INTRODUCTION
Dentin hypersensitivity (DH) is characterized by exaggerated, short-term, intense variable-intensity pain that occurs in reaction to every thermal, chemical, tactile or osmotic stimulus [1]. Multiple etiological factors such as inappropriate teeth brushing, premature occlusal touch, gingival recession, and the presence of large quantities of exogenous and endogenous acids in diets can result in DH [2].
DH is caused by the displacement of the fluid inside the dental tubules [2]. There is a range of therapeutic strategies available for the control of dental hypersensitivity. Various chemical or physical agents are used either to mask uncovered dental tubules or to desensitize the nerve. The typical method of treatment is the placement of a topical agent at frequent intervals. This could be done either by a patient at home or by a dental professional. Another method of sealing the dentinal tubules may include the application of restorations or dental adhesives [3]. Fluoride varnishes have been put to the market to improve the quality and longevity of fluoride release at the site. The mechanism of action is the accumulation of calcium fluoride on the tooth surface and the development of fluorapatite [4].
Aaron S Posner was the first to describe Amorphous Calcium Phosphate (ACP) [5]. Casein Phosphopeptide Amorphous Calcium Phosphate (CPP-ACP) was used as a more advanced material for the treatment of DH. It inhibits enamel demineralization and improves enamel remineralization [6]. The purpose of this research was to determine the effectiveness of CPP-ACP-based varnish relative to sodium fluoride varnish in the reduction of dentin hypersensitivity.
MATERIALS AND METHODS
For this randomized, double-blind and split-mouth clinical trial, 40 systemically healthy subjects between the ages of 20 and 55 years were selected for the trial. Subjects with Visual Analog Scale (VAS) score ≥ 3 after scaling and root planning; were included in the research. Subjects with carious lesions on the selected or neighbouring teeth, extensive restorations as well as defective restorations, abutment teeth for removable or fixed prostheses, cracked teeth and chipped teeth, substance abuse and pregnant females were excluded from the study. Besides, subjects prescribed with the desensitization process or analgesics/anti-inflammatory drugs were excluded from the study. Teeth with gingival recession, attrition, abrasions, abfractions and erosion were not excluded.
After scaling and root planning, 40 subjects were selected for the trial, and divided into two groups:
Group A (Test group): 20 DH subjects treated with MI Varnish® (GC India Private Limited) and
Group B (Control group): 20 DH subjects treated with Fluoritop SR® varnish (ICPA Company).
After obtaining written informed consent, the subjects were assessed for baseline DH scores using VAS. The hypersensitivity level was calculated using VAS. The VAS is a calculating tool with subjective traits or behaviours that cannot be specifically calculated for eg. Pain. Respondents show, when referring to the VAS object, their degree of agreement with the assertion of the sensitivity of damaged teeth in this case by suggesting a place between 0 and 10 on a 10 cm line where 0 is not pain and 10 is the worst possible pain [7].
After adequately drying the experimental site, isolation with the cotton pellet was done. The isolation helped prevent oral fluid contamination during the process. Using applicator tip, varnish application at the experimental site was performed and allowed to dry for at least 5 minutes. The subjects were refrained from taking any fluids, beverages and sticky foods for at least 2 hours after the application. After 2 hours, they were instructed to gently brush their teeth. Brushing is facilitated in the removal of any dried or extra varnish around the tooth. The recall was scheduled on the 14th day for follow up and recording of VAS Scores. The data obtained were subjected to statistical analysis using students‘t’test.
RESULTS
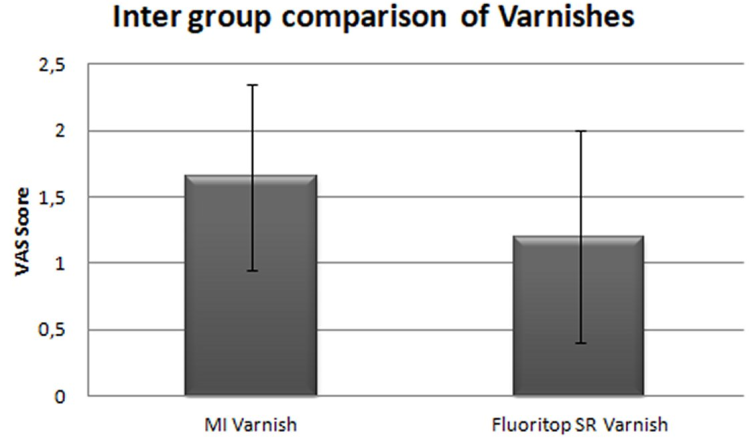
A total of 40 subjects were equally divided (n=20) into two groups for this clinical trial. VAS scores were recorded at baseline and day 14 for both the group. On the Intragroup comparison of the varnishes, a significant statistical difference (p < 0.05) was observed. Baseline VAS score for Group 1 (Figure 1) was recorded as 5.55 ± 1.61 which was reduced to 1.65 ± 0.88 on Day 14 evaluation. Similarly, Group 2 (Figure 2) showed a reduction from 4.6 ± 1.35 to 0.2 ± 1.01. Intergroup comparison showed no statistical significance (p = 0.139) among the groups (Figure 3). The result of the intergroup comparison stated that both groups were efficacious in the reduction of DH and either of them can be used for effective clinical outcome.
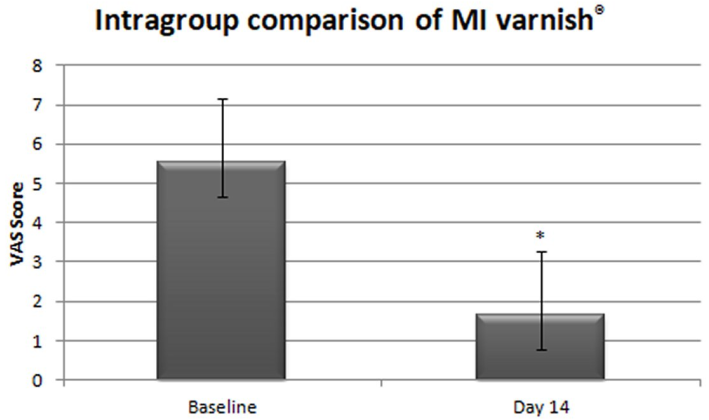
Figure 1. Intragroup comparison at baseline and at 14th day (MI varnish®).VAS Score is expressed as mean±SD. *p < 0.05.
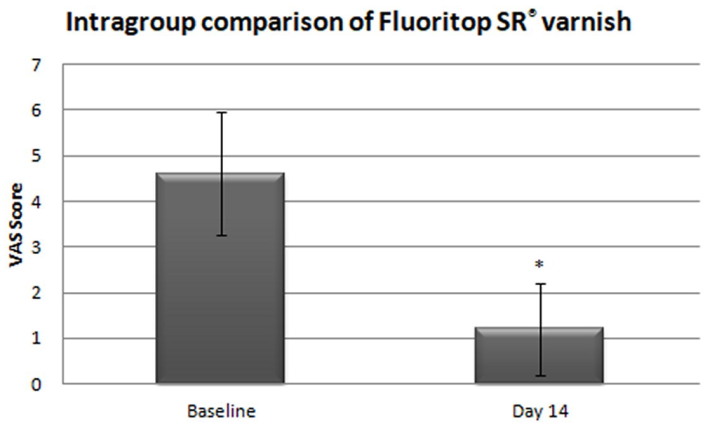
Figure 2. Intragroup comparison at baseline and at 14th day (Fluoritrop SR®).VAS Score is expressed as mean±SD. *p < 0.05.
DISCUSSION
Dental hypersensitivity is the most common challenge that dentists experience in their everyday lives. As a consequence, handling it becomes more critical as there is a lack of enamel and cement during periodontal treatment. Two steps were suggested for dental hypersensitivity pathogenesis, one for initiation of the lesion and the other for localization of the lesion [8]. The initiation of the lesion happens following the elimination of the smear sheet. This arises during the scaling and root planning procedure leading to the opening and exposing of the dental tubules and resulting in the localization of the lesion and DH [9]. The lack of security over dentin in cases where lack of enamel is seen results in abrasion, attrition, erosion, and gingival recession [9].
Various available options are used for the treatment of DH. In the current study, Fluoritop SR®, a sodium fluoride-based varnish has been used as a control group. Studies have shown positive results in reducing DH. In a double-blind, split-mouth clinical study of 8-week, the relief in hypersensitivity occurred shortly after the first application. It also remained persisted during the 8-week follow-up [10]. Slow and continuous fluoride release acts by preventing lesion initiation.
Reddy et al [11] conducted a study on 160 subjects dividing them into different groups: a) a toothpaste containing 5% fluoro calcium sodium phosphosilicate with fused silica (Biomin®); b) a toothpaste containing 5% CSPS (NovaMin®); c) herbal formulation; d) toothpaste containing 5% potassium nitrate. The patient’s DH scores for tactile, evaporative stimuli were recorded on a visual analog scale at baseline, 2 weeks, and at the end of 4 weeks. All the four desensitizing toothpastes containing different active agents were effective in relieving DH. However, the Biomin® group showed a better clinical response at the end of 4 weeks when compared with others.
Aghanashini et al. [12] conducted a randomized clinical trial using diode laser and fluoride varnish for the treatment of DH. DH was evaluated using tactile stimulus and air blast at baseline, 15 days, 30 days and 60 days. They concluded that both diode laser and fluoride varnish were effective in treatment of DH. However laser showed superior results over a period of 60 days.
Nardi et al. [13] conducted a study foe evaluating and comparing the effectiveness of two different desensitizing varnishes. Ninety healthy adults suffering from tooth sensitivity were divided into three groups. Two different varnishes were used for the study: Fluor Protector S®, containing 7700 ppm fluoride (group I), and Cervitec F®, containing 1400 ppm fluoride and 0.3% chlorhexidine (group II). A placebo containing water and ethanol was applied for the third group. Tooth sensitivity was measured using the Schiff’ scale at baseline and after 30 and 90 days. Group I and group II showed statistically significant results they concluded that desensitizing varnishes are a valid treatment for tooth hypersensitivity.
Owoturo et al. [14] conducted a subject‑blind randomized clinical study to determine the clinical outcomes of two different varnishes in the management of DH. The subjects were randomly assigned into Duraphat® or Cervitec Plus® varnish groups in a split‑mouth study design. The teeth were assessed for sensitivity, and this procedure was repeated on week(s) 1, 2, and 4 following the initial visit. There was a significant reduction in sensitivity following application of both control and experimental varnishes. However, there was no statistically significant difference in the efficacy of the control and experimental varnishes. They concluded that Duraphat® exhibited better efficacy in the reduction of dentinal hypersensitivity, though the difference was not statistically significant. The Duraphat® and Cervitec Plus® varnishes can be substituted one for the other.
Patil et al. [15] conducted an in vitro study to assess and compare the efficacy of iontophoresis with 0.33% Sodium Fluoride (NaF) gel and diode laser alone in dentinal tubule occlusion. They concluded that Diode laser application provided better results as compared to iontophoresis on occlusion of dentinal tubules. Hence, it can be used to treat the patients with DH.
The experimental group consisted of MI varnish®, a CPP-ACP based varnish. This Varnish can localize ACP at the tooth structure. This increases the level of calcium phosphate in plaque and acts as a calcium phosphate reservoir. Also, it maintains supersaturation on tooth enamel by buffering the free calcium and phosphate ion activities. These ion activities potentially convert to stable crystalline phases, like as octacalcium phosphate or apatitic products [6]. Hence, it acts to prevent lesion localization.
In one of the clinical trials, DH induced by post scaling procedure was managed by using milk as a desensitizing agent [16]. Another trial, conducted by Sabir et al. [10], stated that casein in milk helped in the remineralization process of early enamel lesion. The above-mentioned studies utilized milk in the form of mouth rinse for management of DH. However, patient compliance is not fair in such cases. MI varnish®, with a direct application on the tooth, increases both surface area and time of contact on initial enamel lesion. This could be the reason for the potential results observed in the current study.
Lata et al. [17] conducted an in vitro study using cream-based CPP-ACP. The cream-based formulation was effective in remineralization, but to a lesser extent than fluoride in remineralizing. ACP has been proven to have remineralization potential in early enamel lesions [17]. In an ex-vivo SEM study, significant remineralization of the early enamel lesions was observed [18]. CPP-ACP, a constituent of milk, has the property of substantivity and longer duration of action [7]. Casein phosphopeptide based cream has been used earlier in an in-vitro study [18]. The present in-vivo study is the first of its kind which uses the varnish for the management of DH. The results obtained from the previous studies [16, 17, 18] are in accordance with the present study.
CONCLUSIONS
Within the limitations of this study, it can be concluded that MI varnish® and Fluoritop SR® varnish are equally efficacious in treating dentinal hypersensitivity. Furthermore, more randomized controlled clinical trials with larger sample size and longer follow-up are required to check the efficacy of MI varnish®.