1. INTRODUCTION
Mucormycosis (Phycomycosis, zygomycosis) is an is an invasive fungal infection and rapidly progressive clinical syndrome caused by fungi belonging to the Mucorales order and the Mucoraceae family and characterized by infarct and necrosis resulting in high rates of morbidity and mortality [1, 2]. The pathophysiology of mucormycosis involves inhalation of fungal spores through the nose or mouth or even through a skin laceration [2]. Mainly, uncontrolled diabetes, long-term corticosteroid usage, and immunosuppressive therapies, and hematologic malignancies such as lymphoma, leukemia, are predisposing factors for mucormycosis. Although rare, healthy people may also become infected [1, 2].
The incidence of mucormycosis is unknown. There were 929 cases of mucormycosis reported by Roden MM et al. [3] depending on this data, diabetes mellitus and hematologic malignancies are the most common risk factors for mucormycosis. Based on anatomic localization, mucormycosis can be classified into six forms: rhino cerebral, pulmonary, cutaneous, gastrointestinal, disseminated, and uncommon presentations [4, 5]. Pulmonary mucormycosis has a poor prognosis, with a mortality rate of 80% [6]. Helpful tests for the diagnosis of pulmonary mucormycosis are radiodiagnostic tests, bronchoalveolar lavage specimens, and histopathological biopsy specimens. A reverse halo sign is one of the common computed tomography (CT) scan findings in pulmonary mucormycosis. Additionally, focal consolidations, masses, pleural effusions, or multiple nodules with airway-invasive features (such as clusters of centrilobular nodules, peribronchial consolidations, and bronchial wall thickening) may also be seen [7].
A chronic myelomonocytic leukaemia (CMML) is a clonal malignant hematopoietic stem cell disorder characterized by clinical and pathological features of both a myelodysplastic syndrome and myeloproliferative neoplasm. CMML is classified as a myelodysplastic/myeloproliferative neoplasm by the 2016 World Health Organization (WHO) classification of hematopoietic tumors [8]. Chronic Myelomonocytic Leukaemia is a genetically diverse hematologic malignancy characterized by cytopenias with or without leukocytosis, marrow dysplasia, monocytosis, splenomegaly, and a propensity to transform into acute myeloid leukemia [9]. The purpose of this case is to report an uncommon case of mucormycosis related to the use of the home-ventilator machine in a patient with diagnosis of chronic obstructive pulmonary disease and CMML.
2. CASE REPORT
A 64-year-old male patient presented to the hospital with complaints of weakness, cough, and fever with 38oC, and a blood pressure of 120/70 mmHg. He had mild hypoxia with oxygen saturation of 89% while breathing room air. His respiratory rate was 24 breaths/min and chest examination revealed crackles at the bases of both lungs. His extraoral examination was normal. On his medical history, he has coronary heart disease, chronic obstructive pulmonary disease (COPD) and using the home-ventilator machine for COPD, CMML and treated with azacitidine for two months. He had no history of diabetes mellitus and other any drug usage. Patient's laboratory results revealed white blood cells (WBCs) 18,000 mm3, monocyte %48, absolute monocyte number 8,640 mm3, hemoglobin: 8gr/dl, thrombocyte: 88,000 mm3, glucose 119 mg/dL, Lactate Dehydrogenase (LDH) 344 mg/dL total bilirubin 1.41, C-reactive protein (CRP): 5 mg/dl.
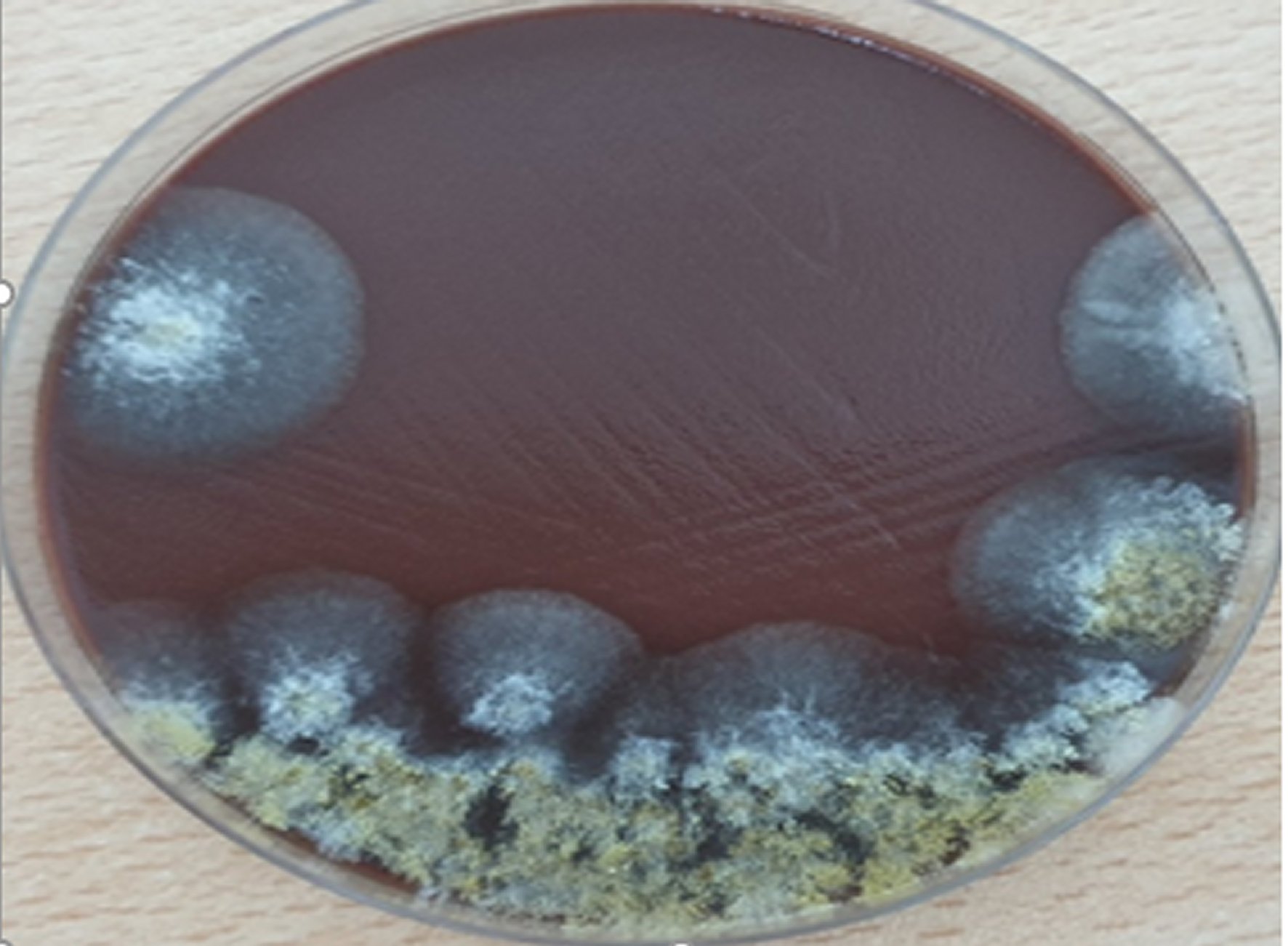
The patient was hospitalized, and he was supported with 5L/min of oxygen with nasal canula and empirically Ceftriaxone 2x1 gr/day/intravenous was started after microbiological cultures (blood, urine, sputum) were taken. A chest high resolution computerized thorax scan (HRCT) was performed. Despite the previous examination of a HRCT was normal and showed no active infection or infiltration in the lungs, which taken two months ago. A second thorax HRCT revealed a ground-glass appearance of the lung and many consolidation areas (Figure 1). These signs were due to a specific fungal infection. The (polymerase chain reaction) PCR test results for Pneumocystis jiroveci, Cytomegalovirus, and Legionella species was negative. Bronchoalveolar lavage analysis was not performed due to the patient's relatives refused this interventional procedure. Since respiratory distress increased, empirical classical Amphotericin B treatment was started according to HRCT findings. In addition, cefriaxone was stopped and empirical piperacillin tazobactam was started.
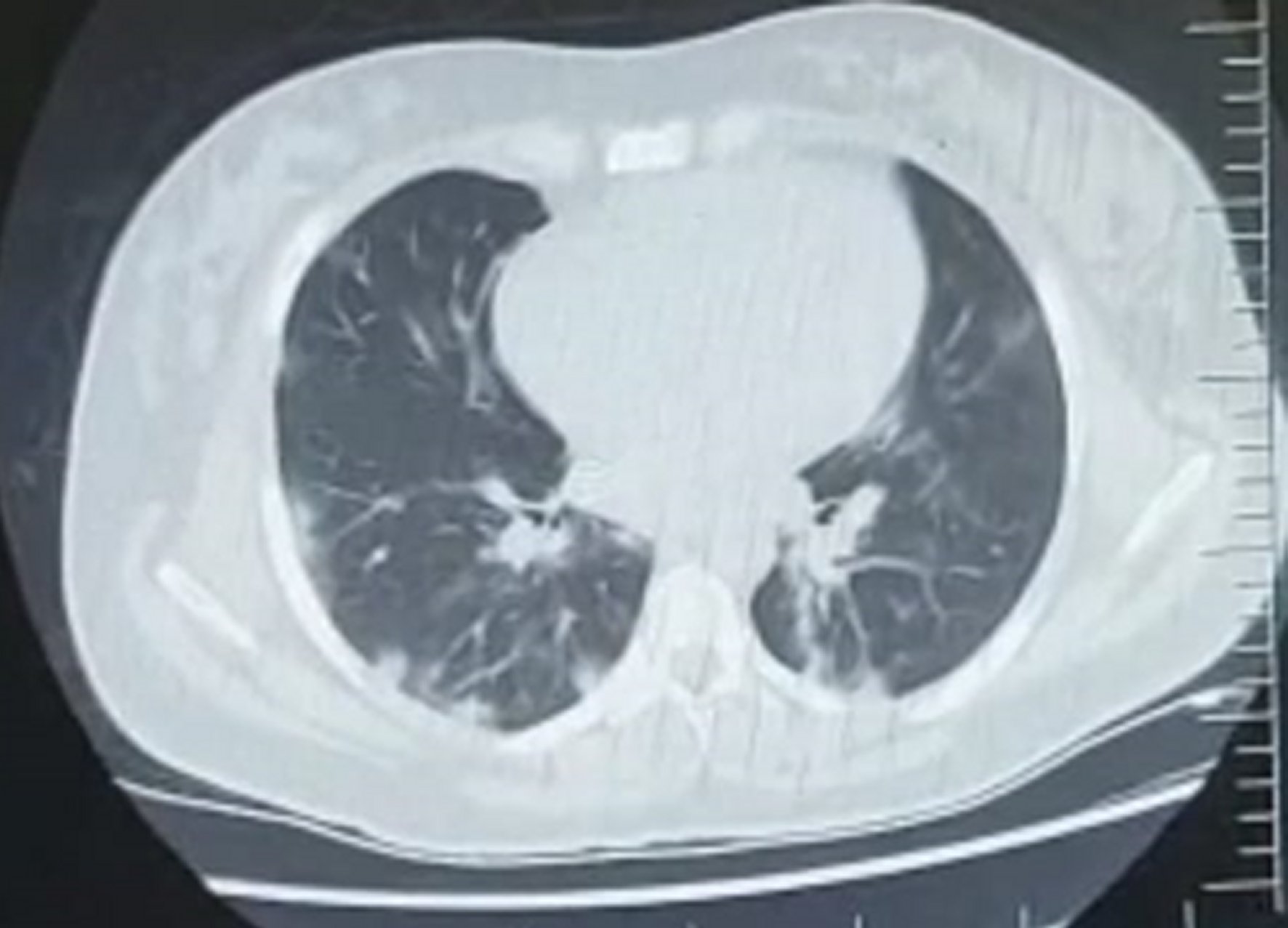
Figure 1: High resolution computerized thorax scan image. The lung bilaterally developed several large consolidations clustered from the centre hilum to the chest wall. He had a bilateral severe air bronchogram and fusiform bronchiectasis. There is also an irregularly thickening pleural on both sides of the hemithorax.
In the patient's deeper anamnesis, we learned he was using his father's home ventilator device for 3 weeks before his complaints. He used this device despite receiving any informed advice from his doctors or other medical professionals. We also learned that from hospital automation system records, he was treated with azacitidine (75 mg/m2/day) for 7 days per month and after two cycles of azacitidine treatment, the patient’s lung and other physical examination findings and laboratory parameters were normal two weeks before the hospitalization, when he come to the outpatient clinic.
The home ventilator device was brought to the hospital for further analysis. The breathing filter was examined, swab samples were taken, and a microbiological examination was performed. The organism was isolated from his father's air tube of the non-invasive ventilation device. Swap samples showed hif and cultures showed growth of a mold rapidly filling the petri dish of chocolate agar within 48 hours of incubation (Figure 2). Grown mold was identified as Mucor spp.
Even with antifungal treatment, our patient went into respiratory insufficiency and died in the 4th day of antifungal treatment.
3. DISCUSSION
Mucormycosis is an uncommonly encountered clinical syndrome in immunocompromised hematology patients. Mucormycosis is rare in both immunocompromised and immunocompetent patients [1, 2]. The most reported clinical presentations in mucormycosis are the rhinocerebral, pulmonary, and cutaneous forms (superficial) and less frequently the gastrointestinal, disseminated, and miscellaneous forms [10]. Pulmonary mucormycosis infections are most found in immunocompromised patients, such as those who are undergoing chemotherapy or chronic corticosteroid treatment. Pulmonary mucormycosis is an infection caused by the inhalation of spores causing pneumonia with the subsequent necrosis of lung tissue. This infection can also spread directly or hematogenous to surrounding structures in the mediastinum such as the heart or other organs [11]. In this study, we aimed to report an uncommon case of pulmonary mucormycosis related to the use of the home-ventilator machine.
The hematological malignancies are the most common underlying disease of mucormycosis. The patients with acute myeloid leukemia, myelodysplastic syndrome, hematopoietic stem cell transplantation and acute lymphoblastic leukemia are at higher risk of developing mucormycosis, especially in the neutropenic period [12]. The presented case had CMML but he was not at in the neutropenic period.
Azacitidine is primarily approved for the treatment of myelodysplastic syndrome. However, it is also approved for the treatment of CMML patients. It is expected to almost all patients be neutropenic in the first 1-3 cycles of azacitidine treatment. Antibiotics prophylaxis and/or G-CSF should be considered in patients requiring urgent treatment with azacitidine, to prevent hospitalization and neutropenic sepsis during the first 2 cycles [13]. However, the data on its relationship with fungal infections could not be reached. As mucormycosis is usually expected to be found after immunosuppression (such as chemotherapy or steroid treatment), but in this the reported patient, the development of this infection occurred at home without any immunosuppression. This is the interesting feature of this case.
Pulmonary mucormycosis commonly occurs in men over 55 years of age. Common clinical findings in these patients are fever, neutropenia, dyspnea, and cough [11]. The presented case was also 64-year-old male, and he did not have neutropenia, but had fever, dyspnea, and cough symptoms.
It was reported that pulmonary mucormycosis could be seen after pulmonary tuberculosis (TB) infection [12]. However, the presented case had no history of TB.
In pulmonary mucormycosis cases, pleural effusion, lung infiltration, consolidation, thickly walled cavities, multiple nodules can be detected mostly, but rarely hilar or mediastinal lymphadenopathy, air crescent sign, pneumothorax, reverse halo sign can be seen in radiological imaging [11, 12]. Radiological findings can be seen bilaterally or unilaterally, but generally radiological findings are non-specific [12]. The presented case thorax HCRT findings were a ground-glass appearance of the lung and many consolidation areas in both lungs.
There are four determining factors in the successful treatment of mucormycosis: early diagnosis, amphotericin B, surgical resection, and reversal of host impairment [1, 2]. It is reported that in addition to medical treatment, additional surgical interventions are required in the treatment of the disease. Its mortality has been reported as over 25% [11]. Our patient. He died without considering surgical treatment. The diagnosis of the patient could not be confirmed microbiologically since his relatives did not accept the invasive procedure.
Patients treated with home respirator devices are at a substantially higher risk for many infections. Patients who use these devices must be informed in detail about the device and its proper use. Additionally, all immunocompromised patients should be informed about the protection of the respiratory tract. Dirty or contaminated equipment are potential sources of infection. All devices and accessories should be cleaned regularly. The tubes should be also checked frequently to ensure that they are safely connected.