presenting signs of lupus disease and thus represent a real diagnostic challenge for clinicians [2, 3, 4].
Acute mesenteric lymphadenitis (AML) remains a rare and unusual manifestation during SLE; forms revealing the disease are exceptional [5, 6].
We report the original observation of isolated AML as the first manifestation of SLE in a 29-year-old woman.
CASE REPORT
A 29-year-old Tunisian woman, without pathological medical history, was explored for acute and febrile abdominal pain evolving for a week and not improved by symptomatic treatment. There have been no reports of associated vomiting or bowel transit disturbances.
The somatic examination noted a fever at 38.5°C and a discrete diffuse abdominal tenderness with peri-umbilical maximum. No peripheral lymphadenopathy, palpable masses, or visceromegalies have been noted.
Biology showed a marked biological inflammatory syndrome with erythrocyte sedimentation rate at 87 mm/H1, C-reactive protein (CRP) at 56 mg/l, and polyclonal hypergammaglobulinemia at 19.3 g/l. The total blood count showed leukopenia at 3400/mm3, neutropenia at 1900/mm3, and lymphopenia at 1140/mm3 with no other abnormalities. The other basic laboratory tests were within normal limits: hemoglobin, platelets, creatinine, blood sugar, serum ionogram, transaminases, muscle enzymes, calcemia, lipid parameters, and urine tests.
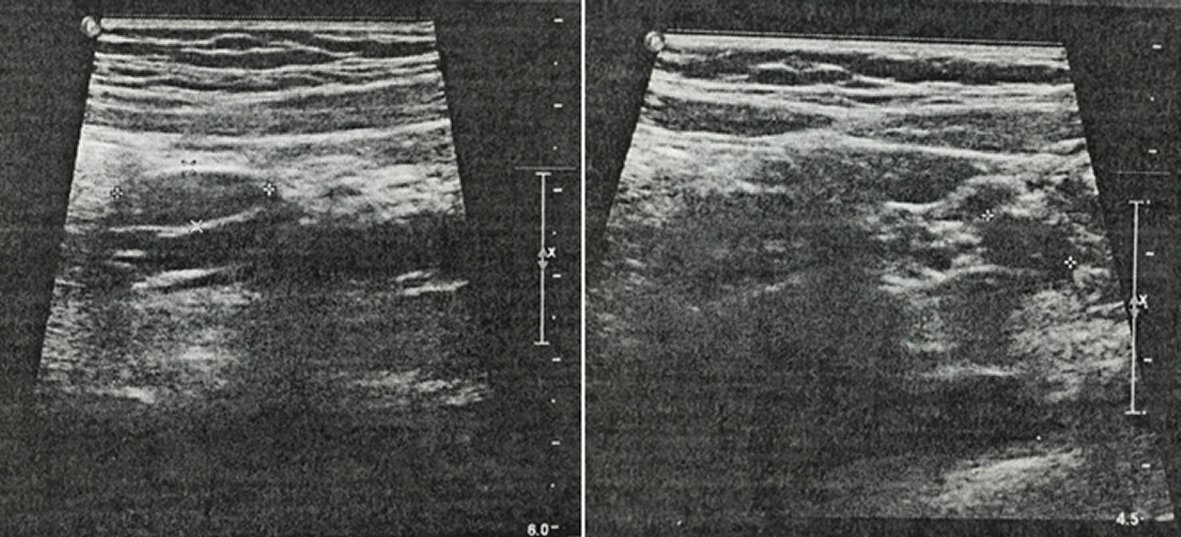
The abdominal ultrasound and computed tomography (CT) objectified multiple large, hypoechoic, and richly vascularized on Doppler mesenteric lymph node compatible with the diagnosis of AML (Figure 1). There has been no evidence of tumor, intraperitoneal effusion, or thrombosis of the mesenteric vessels.
Subsequent investigations made it possible to eliminate an infectious or cancerous cause: blood cultures, urine direct examination and culture, different bacteriological and viral serodiagnostics, tumor markers, chest radiography, thoraco-abdomino-pelvic CT scan, gastroscopy, colonoscopy, transthoracic echocardiography, and tuberculosis tests.
The immunological assessment revealed positive anti-nuclear, anti- double-stranded DNA, and anti-phospholipid antibodies. anti-neutrophil cytoplasmic antibodies (ANCA) and cryoglobulins were negative.
The diagnosis of SLE with revealing acute mesenteric lymphadenitis was retained. Investigations for other specific visceral disorders of SLE (renal, cardiac, and neurological) were negative.
The patient was treated with hydroxychloroquine (400 mg/day), salicylic acid (100 mg/day), and systemic glucocorticoids (0.5 mg/kg/day for four weeks followed by progressive decrease).
The outcome was favorable with disappearance of clinical complaints during the first week, normalization of the hemogram and CRP after two weeks of treatment, and normal abdominal ultrasound at one month of treatment. No recurrence has been noted for two years.
DISCUSSION
Lymph node involvement is far from uncommon during SLE [6-9]. Its prevalence is estimated at 12-59%, and the most common sites are: cervical (43%), mesenteric (21%), axillary (18%), and inguinal (17%). Other sites are more unusual (hilar, mediastinal, and retroperitoneal) [9]. Lymphatic involvement is only exceptionally reported as the primary presenting manifestation of the lupus disease [6, 7, 8, 9].
Acute mesenteric lymphadenitis (AML) remains unusual during lupus, and only a few sporadic observations have been reported [5, 6].
SLE is also an exceptional and unusual etiology of acute mesenteric lymphadenitis; indeed only one case in the series of Macari M et al, of 60 patients with AML had SLE as underlying cause (1.6%) [10].
As in our case, AML may exceptionally be the first manifestation revealing SLE [5, 6]. It therefore represents a real diagnostic and therapeutic challenge for clinicians (specific lupus manifestation or infectious complication?) [11].
The differential diagnosis of lupus AML includes the infectious causes which are particularly frequent in lupus patients (tuberculosis and cryptococcosis) [5, 11], metastatic disease (squamous cell carcinoma and germ cell-tumor) [5], and histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease) which is also frequently associated with SLE [5, 12].
Lupus mesenteric lymphadenitis can be isolated or associated with other lupus manifestations such as: ascites, peritonitis, peritoneal panniculitis, and pancreatitis [5, 12, 13, 14]. It can also be associated with lymphadenopathies in other lymphatic sites [6]. It can even precede the diagnosis of lupus disease by several years [13].
SLE-specific mesenteric lymphadenitis usually has a good prognosis and responds quickly to systemic corticosteroid therapy [5].
CONCLUSION
As exceptional and unusual as it is, this abdominal manifestation of SLE deserves to be known by healthcare professionals to avoid diagnostic and therapeutic delays. Our observation is distinguished by its isolated and inaugural character.
It thus seems useful to screen for SLE in front of any AML that does not prove itself, in particular in young women.