1. INTRODUCTION
Urinary tract infection (UTI) is considered one of the most common infections usually diagnosed in different health units and hospitals [1]. UTI is linked to a high level of morbidity and mortality in high-risk subgroups including children, pregnant women, and immunocompromised patients [2, 3]. The bacteria attack both upper and\or lower urinary tract parts such as ureter, urethra, and the bladder regions causing UTI appears as dysuria, urinary incontinence, or haematuria which could lead to kidney disease and blood pressure disorders [4]. Recurrent urinary tract infection (RUTI) is defined as three infections with three positive urine cultures within a year or two infections within a half year [5] and it is estimated that 80% of RUTIs are reinfection [6]. The morbidity accompanying upper tract UTI during the pregnancy period is significant and causes prematurity, low birth weight, preeclampsia, and cesarean delivery. Thus, diagnosis and treatment of asymptomatic bacteriuria are one of the standard care requirements of pregnant women [7]. E. coli is considered the most frequent pathogen isolated in 85% of UTI patients. Other significant pathogens can also cause UTI including Proteus spp. S. saprophyticus, Klebsiella spp. and other Enterobacteriaceae. Group B streptococcus bacteria are seen in diabetic patients, and Pseudomonas infections are seen more in those with chronic-catheterized patients [7, 8, 9].
Despite the fact that urine culturing is considered the gold standard for the diagnosis of UTIs; it is laborious and time-consuming requires 48h for the results to be confirmed [10]. Antimicrobial treatment should be begun shortly to eliminate infection, prevent bacteriemia, and improve treatment outcomes reducing renal scarring and kidney damage due to excessive antimicrobial usage with adverse effects and bacteria resistance [11]. Therefore, other methods of UTI diagnosis are needed. It has been reported that a change in platelet count could be used as an index for a rapid and probable diagnosis of UTI without the need to wait for urine culture results [12]. Complete blood count (CBC) is commonly used for several infections evaluation [13]. In routine medical diagnosis for patients with UTI, platelet parameters are highly used as an examination to determine any changes made using an automated blood cell analyzer [14].
Made in bone marrow megakaryocyte cells, Platelets are the smallest blood cells. They play the main role in the blood hemostasis, coagulation process, and when activated they are known to participate in host defense [12, 15]. During the inflammation process, the count of platelets increase as a part of the acute phase reaction [11]. Changes in platelet count are used to diagnose infectious and inflammatory diseases [16].
While the correlation of platelet indices had been studied due to its role as an inflammation marker in several diseases [11], there is a need for more data about its response to UTI diagnosis in women. Without extra payment, the platelet count can be determined routinely as a part of the CBC, which is usually ordered by physicians [14]. The alteration in platelet count can be used as a reliable index for the initial prediction of the Gram-type bacterial agent causing UTI with no need to wait for culture results. In this study, due to the role of bacterial species causing UTI in women and platelet count have not widely studied, we hypothesize a positive relationship between platelet count and the Gram type of organism. This could aid in the selection of antimicrobial treatment.
2. MATERIAL AND METHODS
This study was conducted at the Laboratory of Albaraa hospital for women admitted to the Maternity Department with suspected or diagnosed Urinary Tract Infection between 2017 and 2019. The suspected UTI cases were assessed during routine examination of the female patients by the hospital MD staff depending on usual symptoms. Patients with sepsis, iron deficiency anemia, malignant tumors, collagen disorders, or surgical operations and those who are on medications affecting platelet count are excluded.
All urine specimens were midstream clean catches. Each specimen had been processed on blood agar and MacConkey agar with a standard loop followed by overnight incubation at 37˚C. All no-growth cultures served as a control group. Total platelet count examined in our study obtained from CBC results, was tested using a hematology analyzer (Mindray BC-3000plus) at the same period of UTI episode.
3. RESULTS
Urine samples were obtained from 193 women suspected of having urinary tract infections (age 29-36 years) (Table 1). Of these specimens, 101 (52%) gave positive cultures. The rest of the specimens was considered as a control group. Of the specimens with positive cultures, 79 (79%) gave pure colonies and the remaining specimens produced mixed growth. Of the pure positive cultures, 45 (57%) gave growth Gram-negative bacteria and the rest with Gram-positive bacteria. Escherichia coli was the most isolated Gram-negative bacteria (58%) and Streptococcus spp. were the commonest Gram-positive bacteria 27/34 (79%).
Table 1. Distribution of bacterial urinary tract infections in women (n=193).
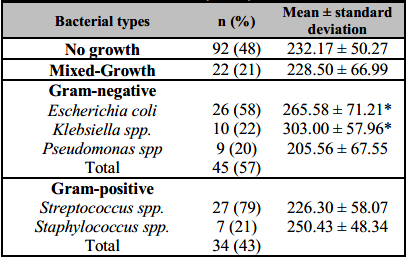
*Significantly higher in subjects (p < 0.05) compared to No growth group.
During the UTI episode, the mean platelet count was significantly higher during the Gram-negative bacterial infections (mean, SD: 261.89*103/µl ± 73.752) than Gram-positive and No growth group (p = 0.03) (Table 2). Gram-positive bacteria, Mixed-growth, and No-growth groups had almost a similar mean platelet count (Figure 1). Klebsiella spp. and E. coli were associated with the highest mean platelet count 303.00*103/µl ± 57.960, 265.58*103/µl ± 71.211, respectively) (Table 1) comparing with the no-growth group 232.17 ± 50.27 (Figure 2, p < 0.05), further highlighting the possible association between platelet counts and bacterial species in UTI.
Table 2. Comparison of mean platelet counts of urinary tract infections in women (n=193).
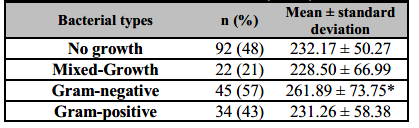
*Significantly higher in subjects (p = 0.03) compared to No growth group.
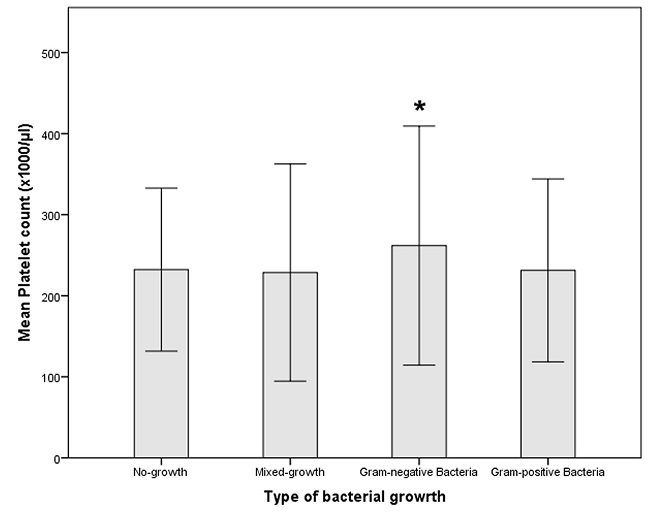
Figure 1: Mean platelet counts are shown for women infected with either gram-positive or gram-negative pathogens.Mean platelet count in Gram-Negative-infected women (mean, SD: 261.89*103/µl ± 73.752) was significantly higher than in Gram-positive ones and other groups. Data shown are mean ± SD.
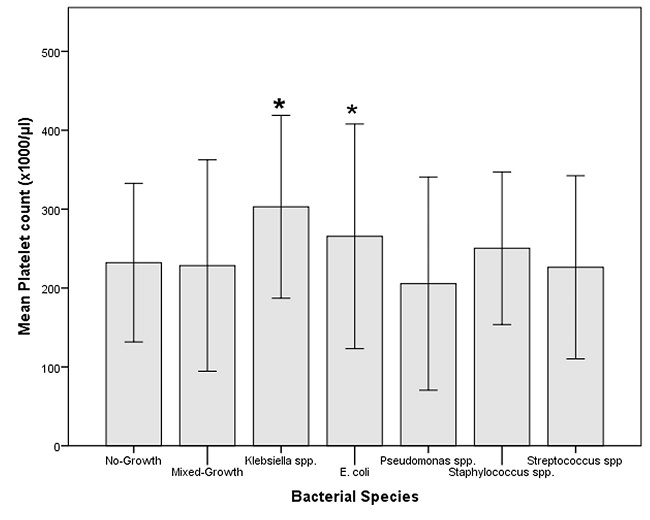
Figure 2: Mean platelet counts are shown for women infected with each bacterial type compared with No-growth (control) and Mixed-growth.Mean platelet count in Klebsiella spp. and E. coli-infected women were the highest level than other group (mean, SD: 303.00*103/µl ± 57.960, 265.58*103/µl ± 71.211 respectively).
4. DISCUSSION
Urinary tract infection (UTI) is one of the most common human diseases, being a challenge to the physician in the diagnosis process [17]. UTI is seen more in women than men. A number of risk factors could contribute to it, including physiological and anatomic, genetic, and functional status [18]. In addition, it has been reported that the high rate of occurrence may be due to hormonal alterations during pregnancy, which leads to anatomic changes in ureteric musculature. This might possibly be assisted possibly by mechanical pressure from the gravid uterus resulting in urinary stasis that consequently increases bacterial proliferation in urine; which is regarded as a perfect culture media [19]. Although the diagnosis tools of infectious diseases have been developed through time, more effective and simple practical diagnosis methods are still needed [20, 21]. It is believed that platelets are activated and participated in the host defence system in infections. This is in addition to creating oxidative molecules and cytotoxic free radicals [12]. Besides, differences in platelet count were seen in several clinical conditions [11, 12]. This study showed that there are quantitative variations in the platelet's response to both Gram-negative & Gram-positive bacteria caused UTI in women. The outcomes of the present study revealed that the most common bacterial pathogens isolated from the study cases were Streptococci spp. 27 (34%), E. coli 26 (33%), Klebsiella spp. 10 (13%), Pseudomonas spp. 9 (11.0%), Staphylococcus 7 (9%). This finding in agreement with the findings of other reports which indicate that Gram-negative bacteria, predominantly E. coli was the most common pathogen isolated from patients with UTIs locally and worldwide [5, 17, 22].
Response of platelets to different infections has not been widely characterized for human bodies. Acute infections are not frequently related to thrombocytosis because megakaryopoiesis is inhibited at acute infection episodes by a number of aspects such as bacterial endotoxin, transforming growth factor b, and tumour necrosis factor. In contrast, chronic infections are regularly associated with responsive thrombocytosis [23]. Although specific platelet responses to different bacterial infectious agents have not been extensively studied in vivo in humans, various studies showed conflicting results on platelet count in patients with different bacterial infectious diseases in terms of gender, age group, and size of injury-related-infection (severity of infection). Mean platelet counts in our study results were significantly higher in Gram-negative bacterial infections than with Gram-positive bacterial infection conversely to previous studies [24]. A possible explanation could be age differences of age groups as mentioned earlier in this study (adult women with an age range of 29-36) and those previous studies among children ranged from 2 months to 14 years [11, 14, 25].
Among Gram-negative bacterial pathogens, Klebsiella spp. caused the highest increase in platelet count; Klebsiella spp. has the ability to express lipopolysaccharides (LPS with O antigen) and capsular polysaccharides (K antigen) which both are contributing to its virulence. There is a variance in the genetic composition of O antigen between Klebsiella spp. and other Gram-negative bacteria, which is critical for Klebsiella spp. in its ability to resist complement-mediated opsonophagocytic killing [26]. These variations in Klebsiella spp. might be responsible for the maximum effect on platelet count compared to other bacterial pathogens as seen in our study. The quick response to the presence of lipid (A) in lipopolysaccharide (endotoxin) released after bacterial cell membrane degradation of Gram-negative bacteria consequently reactivate bone marrow within a day leading to high production of larger and more active platelets [11, 12]. Similarly, current study results showed an increase in platelet counts with Gram-negative bacterial UTIs compared with Gram-positive. The small number of Gram-positive bacteria might be the cause of UTI in our study. While at the same time, there was no significant difference in a Gram-positive bacterial infection group in comparison with the control group. Therefore, platelet count and can be used as a direct indicator of the gram type of bacterial pathogen agent causing UTI.
According to our results, platelet count obtained during routine CBC analysis could be useful indicator of UTI in women. It could predict the Gram-type of bacterial pathogen causes UTI. However, several studies identified the significant correlation amongst platelet parameters including platelet count, mean platelet volume (MPV), and platelet distribution width (PDW) in children in which observed converse results in various clinical conditions [25]. Therefore, further studies are needed, as more data would give better clear evaluation to understand the platelet parameters role especially in those with recurrent UTI.
This study had a number of limitations. First, the size of the sample was too small. As a result, the findings obtained from the analysis of specimens may not dependable. It would be better to include other women groups with severe cases such as those who were admitted into intensive care units or catheterized women. Additionally, due to the availability of only platelet count, we were unable to study the relationship between platelet count, MPV, and PDW in women during UTI. Thus, further studies are needed in order to clarify the clinical meaning. Furthermore, the specific response to different microorganism agents has not been extensively characterized for UTI in women. Moreover, it would be valuable to study all platelet parameters data during infection until the end of treatment.
5. CONCLUSIONS
Although urine culturing continues to be the primary (standard) tool for UTI diagnosis, early diagnosis and management would prevent any further complications. Due to the significant role of platelets in the hemostatic component in pathophysiology during infection occurrences. Our findings suggest that there is an association between platelet count and the Gram-type of bacterial agent causing UTI among women. Further investigation in parallel with more UTI Cases is needed in order to achieve better understanding of the basis of the effect of a particular organism on platelet counts and other platelet parameters.














