INTRODUCTION
Cardiac arrest is defined as the cessation of the mechanical activity of the heart, which is confirmed by the absence of signs of circulation such as loss of consciousness, apnea, and absence of palpable central pulse [1]. Around 80% of cases have a cardiac origin, and ischemic heart disease is the most common cause. Less frequent causes are cardiomyopathies, valvular heart diseases, congenital heart diseases, and arrhythmias. The remaining cases have a non-cardiac origin and can be caused by traumas, malignancies, non-traumatic hemorrhages (gastrointestinal, cerebrovascular, aortic dissection), asphyxia, and hypoxia, among others [2].
The incidence rates of cardiac arrest fluctuate according to the evaluated country. For instance, in the United States, the out-of-hospital cardiac arrest (OHCA) incidence in 2015 was 140.7/100000 person-year in adults [3]. In Peru, the national incidence of cardiac arrest is unknown, but studies such as that of Guillen, 2005 [4] and Escudero, 2011 [5], reported an incidence of 4 cardiac arrest cases for every 1000 patients who were treated in the emergency department of the Dos de Mayo National Hospital during the period January 2004 – August 2004 and an incidence of 2.56 cardiac arrest cases for every 1000 patients in the emergency department of the Jose Casimiro Ulloa Emergency Hospital during the period January 2008 – August 2008, respectively.
60% to 80% of the cardiac arrest cases are witnessed; however cardiopulmonary resuscitation (CPR) is only initiated in 1 out of 5 cases [6]. Many witnesses are relatives who live with the victim as 4 out of 5 cardiac arrests occur at home [3, 7]. Starting a high-quality CPR may double or triple the survival rate for cardiac arrest victims [8]. For instance, in the systematic review performed by Yan et al., 2020 [9], the survival of patients with unwitnessed OHCA was reported to be 4.4% while survival was 11.3% if a witness performed CPR.
For these reasons, CPR training in the general population is the main tool to reduce morbidity and mortality of cardiac arrest and in the last years, educational interventions teaching CPR to the general population have been implemented intending to improve cardiac arrest survival rates with diverse teaching methodologies. The Family & Friends CPR course of the American Heart Association (AHA) is one such example aimed at the general community and is developed with a video and a manikin to practice the CPR skills. By this time, no research has been reported evaluating the effectiveness of this intervention.
In Peru, the majority of research related to CPR evaluates theoretical knowledge level in different subgroups, such as medical students, healthcare workers, police officers, and schoolchildren. However, there are few studies such as that of Robles, 2013 [10], which have evaluated the effectiveness of educational interventions. This study was performed in 4th and 5th grade students with a five-session intervention developed by the researcher, improving theoretical knowledge level and CPR practical skills. However, in Peru, no interventions specifically targeting populations with a greater risk of cardiac arrest have been performed.
Different scores can be used to identify people at greatest risk to develop cardiovascular events and suffer from a cardiac arrest. One of them is the ASCVD (Atherosclerotic Cardiovascular Disease) cardiovascular risk estimator of the American College of Cardiology (ACC)/AHA of 2013, which considers variables such as type 2 diabetes mellitus, systolic blood pressure (elevated in hypertensive patients), age, gender, race, total cholesterol, smoking, and if the patient receives antihypertensive treatment [11]. This scale classifies people in low (< 7.5%) or high (> 7.5%) risk to suffer from a cardiovascular event in the next 10 years, defined as a fatal or non-fatal acute myocardial infarction and fatal or non-fatal stroke [12].
This scale is useful because both the variables it contains to estimate the risk and the cardiovascular events it measures are independently associated with an increased risk of cardiac arrest. For example, we know that arterial hypertension increases the risk of cardiac arrest both by itself and by the ventricular hypertrophy that it generates [13]. Furthermore, people with type 2 diabetes mellitus have a two to four-fold increased risk of suffering from cardiac arrest [14]. Additionally, people with a previous episode of an acute myocardial infarction have a four-to-six-fold increased risk, with an annual incidence of 2-4% in this group [15]. Lastly, in people who suffered from an ischemic stroke, the predisposition to develop arrhythmias and myocardial injuries after that event increases the risk of suffering a future cardiac arrest [16]. All of these risk factors affect the cardiac arrest incidence, being approximately 6/1000 person-years in patients with any previous cardiac disease, while in people with no cardiac pathology, this incidence decreases to 0.8/1000 person-age [17].
For this reason, teaching CPR to relatives of patients with high cardiovascular risk or who have suffered a cardiovascular event would have a high impact, as performing interventions directed to this population (which has more probabilities to be witnesses of a cardiac arrest) would be a cost-effective strategy to increase the CPR rates performed by witnesses [18]. Moreover, Cartledge et al., 2016 [19] and Liu, et al. 2009 [20] observed that relatives of cardiac patients have more interest in learning and practicing their CPR skills in comparison with the general population.
Consequently, our study aimed to demonstrate the effectiveness of the Family & Friends CPR course of the American Heart Association in learning CPR in relatives of patients with high cardiovascular risk or who have suffered a cardiovascular event.
MATERIALS AND METHODS
An analytical, quasi-experimental, prospective, before-and-after study was conducted, aiming to demonstrate the effectiveness of teaching the Family & Friends CPR course in the theoretical and practical learning of cardiopulmonary resuscitation in relatives of patients with high cardiovascular risk or who have suffered a cardiovascular event. High cardiovascular risk was defined according to the ASCVD cardiovascular risk estimator of the ACC/AHA in 2013, as having a risk equal or greater than 7.5% of developing a cardiovascular event in the next 10 years. Moreover, a history of cardiovascular event was defined as having suffered from an acute myocardial infarction or a stroke.
Participants were selected through a consecutive non-probability sampling during the outpatient consultation of the Cardiology Department of the Cayetano Heredia Hospital in Lima, Peru. To be considered in the research, they had to meet the following inclusion criteria: at least 18 years of age, living in the same house as the patient, and knowing how to read. Those who temporarily lived in the patient's house, had previous CPR training, and participants who were unable to perform physical effort due to any disease, disability, and medical treatment were all excluded.
The sample size was estimated at 20 people, with a confidence interval of 95% and a power of 80%. The aforementioned sample-sized was obtained by considering a mean of 8 ± 5 previous to the intervention and a mean of 13 ± 3 after the intervention.
The educational intervention used was the Family & Friends CPR course which is given by the International Training Center of the Cayetano Heredia Peruvian University which is accredited by the American Heart Association and directed by the researchers (training facilitators qualified to conduct the course). This course is developed with a video that explains the theoretical and practical parts of CPR. Primary survey, compressions, and ventilations are practiced through the “practice-while-watching” technique, in which the participant practices the maneuvers with a manikin while looking at a person performing the same activities in the video. Participants are given immediate feedback and time for repetition to improve performance (deliberate practice approach). For this research, the modules “Hand-only CPR in adults and AED” and “CPR with ventilation in adults” were taught.
To measure the theoretical knowledge level about CPR, a questionnaire created by the authors was used. This questionnaire included topics such as definitions of cardiac arrest and CPR, adequate sequence of the primary survey, chest compressions, and adequate ventilation. Demographic data of participants such as gender, age, and level of education were also collected. The questionnaire consisted of 20 questions, each with one correct answer and 3 alternatives with one point given for each correct answer. Based on the score, the participants were rated in good (16-20 points), regular (11-15 points) or bad (0-10 points) theoretical knowledge level in three moments: before, immediately after, and one month after the intervention.
To validate the instrument, a pilot that included 10 participants was performed, in which the comprehension of the questionnaire was verified. The result was satisfactory and did not require grammatical adaptations in the questions or statements. To evaluate the reliability, the instrument was analyzed with the Cronbach's alpha coefficient and a result of 0.8539 was obtained, which indicated that the reliability of the instrument was good (it is considered that values from 0.7 up to 0.8 are acceptable, from 0.8 up to 0.9 are good, and from 0.9 up to 1.0 are excellent).
The practical learning level was measured by both researchers through the use of the checklist of the Basic Life Support (BLS) course of the American Heart Association, which contains 16 items related to skills and abilities in CPR and evaluates primary survey, chest compressions, and ventilations. One point was given for each item performed adequately, while no points were given if the participant did not perform an item or performed it inadequately. Based on the obtained score, the participants were rated in good (13-16 points), regular (9-12 points), or bad (0-8 points) practical knowledge levels in two moments: immediately after, and one month after the intervention. The participants used feedback bracelets that were activated when they performed compressions at a frequency of 100-120 per minute and a minimum depth of 5 cm to have greater accuracy of the practical evaluation.
The statistical package STATA v.16 was used for data analysis. Central tendency measures (mean or median) were used for numerical variables and the demographical ones were resumed in tables and graphics. Paired T-test was used to analyze theoretical knowledge as they had normal distribution according to the Shapiro Wilk test. Conversely, the Wilcoxon signed-rank test was used to analyze practical knowledge as these variables did not follow a normal distribution. A multivariate regression model was made to evaluate the role of confounding factors on final results.
This study was approved by the Ethics Committee of the Cayetano Heredia Peruvian University, and written informed consent was obtained from all trained participants
RESULTS
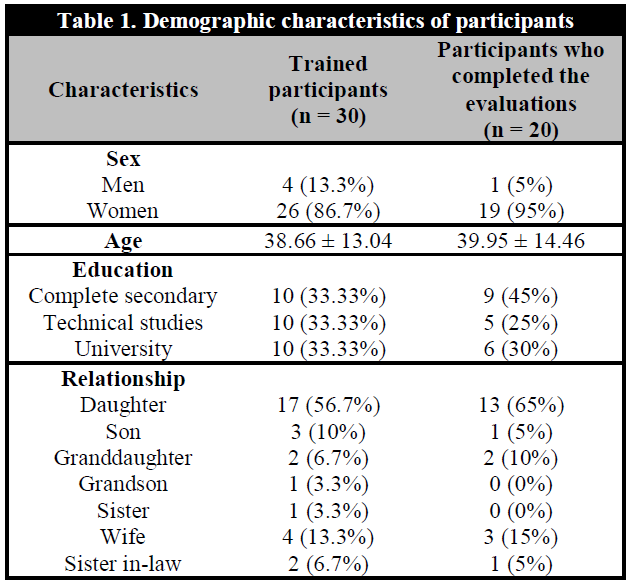
Relatives of 23 high risk patients were recruited for a total of 30 participants who were trained and completed the evaluations before and immediately after the intervention, and 20 of them completed the evaluations one month after the intervention. Participants were more frequently women (86.7%), the average age was 36.88 ± 13.04 years old and the degree of instruction was equally distributed (complete secondary school 33.3%, technical studies 33.3%, and university education 33.3%). Moreover, participants were mostly the daughters (56.7%) or wives (13.3%). Other relationships were: son (10%), granddaughter (6.7%), sister-in-law (6.7%), sister (3.3%), and grandson (3.3%) (Table 1).
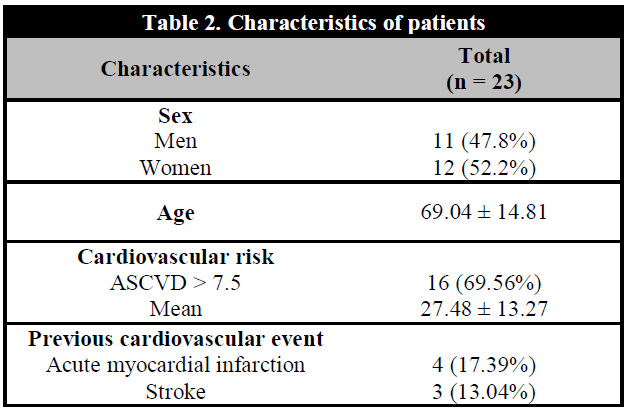
Concerning the 23 high risk patients, the gender distribution was uniform (52.5% women, 47.8% men), with an average age of 69.04 ± 14.81 years old. 7 out of the 23 patients had a previous cardiovascular event (4 with acute myocardial infarction and 3 with ischemic stroke). The remaining 16 patients had a high cardiovascular risk, with a mean of 27.48% ± 13.27% of cardiovascular risk according to the ASCVD scale of the ACC/AHA in 2013 (Table 2).
With regard to theoretical knowledge (TK), the mean of the 30 participants before the intervention (TKBI) was 8.63 ± 2.47 (overall bad TK level, confidence interval (CI) at 95% 7.71 – 9.56), in which 22 of the 30 people obtained a bad TK (7.59 ± 1.99) and 8 a regular TK (11.5 ± 0.76). Moreover, the mean immediately after the intervention (TKIAI) was 17.33 ± 2.02 (overall good TK level; CI at 95% 15.58-18.09), in which 7 of the 30 people obtained a regular TK (14.43 ± 0.79) and 23 of them obtained a good TK (18.22 ± 1.31). Furthermore, the 20 participants that completed the evaluation a month after the intervention (TK1MAI) had a mean of 16.5 ± 1.91 (overall good TK level, CI at 95% 15.61-17.39), in which 6 obtained a regular TK (14.17 ± 0.41) and 14 of them obtained a good TK (17.5 ± 1.29) (Table 3).
Tabld 3. Theorical knowledge before, immediately after and a month after the intervention
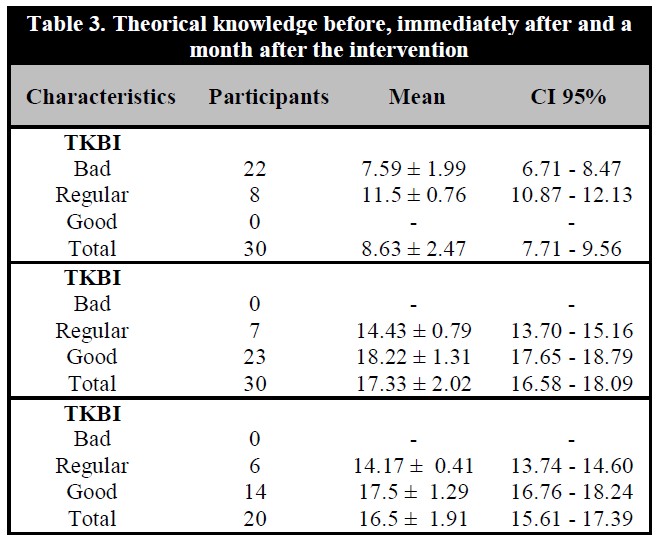
TKBI: Theoretical knowledge before the intervention; TKIAI: Theoretical knowledge immediately after the intervention; TK1MAI: Theoretical knowledge a month after the intervention.
A paired T-test was used to compare the differences between the means in the three moments. When comparing the TKBI means against TKIAI of the 30 participants and TKBI against TK1MAI of the 20 who completed the research, a statistic <0.001 (<0.05) was obtained in both cases, meaning that the theoretical knowledge level improvement was statistically significant with the intervention. Besides that, when comparing the means of TKIAI against TK1MAI of the 20 participants who completed the research, a statistic of 0.074 was obtained (>0.05, statistically non-significant), which implies that there was no difference between the means of theoretical knowledge achieved with the intervention and the increase in theoretical knowledge level was maintained after a month. After adjusting for confounders, a multivariate regression analysis showed a significant improvement in CPR knowledge with the intervention, and variables like age and degree of instruction didn't have a statistically significant influence on results.
In the case of practical knowledge (PK), the medians of the results were evaluated as they did not follow a normal distribution. The median of the 30 participants immediately after the intervention (PKIAI) was 15 (the obtained results ranged between 13 and 16 points), indicating all of them had a good PK. The median of the 20 participants who completed the evaluation one month after the intervention (PK1MAI) was 15 (the obtained results ranged between 12 and 16 points), in which 2 obtained a regular PK (median = 12) and 18 obtained a good PK (median = 15) (Table 4). Thus, in both moments participants maintained a good level of practical knowledge.
To compare if there were differences between PKIAI and PK1MAI, the Wilcoxon signed-rank test was used as they did not follow a normal distribution. A statistic of 0.23 (> 0.05) was obtained. Thus, the medians of PKIAI and PK1MAI have no statistically significant difference, which implies that the practical knowledge level was maintained a month after the intervention.
DISCUSSION
In our research, the majority of trained people were female. This distribution aligns with other studies such as the one of Case et al., 2018 [21] in which women were identified as the ones who most frequently (65.6%) activate the emergency response in cases of OHCA. Moreover, it agrees with the exposed by González-Salvado et al., 2020 [22] in which cardiac arrest witnesses are more frequently women, namely wives or relatives of the victims, which suggests that teaching should be directed to this group of people. Additionally, all participants came from a low socio-economic status (SES) since the Cayetano Heredia Hospital is a reference center for patients from unfavored areas of the capital of Peru. Targeting this population is important because a low SES is associated with lower rates of bystander CPR, lower rates of survival [23] and lower training rates [24].
In Peru, the majority of studies evaluated CPR knowledge level in diverse populations, with few performing educational interventions, such as Sandoval, 2019 [25], in which a group of nurses obtained a regular level of theoretical and practical knowledge after an educational intervention created by the author. In another such study, Robles, 2013 [10], an increase in the level of theoretical and practical knowledge in students of 4th and 5th year of secondary school was obtained with a five-session intervention developed by the author. However, our research is novel, in that we evaluate the learning one month after the intervention, in which it was possible to trend the evolution of the learning level through time. Furthermore, this is the first study in Peru that specifically trains relatives of patients with a high cardiovascular risk, who have a higher risk of witnessing a cardiac arrest compared to the general population. In consequence, this research aims to promote and continue the training to relatives and caregivers of people from this group. Another relevant aspect of our research is that positive results were achieved with a one-session course, in comparison to other studies that required multiple sessions to complete their training [10, 26, 27]. This decreases the possibility of giving incomplete training when developing the course, as there are more probabilities that participants do not finish the intervention if it is divided into several sessions. Lastly, practical skills were developed with a manikin and supported by a feedback device, achieving a better quality and reliability in chest compressions [22]. Even though our intervention achieved a good learning level in theoretical and practical knowledge, we consider that having achieved a good level in practical knowledge with the Family & Friends CPR course is the most significant finding of our research, since performing a high-quality CPR is the most important strategy in a context of a real situation of OHCA with aiming to save a life.
It is important to highlight that, according to the skills and abilities checklist for CPR in adults used for this research, participants had fewer mistakes in the items that evaluated the quality of chest compressions both in the evaluation immediately after and one month after the intervention. According to the AHA, this is a positive result as high-quality chest compressions (with adequate frequency and depth) are the main components of cardiopulmonary resuscitation. Additionally, an adequate chest compression depth is associated with improved clinical outcomes from cardiac arrest [28], and all participants achieved a minimum depth of 5 cm based on the feedback bracelets that were used during training. Moreover, the course trained and verified the learning of the activation of the emergency response, a key step of the OHCA chain of survival [29].
Several studies have compared conventional CPR (compressions associated with ventilations) with hands-only CPR (only chest compressions), with conflicting results. In some studies, such as Bobrow et al., 2010 [30], it is concluded that hands-only bystander CPR in patients with OHCA is associated with a higher survival rate compared to conventional CPR; while Ogawa et al., 2011 [31], reports the opposite. Other studies, such as the one performed by Iwami et al., 2007 [32] and Rea et al. 2010 [33], report that there is no difference in survival rates between the patients that receive any of the two resuscitation modalities. However, all of them agree that independently of the modality that is performed, results show an increase in patient survival rate in comparison with not performing any type of resuscitation. Finally, AHA recommends that even if the resuscitators are not trained in giving ventilations or do not want to perform them, they should start chest compressions immediately in addition to activating the emergency response [29]. The intervention used for this research included a teaching module called “Only-Hands CPR in adults and AED”, but also has optional learning modules such as “CPR with ventilation in adults”, so that participants could be trained according to their preferences. A deliberate practice approach with an added mastery learning approach (use of deliberate practice training along with testing to set a standard that implies mastery of the technique) was used, which is recommended to improve skill acquisition and performance [28].
According to the results obtained in this research, participants achieved a good level of theoretical and practical learning immediately after the intervention, not finding a significant difference when reevaluating them one month after. In other words, the level of theoretical and practical learning is maintained through time. This aligns with the research performed by Kim et al., 2016 [34], who also showed an increase in the level of theoretical knowledge immediately after and a month after their intervention, as well as an increase of practical level immediately after in a similar population to ours. There are other studies such as the one of Saad et al., 2019 [26], who followed participants for a longer period, showing that, after receiving a BLS training of 10 hours divided into 3 sessions, medical students showed a 90% retention of CPR skills in the first month, while the retention was only of 61% after 42 months. Based on these results, the authors suggest retraining between 18 to 24 months as a strategy.
According to AHA [35], the interval established for retraining is two years. However, quick and frequent reminder sessions may be a tool to improve retention of CPR learning [22], as is shown by González-Salvado et al., 2018 [27] where two groups were trained, one with a standard BLS course and the other one received practical sessions with a manikin every two weeks, starting with 30 seconds of compressions until reaching 2 minutes in week 8. Both groups were reevaluated after two months. It was observed that the second group presented better retention of the protocol in comparison with the standard group [27]. Even conducting a 15-minute booster training 6 months after the first educational intervention can help participants retain CPR skills for up to 1 year [36].
Although the participation of the trained people in our research ended when they were reevaluated one month after the intervention, at that moment all of them received personalized feedback of their mistakes in the theoretical and practical parts, making sure that all of them finished the investigation without mistakes in the technique and were prepared to respond in a real situation of cardiac arrest. This is beneficial, since implementing monthly retraining with duration of two minutes of practice on a manikin associated with real-time feedback, improved practical CPR skills [37]. Limitations of our research included that some participants were lost to follow up and could not be re-evaluated after one month. Furthermore, it was not analyzed if the motivation level of our participants, since they were all relatives of patients with high cardiovascular risk, would have any impact on the learning level in comparison with the general population.
Even though this study shows that the Family & Friends CPR course is effective in the theoretical and practical learning of relatives of patients with high cardiovascular risk or who have suffered a cardiovascular event, it is imperative to increase studies and training to a higher quantity of people from every socioeconomic level and geographic areas of the country (aiming to increase the bystander CPR rates) and more research related to cardiac arrest etiologies and post-resuscitation care is needed. Furthermore, public policies such as standardizing the register and report of cardiac arrests and CPR are needed in the country, so that the real incidence and survival rates can be determined in our country. Additionally, the AHA recommendation of implementing CPR training at school as a mandatory activity could be adopted so the proportion of trained adults increases, the population is more aware of the importance of CPR in the context of a cardiac arrest and a repeated exposition to the technique will generate an improvement of itself over time [38]. For example, in some Scandinavian countries where education of schoolchildren in CPR is mandatory, bystander CPR rates are high [39]. An easy and low-cost strategy consists of CPR training at least two hours a year to students starting at the age of 12, which would allow for the training of a whole new generation and could have a high impact on public health [40], though it would require additional training and education of personnel to teach the technique and direct the courses. Furthermore, starting CPR training at a young age allows these skills to be retained for a lifetime and be easily refreshed [41]. Also, early training may instill a positive attitude and confidence toward a real-life situation [28]. On the other hand, campaigns should be promoted to decrease the barriers that inhibit witnesses to perform CPR, which includes fear of causing damage, fear of contracting infectious diseases, panic, rejection of mouth-to-mouth contact, concern over the technique's high complexity, among others [30]. Finally, we hope that interventions to improve primordial, primary, secondary, and tertiary prevention of cardiovascular disease in our country increase in the future, including cardiac rehabilitation programs that include teaching CPR to patients and their families [27]. Additionally, care managers should be incorporated in health care systems to support the specialists, like in project Leonardo, in which an empowerment approach was implemented and the care manager worked with patients with chronic diseases to change their health behaviors by increasing their health knowledge, allowing patients to take an active role in their health [42].
In conclusion, the Family & Friends CPR course was effective in improving the theoretical and practical knowledge in cardiopulmonary resuscitation in relatives of patients with high cardiovascular risk or who have suffered a cardiovascular event, and it was maintained through time.