INTRODUCTION
The relationship between inflammation and cancer has been an interest of researchers for over 100 years [1]. The inflammation process plays a key role in the initiation and progression of malignant processes that are activated by cytokines and other immune system mediators [2]. Serum cellular biomarkers like the neutrophil-lymphocyte ratio (NLR), the plateletlymphocyte ratio (PLR) and the lymphocyte-monocyte ratio (LMR) provide indications of the systemic immunological response to tumour cells [3]. Several studies have highlighted the prognostic value of these biomarkers for certain types of cancer [3], and the ability of NLR and PLR to predict tumour malignancy has recently gained the attention of researchers [4].
Platelets contribute to inflammation through their interaction with myeloid cells and nonimmune cells [5]. Platelets also contribute to anti-inflammatory effects by inhibiting the release of tumour necrosis factor from mononuclear cells such as monocytes and macrophages and by promoting the release of anti-inflammatory cytokines [6]. Recent studies have suggested that platelets contribute to the development and spread of cancer [7].
Platelet mass has been shown to be a more effective indicator of platelet activity than platelet count; therefore, the platelet mass index (PMI), also known as plateletcrit, has been increasingly used as a diagnostic parameter [8].
Testicular tumours are rare cancers that comprise only one percent of male malignancies [8]. Although uncommon, screening is important because testicular cancer targets younger men, typically from 15 to 40 years of age, and it has a high cure rate even if the tumour has spread [9]. This high cure rate may be due to the relationship between testicular tumours and immunity [10]. Recent reports linking immunocompetence and testicular cancer patients are still unsubstantiated [11].
Previous studies have investigated the role of NLR in urogenital cancer diagnosis; however, although there are very limited reports on the diagnostic value of PMI in the literature, no studies on testicular malignancies have been reported. In our study, preoperative PMI values of testicular cancer patients were compared with a control group of varicocele patients. The discriminatory role of PMI in patients with testicular masses was investigated.
MATERIALS AND METHODS
In this retrospective study, the data of 76 male patients between January 2007 and January 2017 (38 subjects with localized testicular cancer and a control group of 38 subjects with varicocele) were analysed after the study was approved by the institutional review board committee. The following parameters were analysed and subjected to statistical analysis: age, number and percentage of neutrophils and lymphocytes, haemoglobin levels, platelet number, mean platelet volume (MPV), NLR (neutrophil count divided by the number of lymphocytes) and PMI (the number of platelets multiplied by the MPV). The exclusion criteria were as follows: having infection or inflammation; immunologic, splenic or renal diseases that may have affected platelet counts and MPV, pathologies other than a primary testicular tumour, having high levels of biomarker post-orchiectomy and metastasis in post-procedural metastatic evaluation. Peripheral blood samples were obtained during the preoperative period. Patients underwent metastatic evaluation after the operation. Serum biomarkers were re-evaluated at the appropriate period after the procedure. For the purpose of this study, localized testicular cancer was defined as stage 1 (1A and 1B) in patient with no metastasis at lymph nodes or distant organs.
STATISTICAL ANALYSIS
Statistical analyses were performed with the SPSS version 19.0 software (SPSS Inc., Chicago, IL, USA). The distribution of the data was determined by the Shapiro-Wilk test. The study data was evaluated using descriptive statistical methods. Mean, standard deviation, minimum, maximum, median, frequency and ratio was used to evaluate the study variables. Continuous variables were compared with the independent sample t test or the Mann-Whitney U test for two groups. For all tests, p values of less than 0.05 were considered statistically significant. A receiver operating characteristic (ROC) analysis was constructed to assess the discriminative ability of PMI, NLR and the ratio of the percentage of neutrophils to lymphocytes (NL%R) in localised testicular cancer.
RESULTS
This study included a control group of 38 healthy patients with a mean age of 32.8 ± 9.7 years and a study group of 38 patients with localised testicular cancer with a mean age of 30.84 ± 5.79 years. The pathological diagnostic distributions of the patients with testicular tumours were: pure seminoma (n = 13), mixed germ cell carcinoma (n = 20), embryonal carcinoma (n = 1), teratoma (n = 3) and Leydig cell carcinoma (n = 1). Tables 1 and 2 set the age and blood values of the patients in the study and control groups. The neutrophil counts and percentages were significantly higher in the patients with testicular cancer than in the control group (p < 0.001 and p = 0.01, respectively). The lymphocyte counts were not statistically different between the groups (p = 0.330), but there was a significant difference in the lymphocyte percentages between the groups (p = 0.001). The lymphocyte percentages were significantly lower in the study group with testicular cancer than in the control group. The NLR values in patients with testicular tumours were significantly higher than in the control patients with varicocele (p = 0.001) (Figure 1). There was also a significant difference between the groups in terms of their NL%R values (p < 0.001). The NL%R values in patients with testicular tumours were significantly higher than in the control patients with varicocele (Figure 1). A statistically significant difference was found between the groups regarding the platelet counts of the cases (p =0.019). The plateler counts in the patients with testicular tumours were significantly higher than those seen in the patients with varicoceles. A statistically significant difference was found between the groups regarding the PMI of the cases (p = 0.004). The PMI values in the patients with testicular tumours were significantly higher relative to those seen in the patients with varicoceles (Figure 2). No statitistical difference was detected between the groups in terms of haemoglobin levels.
Table 1. Age and hematological data of the patients
MPV: mean platelet volume; PMI: platelet mass index; AFP: alpha fetoprotein; B-HCG: human chorionic gonadotropin; LDH: lactate dehydrogenase.
Table 2. Blood values of the patients were shown according to the groupsMPV: mean platelet volume; PMI: platelet mass index. Values are expressed as mean ± standard deviation. p< 0.05 statistically significant.
* student-t test. aMann-Whitney U test
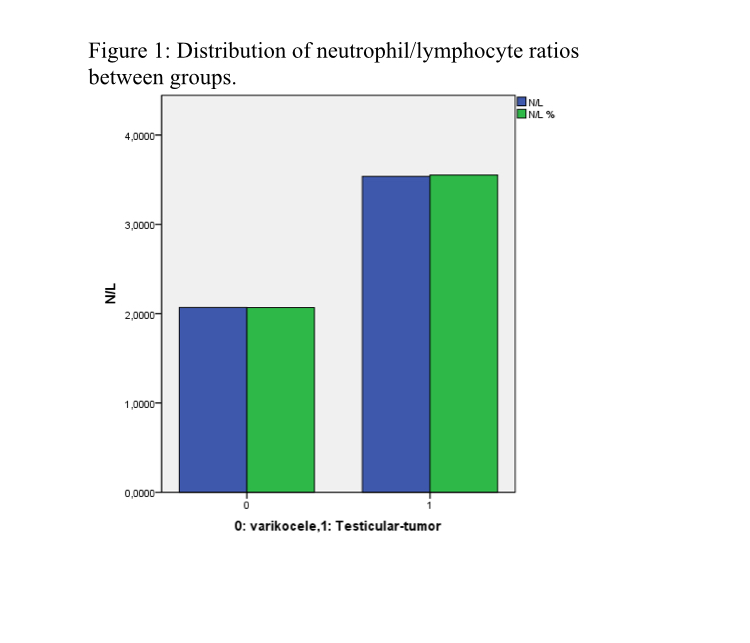
Figure 1. Distribution of neutrophil/lymphocyte ratios between groups.0: varicocele; 1: testicular tumours. N/L: neutrophil/lymphocyte ratios; N/L%: ratio of the percentage of neutrophils to lymphocytes.
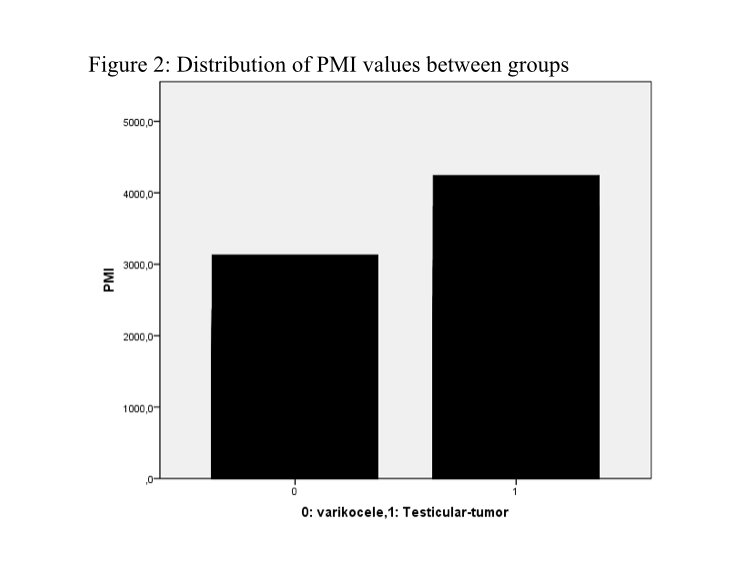
Figure 2. Distribution of PMI values between groups.0: varicocele; 1: testicular tumours. PMI: platelet mass index.
The area under the ROC curve for NLR in the localised testicular cancer patients was 0.74, (95% confidence interval (CI) = 0.62–0.85) with a threshold value of 2.06, 68% sensitivity and 64% specificity. The area under the ROC curve for the NL(%)R in the localised testicular cancer patients was 0.74, (95% CI = 0.62–0.85) with a threshold value of 2.04(%), 71% sensitivity and 61% specificity. The area under the ROC curve for the PMI in localised testicular cancer patients was 0.69 (95% CI = 0.57–0.81) with a threshold value of 1908.2, 76% sensitivity and 56% specificity (Figure 3).
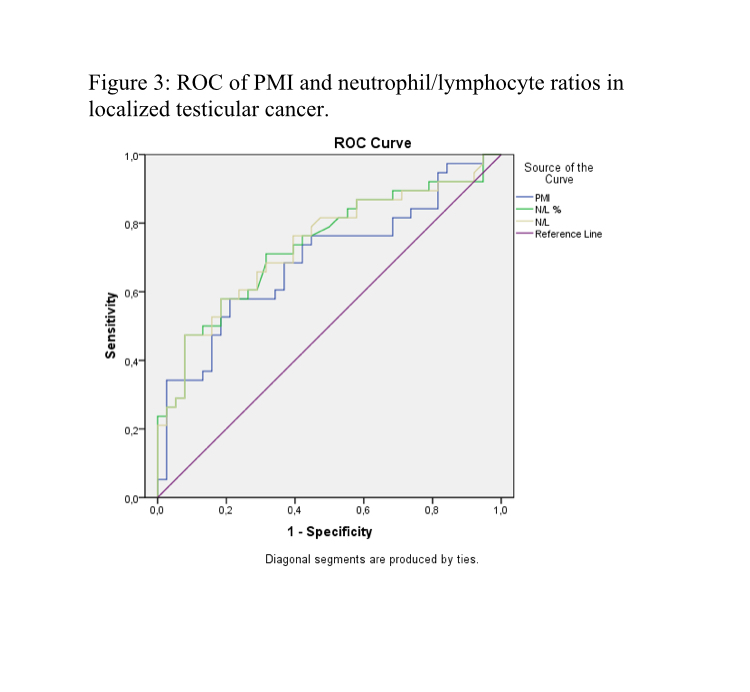
Figure 3. ROC of PMI and neutrophil/lymphocyte ratios in localized testicular cancer.PMI: platelet mass index; N/L: neutrophil/lymphocyte ratios; N/L%: ratio of the percentage of neutrophils to lymphocytes. PMI (area under curve (AUC)=0.69, 95% confidence interval (CI) = 0.57–0.81) ; N/L% (AUC=0.74, 95% CI = 0.62–0.85); N/L (AUC=0.74, 95% CI= 0.62–0.85).
DISCUSSION
The systemic inflammatory response that occurs in biological systems can be demonstrated by various haematological and biochemical parameters. Total white blood cell count, neutrophil and lymphocyte count, C-reactive protein and procalcitonin are the inflammatory markers that are typically monitored [11]. Platelets are located at the edge of the cellular immune system, outside the inflammatory pathways that have previously been described [12]. But in light of recently published data, thrombocytes have begun to move toward the centre of the inflammation process [13].
Systemic inflammation plays an important role in the development of cancer [14]. The degree of the biological system's inflammatory response and the mediators secreted by the tumour cells can vary according to tumour type [11]. This struggle between the tumour and the biological system is often overlooked by the existing prognostic measurements. The immune system is involved in cancer initiation and enhancement as well as cancer suppression. The clinical result depends on which of these effects dominates [11]. An increase in the number of neutrophils contributes to tumour development and is therefore interpreted as a poor prognostic indicator [15]. The systemic inflammatory response has been evaluated in various urological cancers, such as renal cell carcinoma, upper urinary tract cancer, bladder cancer and prostate cancer, and its potential for predicting positive surgical margins and progression-free survival has been demonstrated [11].
A limited number of studies have addressed the relationship between testicular cancer and immunity, but there is little evidence in the literature regarding the development and progression of testicular cancers and the role of the inflammatory response.
The prognostic indicators of age, gender, NLR and platelet counts have been found to be important indicators in urothelial cancers [16]. Of these, NLR is perhaps the most vigorously studied, particularly with respect to localised prostate cancer. Hakimi et al. reported that NLR values prior to radical prostatectomy surgery in locally advanced prostate cancer patients predicted biochemical recurrence [17]. However, these results could not be confirmed in a study carried out by Ipekci et al [18]. Experts have tried to explain this inconsistency by referencing the low patient numbers and the insufficient follow-up time. Ohno et al. Reported that the risk of recurrence in patients with non-metastatic renal cell carcinoma could be predicted with a combination of NLR and the disease stage [19]. Similarly, Kobayashi et al. showed that NLR may be a criterion for progression-free survival and response to treatment in metastatic renal cell carcinoma [20], while Hashimoto et al. found neutrophil counts to be a poor prognostic indicator before neoadjuvant chemotherapy in patients with non-metastatic upper urinary tract cancers [21]. Notably, Yuksel et al. were the first to examine NLR as a preoperative blood marker for localised testicular cancer patients; they predicted that NLR could be used as a biomarker for the preoperative period [11]. In our study, NLR was found to be significantly higher in patients with localised testicular cancer than in the control group. As in the previous study, our results support the theory that NLR may be a biomarker that can be used in the preoperative period. We found a cut-off value for NLR of 2.04 with 68% sensitivity and 64% specificity, similar to the previous study, in which the cut-off value was 2.06 with 69% sensitivity and 69% specificity.
Mediators such as transforming growth factor-beta, platelet-derived growth factor and prostaglandin E2, which induce the proliferation of cancer cells, are abundantly present in platelets [22]. The recently demonstrated relationship between cancer and thrombocytes has accelerated studies on the use of platelet parameters for cancer prognosis.
Similar to NLR, there is evidence to suggest that PLR could be a prognostic indicator for colorectal, gastric, breast and lung cancers [23]. Wang et al. reported that a high PLR rate in renal and prostate cancers was an indicator of poor overall survival in a meta-analysis of 20 studies evaluating urological cancer patients. However, this relationship was not found in patients with bladder cancer [23].
An increased platelet count has been shown to be a poor prognostic indicator in gastrointestinal and gynaecological cancers [24, 25]. The number of platelets in systemic circulation reflects the balance between production and destruction; therefore, the prognostic reliability of platelet counts has been debated. MPV, the most widely used criterion of platelet size, is a strong indicator of platelet activity. Studies have shown that significant changes in MPV values occur in some cancers [26]. A recent study by Wang et al. reported that low MPV values were associated with a poor prognosis in patients with muscle-invasive bladder cancer [27].
PMI is a biomarker that has recently attracted researchers' attention. In the first study on PMI, it was reported that unnecessary platelet transfusions can be prevented in neonatal intensive care units [28, 29]. The first study on PMI in urological cancers was conducted by Girgin et al. to predict early recurrence in prostate cancer [30]. In this study, a statistically significant negative correlation was observed between PMI and Gleason score, whereas no statistically significant difference was observed between PMI values and biochemical early recurrence. In the current study, PMI, MPV and total platelet count values were higher in the patients with testicular cancer than in the controls. The PMI cut-off value was 1908.2 with 76% sensitivity and 56% specificity. We believe that this elevated PMI value may have occurred in response to tumour formation, as there was no corresponding PMI spike in the control group.
There were a few limitations to this study. Firstly, it a single centre study based on retrospective hospital records. The study and control groups contained a relatively small sample set of patients. The data used to exclude the factors that may have affected platelet counts and volumes were dependent on hospital records. And also testis tumor subtypes were not correlated with PMI in our study. Lastly, this study had not a prognostic predictive design.
CONCLUSIONS
For patients with testicular tumors, there is generally a short period of time between the carcinogenic effect and the patients' referral to the clinic. In this cancer, hematological changes develop rapidly. Complete blood count (CBC) is a cheap and reproducible parameter that is often used in clinical practice, and the current trend is to increase the use of CBC data in cancer diagnosis and follow-up. In the current knowledge, it is still not possible to overcome unnecessary surgeries in testicular masses. Although we argue that hematologic data, especially PMI, may shed light on the prediction of malignancy of clinically-radiologically indistinguishable testicular masses in our study, this should be supported by well-designed, prospective large-scale studies.
ETHICAL CONSIDERATIONS
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. (Local Ethics Committee meeting no: 2018/03, protocol no: 2018-41-31 / 01).














