INTRODUCTION
Thyroid carcinomas which are derived from follicular epithelial cells namely, papillary, follicular and Hurthle cell types are generally categorized as well differentiated thyroid cancers and constitute the majority of thyroid malignancies [1, 2, 3, 4, 5, 6, 7, 8]. Anaplastic carcinoma falls under the category of undifferentiated thyroid malignancy [1, 2, 3, 4, 5, 6]. Patients are classified by using well-established prognostic parameters and therapy follows a variety of published and regularly renewed guidelines. Treatment of thyroid cancer employs a three-tiered approach comprising surgery, iodine radiometabolic treatment and long-term thyroid-stimulating hormone suppression by exogenous administration of thyroid hormone [9, 10, 11].
DEFINITION OF TERMS
Occult thyroid carcinoma
The term “Occult Thyroid Carcinoma” is highly controversial and could depict several meanings in different clinical scenarios from the literature. The Merriam-Webster dictionary, in the current on-line version, explains “Occult carcinoma” as “not manifest or detectable by clinical methods alone”, and as “not present in macroscopic amounts” [9, 12]. The McGraw-Hill Concise Dictionary of Modern Medicine (2002) defines “occult primary malignancy” as “unknown primary malignancy that is symptomless, which first manifests itself as metastases or secondary paraneoplastic phenomena” [13]. In 1997, Moosa and Mazzaferri defined “Occult thyroid carcinoma” as an “impalpable thyroid carcinoma that is generally smaller than 1.0 cm” [9, 14]. A more precise definition of size is used by Stedman's Medical Dictionary (2006), where “occult papillary carcinoma of the thyroid” is described as micro-carcinoma of the thyroid or microscopic papillary carcinoma of the thyroid, usually well encapsulated and measuring less than 5 mm in diameter [9, 15]. A combination is used in the World Health Organization (WHO) classification system, where papillary thyroid microcarcinoma (PTMC) is defined as “papillary carcinoma measuring 1.0 cm or less in maximal diameter while other clinico-pathological features, such as metastasis to regional lymph nodes and/ or distant organs as well as extra-thyroid extension, are not considered” [9, 16]. Shaha uses a broader definition of PTMC: “Traditionally, microcarcinoma was considered to be less than 1 or 1.5 cm” [9, 17]. Therefore, from the preceding, the terms occult thyroid carcinoma and papillary microcarcinoma could be synonymous in most clinical situations.
Thyroid incidentaloma
“A thyroid incidentaloma is an unexpected, asymptomatic thyroid tumor incidentally found during the investigation of an unrelated condition” [18]. Interestingly, another study submitted that a thyroid nodule discovered during imaging study performed due to unrelated thyroid disease is known as a thyroid incidentaloma [18].
“PAIN” phenomenon
This term is referred to as Positron Emission Tomography Associated Incidental Neoplasm of the thyroid gland, which represents asymptomatic thyroid tumor fortuitously discovered on Positron Emission Tomography (PET) scan during the investigation of an unrelated condition [19].
CLASSIFICATION OF OCCULT THYROID CARCINOMA
Furthermore, the term “occult thyroid carcinoma” can be divided into four different categories.
Category One: The first group comprises of patients with thyroid carcinoma or microcarcinoma incidentally found in the thyroid gland after total thyroidectomy for benign disease [9, 17, 20, 21, 22] or at autopsy [9, 23, 24, 25, 26, 27, 28, 29, 30].
Category Two: In the second group there are patients with incidentally detected PTMC on imaging studies, mainly ultrasonography, and evaluated by fine needle aspiration biopsy (FNAB) [9, 23, 24, 25, 26, 27, 28, 29, 30].
Category Three: The third group consists of patients with clinically apparent metastases of thyroid carcinoma, where the primary tumour is not detectable before surgery and microscopic tumour – microcarcinoma is found in the final histological specimen [9, 23, 24, 25, 26, 27, 28, 29, 30].
Category Four: The fourth group covers patients with thyroid cancer localized in ectopic thyroid tissue with clinical symptoms or with apparent metastases [9, 23, 24, 25, 26, 27, 28, 29, 30].
BURDEN OF THE DISEASE
Thyroid carcinoma is rare, with a global incidence of only 1–2% of the population. It constituted approximately 12.5% of all thyroid disorders in Southwestern Nigeria [31, 32, 33]. The survival rate from thyroid cancer is extremely high in the United States of America [34], while the treatment outcome is usually relatively poor in a low-resource setting. This finding of poor outcome in our setting might be because of the late presentation of patients with goitre, due to poverty and ignorance [35], in addition to the limited facilities for managing patients.
We adopt “occult thyroid carcinoma” because our study is aimed at detecting the proportion of those in this cohort of patients, who were diagnosed with thyroid carcinoma or microcarcinoma incidentally after total thyroidectomy for benign disease [9, 17, 20, 21, 22]. The poor management outcome might be worsened by a high proportion of occult thyroid carcinoma found following thyroidectomy for seemingly benign goiter [9, 20, 21, 22].
Occult thyroid carcinoma was 37% of the thyroid gland diseases managed in our centre about four decades ago [31]. It is still common globally despite the improvement in preoperative diagnostic facilities [36], constituting 8.9% of multinodular goitres in a study [37] and 9.2% in a recent review of fine needle aspiration cytology of thyroid masses in our centre [38].
OBJECTIVE OF THE STUDY
The proportion of patients in which a diagnosis of occult thyroid carcinoma was made following post-operative histopathological study in our practice is unknown. Therefore, this study was conducted to evaluate that proportion and highlight the outcome of managing the patients with occult thyroid carcinoma in our low-resource practice.
MATERIALS AND METHODS
A retrospective review of the records of patients managed for thyroid carcinoma in our centre over the 15 years between 1995 and 2009 was conducted. The data retrieved from the record include the biodata, clinical features, clinical and histopathological diagnoses, and the extent of thyroidectomy performed on the patients. The study population includes 62 patients who were managed with a histological diagnosis of thyroid carcinoma during the period and whose records were complete. The data analysis was done using descriptive statistics. We also identified the challenges that might have hindered the management of the patients with such post-operatively diagnosed thyroid cancer.
RESULTS
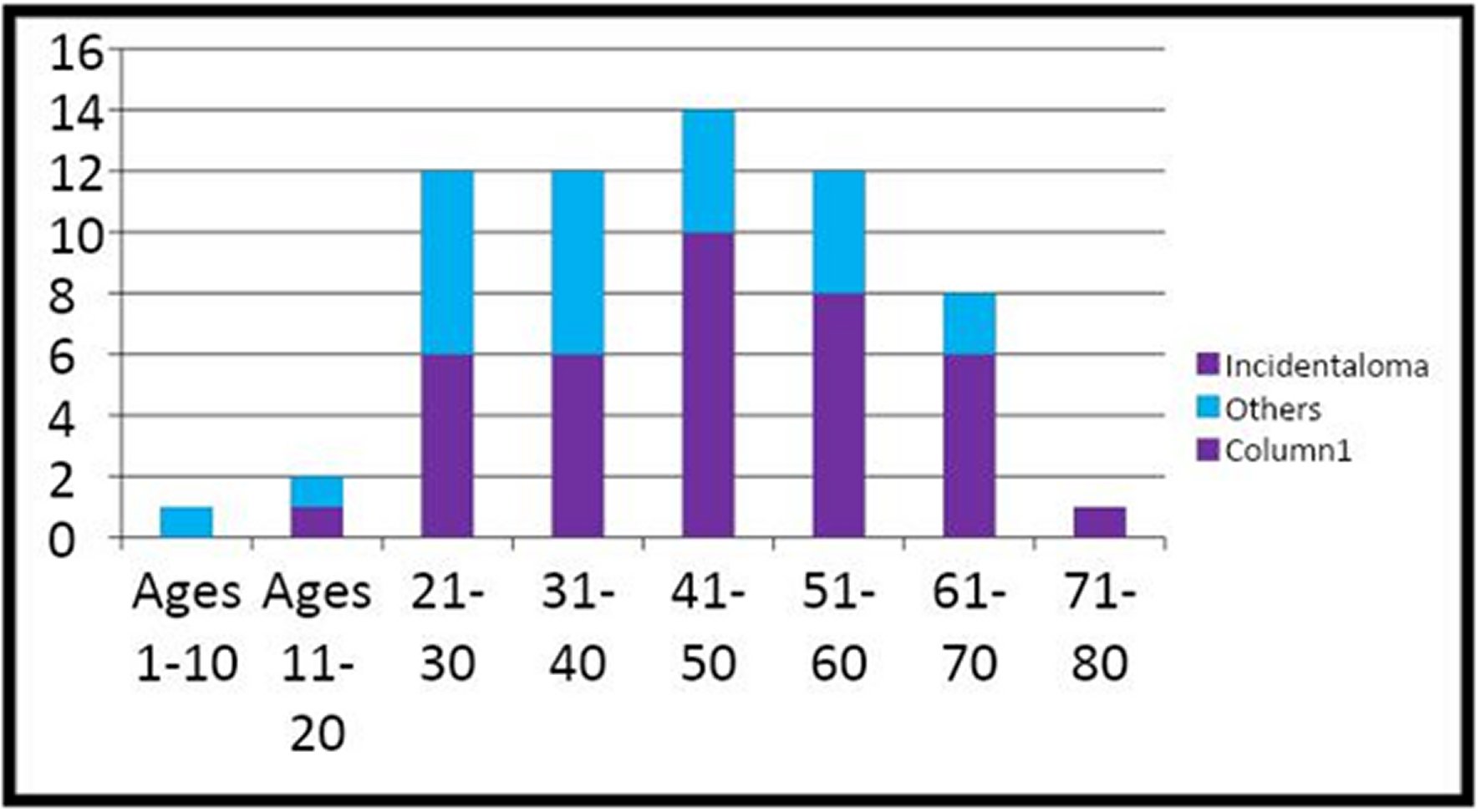
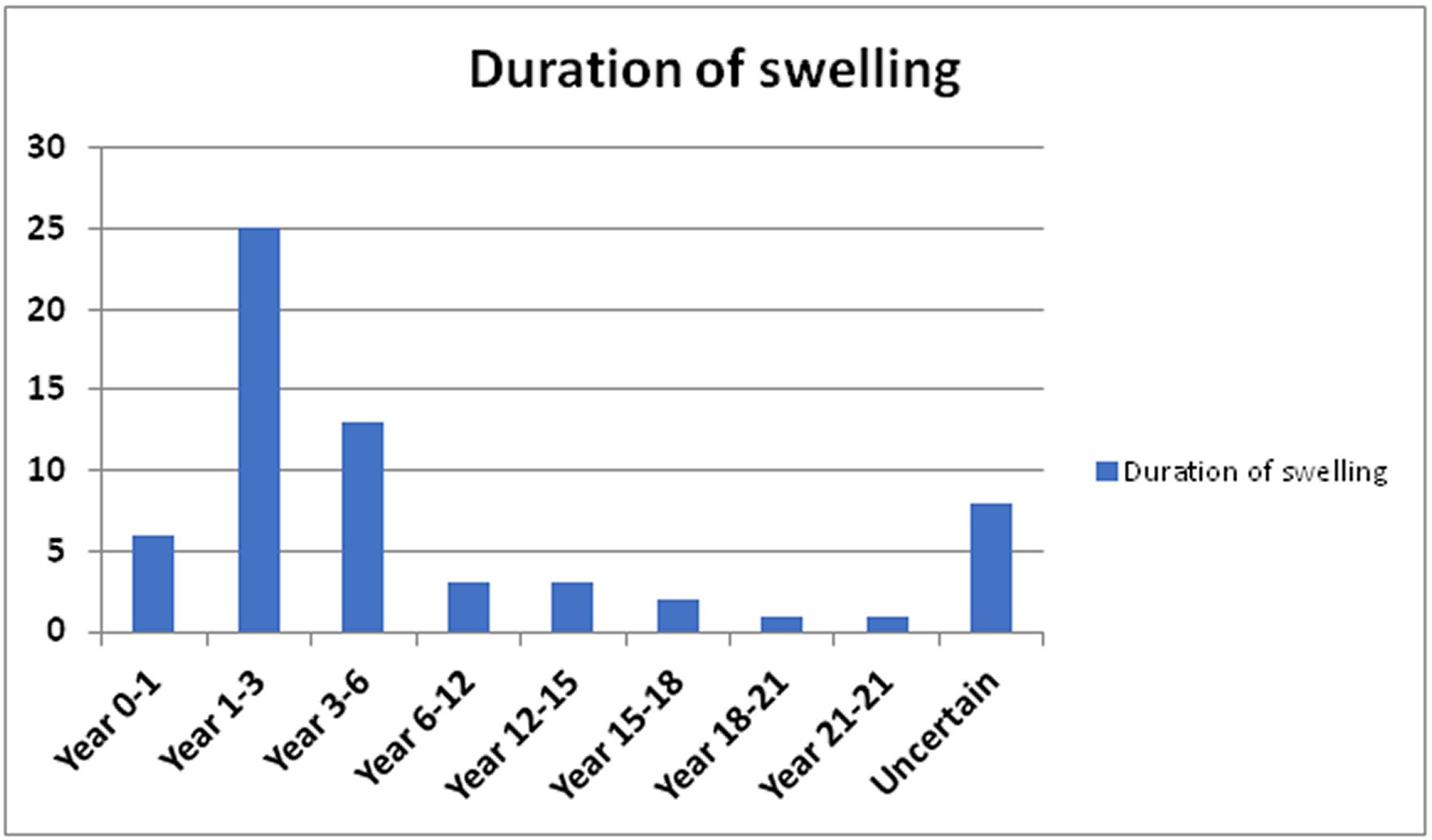
Sixty-two patients met the inclusion criteria and had an age range between 7 and 74 years, with a median interquartile range of 45 years. The age distribution of the patients is shown in Figure 1. The male-to-female ratio of the patients was 1:4. There were 354 cases of thyroid patients operated during the study period, and their clinical features include anterior neck swelling, dysphonia, dyspnoea, dysphagia, weight loss, pain, cervical masses, and bony swelling. The duration of neck swelling in patients who presented with thyroid cancer in the study is shown in Figure 2. The surgeries performed on the patients were total thyroidectomy, 48 (77.4%), completion-thyroidectomy, 14 (22.6%), near total thyroidectomy, eight (12.9%), and, subtotal thyroidectomy, four (6.5%). Thirty-eight (61.3%) of the patients were diagnosed incidentally after the reports of the histology of the thyroidectomy specimens were available. The histological types of carcinoma in the 62 patients are papillary, 34 (54.8%), follicular, 25 (40.3%), medullary, 2 (3.2%), and anaplastic, 1 (1.6%). The complications of management are respiratory obstruction, dysphonia, secondary haemorrhage, seroma, surgical site infection, wound dehiscence, hypertrophic scar, keloid, and death. Two of the patients who presented late with non-resectable tumours received palliative care, while two other patients died from the disease's progression (Figure 3). The limitations confronting effective care of patients identified in this series include late presentation, inadequate oncologic surgery, financial constraint, low utilization of radioiodine facility, and non-resectability of the recurrent or residual tumours.
DISCUSSION
The prevalence of incidental thyroid carcinoma in the United States, from general autopsy studies, is approximately 3.6% [39]. However, this disease entity's clinical significance is likely to vary globally according to the available resources for the management of patients. Patients with Graves' disease have a 2.2% prevalence of occult thyroid carcinoma, which did not differ significantly from most patients with nontoxic or toxic nodular goiter [40]. While the carcinomas in those patients were papillary microcarcinomas of no clinical consequence, the diagnosis of more giant coincidental tumors in apparently benign goitres might contribute to management challenges in a low resource setting if it constitutes a high proportion of patients with thyroid cancer. The choice of occult thyroid carcinoma as opposed to “incidental thyroid carcinoma” in this study is based on the clear distinction between them as well defined and presented in the preceding section [18, 19].
The clinical features in those patients whose diagnoses of thyroid cancer were apparent even before ancillary investigations were performed invariably demonstrated late presentation. These features include bone masses, ulcerating and bleeding thyroid masses as illustrated in Figure 3; others are cervical lymphadenopathy, and pathological fractures, etc. However, some clinical features like a goitre, dysphonia, dysphagia, and paresis of a vocal cord may not be specific for thyroid cancer because our patients usually present late with large goiters, with pressure on the contiguous structures [35]. The large goitres in the patients who presented late initially and the locally advanced recurrent or residual disease account for the complications like airway obstruction and seroma. The mortality of only two patients at the time of this review is attributed to the retrospective nature of the study with some of the patients lost to follow-up at our centre.
Generally, in most countries in Africa comprehensive diagnostic facilities for thyroid disorders are lacking. The commonly operational diagnostic techniques include immunoassays, serology, ultrasonography, cytology, and histopathological techniques for the evaluation of thyroid nodules. Computer tomographic scans and magnetic resonance imaging facilities are also not readily available [1]. Even where these facilities are available, the patients are unable to access the diagnostic facilities practically because of the health care payment system otherwise referred to as “out of pocket payment [1].
In this series, occult thyroid carcinoma constituted 61.3% of the patients managed for thyroid cancer. This contrasts with the previous study which found thyroid carcinoma in 37% of patients managed for thyroid disorders generally. The current value is the proportion of occult thyroid carcinoma in the patients who were managed for thyroid cancer. The value may be attributed to the low sensitivity and specificity of the patient's clinical features. The value may be improved upon by use of the ancillary investigations compared to the past. The preoperative diagnosis of thyroid cancer was not made adequately made with the limited facilities available like Fine Needle Aspiration Cytology (FNAC) because of its limitations. Radionuclide thyroid scanning facility, which is not readily available in a low-resource setting, became available in our hospital in the latter period of this study. However, it was not used routinely in patients' preoperative evaluation due to the additional financial burden on them. Besides, its role in the routine preoperative evaluation of patients with thyroid nodules is doubtful because ultrasound guided FNAC of goitre was more cost-effective for tissue diagnosis. Our center's thyroid FNAC audit showed a sensitivity of only 35%, with accuracy for detecting thyroid malignancy of 89% [36]. The high proportion of occult thyroid cancer may be reduced using ultrasound guided FNAC of thyroid gland, which was instituted after the audit.
The proportion of occult thyroid cancer in this study is similar, but less than the incidence in another survey from Southwestern Nigeria where occult malignancy occurred in 69% of thyroid malignancy [41]. While follicular carcinoma was the most common histology subtype in that series, the papillary subtype is the most common in this study and another from Southern Nigeria [42]. However, the relatively lower 54.8% prevalence of papillary carcinoma in this series of patients compared with the 85% [43] in an iodine-replete environment like the US may negatively impact the prognosis. Papillary microcarcinoma was not diagnosed in any of the patients in this study. This missed diagnosis may be due to late presentation of the patients with bigger and multiple nodules. The prognosis of the patients might have been better overall if this histological subtype were predominant. As a result, the overall prognosis of occult papillary microcarcinoma is so good that it was suggested that no further treatment like completion-thyroidectomy or lymph node dissection might be necessary immediately after its diagnosis [36].
Total thyroidectomy was the most performed surgery in this series of patients, followed by completion- thyroidectomy. The performance of total thyroidectomy for apparently benign goitres was introduced around the beginning of the period under review. The apparent rise in the incidentally diagnosed thyroid cancer was one indicator for the shift from partial to total thyroidectomy for benign thyroid lesions. This shift reduced the challenge of performing completion-thyroidectomy for the patients with post-operatively diagnosed thyroid carcinoma. Completion-thyroidectomy was 22.4% of the surgeries performed because of the need for adequate adjuvant management of those patients who had a partial thyroidectomy. Most of this group of patients had primary surgery elsewhere and either presented on their own or was referred for radioiodine therapy.
Interestingly, like lobectomy and subtotal thyroidectomy, partial thyroidectomy is still the most performed surgery in many centres for patients who have thyroid enlargement. The reasons for this preference include the burden of replacement l-thyroxine and the belief that the complication rate of partial thyroidectomy is lower than that of total thyroidectomy. However, there is evidence that the complication rates of partial thyroidectomy and total thyroidectomy in centres where large-volume surgery is performed are similar [44, 45]. The challenges of completion-thyroidectomy include the technical difficulties that may attend it as most of the patients presented late with recurrent or residual tumours. The complications following total thyroidectomy were like those of conservative procedures, while second surgical procedures for recurrent goitre and incidental thyroid carcinoma have a higher risk of complications in a study. The authors, therefore, recommended total thyroidectomy as a standard procedure for benign thyroid pathologies [46]. This act of performing total thyroidectomy will minimize the challenges that attend performing a completion-thyroidectomy. The challenge of inadequate surgery, even if the patient agreed to total thyroidectomy, can be overcome by acquiring the necessary skills to perform the procedure with reduced complications. This scenario would have reduced the challenge of managing the patients who presented late with non-resectable tumours and received palliative care; and the two other patients who died from the disease's progression.
The role of effective national health insurance scheme as an antidote to out-of-pocket healthcare expenses cannot be over-emphasized, which could invariably proffer solution to the high cost of healthcare, accessibility, and affordability in our low resource settings [47, 48, 49]. Besides, the cost of treatment, which is usually met through out-of-pocket expenditure, is a challenge to patient management. Two patients could not afford the cost of completion-thyroidectomy following the diagnosis of incidental thyroid cancer after the initial partial thyroidectomy. The burden of daily replacement or suppressive l-thyroxine therapy for life, including cost, was the reason for not giving consent for total thyroidectomy initially by the patients. Some patients' decision not to give consent for total thyroidectomy was reinforced by the low sensitivity of FNAC for the preoperative diagnosis of thyroid cancer. Radioactive iodine ablative therapy for thyroid cancer has been well discussed in the literature [50, 51]. However, our patients in this series were not treated with radioactive iodine therapy due to high cost and non-availability in our facility during the study period. Surprisingly, for the reasons of the high proportion of occult thyroid carcinoma in patients with thyroid cancer and recurrent benign goitres in our practice, we decided to be offering total thyroidectomy for most patients.
LIMITATIONS OF THE STUDY
Retrospective nature of the study with possible could be marred by poor record keeping due to incomplete data in less than 10% of the total patients managed.
Lack of Electronic Medical Record System in the hospital till date with resultant loss of data.
The clinical course of the disease is mostly altered by delay in patients' presentation, as observed in this series.
Poverty, ignorance, false beliefs, and insufficient health infrastructure, in the sub-region of Nigeria are amongst the lists of possible limitations of this study.
PANEL KEY MESSAGES
The burden of late presentation of patients to the clinicians is enormous in our thyroid clinic.
In most part of Africa, comprehensive diagnostic facilities for thyroid disorders are lacking.
The low sensitivity of FNAC that could impact negatively on its accuracy.
The cost-effectiveness of preoperative diagnostic radionuclide scanning remains doubtful, and this might impact significantly on the outcome of healthcare in our low resource setting.
Total thyroidectomy was the most performed surgery in this series of patients, followed by completion- thyroidectomy.
The performance of total thyroidectomy for apparently benign goitres was introduced around the beginning of the period under review.
The apparent rise in the incidentally diagnosed thyroid cancer was one indicator for the shift from partial to total thyroidectomy for benign thyroid lesions. This shift reduced the challenge of performing completion-thyroidectomy for the patients with post-operatively diagnosed thyroid carcinoma.
Surprisingly, for the reasons of the high proportion of occult thyroid carcinoma in patients with thyroid cancer and recurrent benign goitres in our practice, we decided to be offering total thyroidectomy for most patients.
The overall financial burden of healthcare due to out-of-pocket payment in most contemporary African settings.
There is inadequate use of total thyroidectomy due its technicality in our practice settings.
The utilization of life- thyroxin replacement therapy contributes directly or indirectly to a huge financial burden for these patients.
The absence of the papillary microcarcinoma histology subtype may also impact negatively on the overall outcome of care.
RECOMMENDATIONS
Clinicians globally need to be conversant with the clinical entity known as “occult thyroid carcinoma” which is gradually increasing in our practice.
There is a strong need for public health campaign to encourage early presentation for our patient.
For clinician globally, a high level of clinical suspicion and aggressive work-up and treatment are usually rewarding.
As a matter of urgency, there is therefore a need to formulate a guideline to help clinicians make the right decision when treating patients with occult thyroid cancer.
The role of effective national health insurance scheme as a solution to out-of-pocket healthcare expenses cannot be over-emphasized. This could invariably proffer solution to the high cost of healthcare, accessibility, and affordability in our low resource settings.
Concerted effort should be geared towards improving the diagnostic accuracy of FNAC, and availability of high yield preoperative tools like CT and PET scan, for thyroid disorders.
We, therefore, recommended total thyroidectomy as a standard procedure for benign thyroid pathologies. This act of performing total thyroidectomy will minimize the challenges that attend performing a completion-thyroidectomy.
The challenge of inadequate surgery, even if the patient agreed to total thyroidectomy, can be overcome by acquiring the necessary skills to perform the procedure with reduced complications.
The need for completion-thyroidectomy and the reduced utilization of radioiodine therapy in non-resectable or inoperable recurrent or residual tumour, arising from inadequate surgery, can equally be challenging to the surgeons and patients alike.
CONCLUSIONS
In this series, the audit of occult thyroid cancer cases demonstrates that those large goitres could be sanctuary sites for carcinoma or even micro-carcinoma. Therefore, there a need for an aggressive public health campaign to encourage early presentation for our patient. For clinician globally, a high index of clinical suspicion and aggressive work-up and treatment are usually rewarding. As a matter of urgency, there is therefore a need to formulate a guideline to help clinicians make the right decision when treating patients with occult thyroid cancer.
Concerted effort should be geared towards 1) improving the diagnostic accuracy of FNAC, 2) better healthcare financing system through insurance, 3) availability of high yield preoperative tools like CT and PET scan, and 4) improvement in skills for adequate oncologic surgery, or appropriate referral to centres where such expertise is available in the short term.