INTRODUCTION
Nosocomial infections are very common, and approximately 40% of these infections are catheter-related urinary tract infections (CAUTI) [1]. A Foley catheter, which is the most important predisposing factor of CAUTI, is used in 25% of hospitalised patients generally and almost 100% of patients in intensive care [1].
CAUTI is an important cause of morbidity and mortality in hospitalised patients [2]. It also creates a serious reason for the irrational use of antibiotics and the development of resistant microorganisms, putting other patients at risk of being infected with these resistant organisms [1, 2, 3]. CAUTI increases susceptibility to catheter occlusion in catheterised patients and predisposition to urinary system stones, including malignant transformation [1]. This susceptibility, paradoxically, also increases the risk of CAUTI [1].
The risk of CAUTI increases with each passing day with a catheter [1]. The incidence of CAUTI has been found to be similar in patients receiving intensive and nonintensive care [4]. The most important parameter to prevent CAUTI is to avoid unnecessary catheterisation; thus, it is important to evaluate all patients with a catheter [5]. Although infection control committees in hospitals have established strict follow-up protocols regarding CAUTI, if doctors and nurses have sufficient knowledge of this issue, it will help in reducing such infections [6]. In this study, we aimed to determine the compliance of healthcare personnel with urethral catheterisation standards and the factors affecting it in a rural academic hospital in Turkey.
MATERIAL AND METHODS
Ethical approval for this study was obtained from Zonguldak Bulent Ecevit University Local Ethics Committee (meeting date: 10/02/2021; meeting no: 2021/03). A questionnaire was emailed to 712 healthcare professionals (HCPs) (330 doctors at different academic levels and 382 nurses) and asked to respond after obtaining their written consent. The present research study included participants working in different departments and areas (i.e. intensive care, operating room, ward etc.) in Zonguldak Bulent Ecevit University Hospital, Zonguldak, Turkey between February and March 2021. Google Docs™ was used to prepare the survey form, as it ensured the participants' anonymity. Furthermore, the participants were informed that the results of the questionnaire would be used for scientific purposes only.
The survey questions for this present study were adapted particularly for this study from the questions prepared according to the Centers for Disease Control guidelines by Jain et al [1, 7]. The authors to ensure they reflect the knowledge and skills of the target audience and that they are simple and understandable previously evaluated the questions. Demographic data (such as age, gender, academic position, department and area of posting) of the participants were collected during the survey. The second section of the survey had 10 questions that evaluated the participants’ knowledge of the indication for catheter insertion, the third part had 15 questions that assessed their knowledge level about CAUTI prevention, and the last part had 8 questions that evaluated the general attitudes of the participants /towards CAUTI.
The participants were asked to answer questions on the indication for catheter insertion and methods of preventing CAUTI on a four-point scale. After comparing the answers with the Centers for Disease Control guidelines, the questionnaire responses were converted to binary variables before performing the analysis agreeing the method employed by Jain et al [1]. The values were expressed as follows: (4): Almost always indicated; (3): Sometimes indicated as indicated; (2): Rarely indicated; (1): Never indicated as not indicated) (4: Large effect; 3: Moderate effect as effective; 2: Some effect; 1: No effect as ineffective).
STATISTICAL METHODS
Nominal and ordinal parameters were reported as frequencies. Fischer’s exact test was used to assess the differences between the categorical parameters. Means and standard deviations were used for the description of the scale parameters. The Kolmogorov–Smirnov test was used to evaluate the normality of the scale parameters. The independent samples t-test was used for the normally distributed parameters, while the Mann–Whitney U and Kruskal–Wallis tests were used for no normally distributed parameters. All the analyses were performed using SPSS 17.0 for Windows, with a 95% confidence interval and 0.05 significance level.
RESULTS
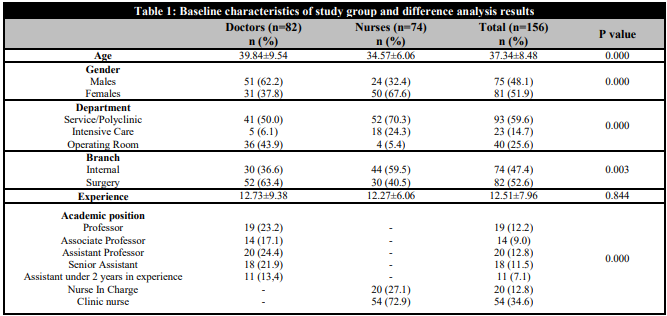
Of the 712 HCPs in the hospital, 156 (21.91%) participated in the survey. The mean age of the participants was 37.34 ± 8.48, and 48.1% of the participants were male. Of the 156 HCPs, 82 (52.6%) were doctors, while 74 (47.4%) were nurses. The baseline characteristics of the participants are summarised in Table 1.
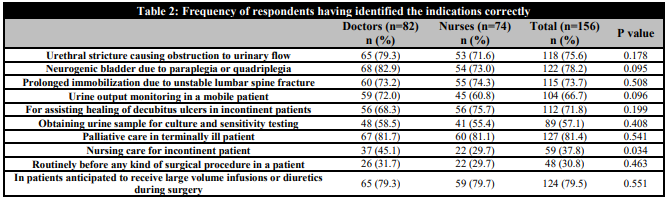
Regarding the participants’ level of knowledge of the indications for urethral catheterisation, there was a significant difference between doctors and nurses’ knowledge of nursing care for incontinent patients (p < 0.05). All answers to the other questions were statistically significant (p > 0.05) (Table 2).
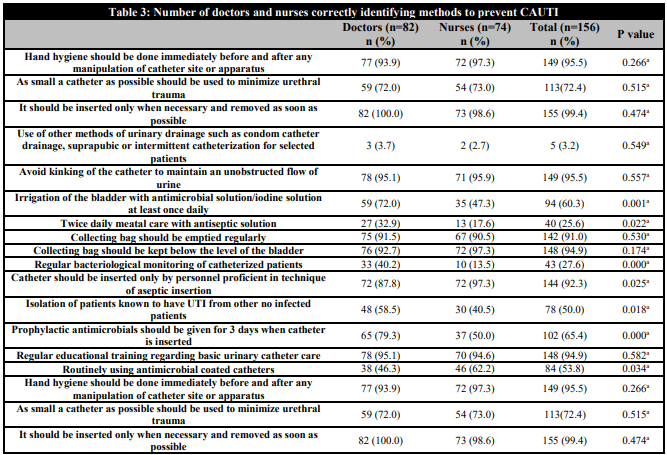
The answers given to ‘Irrigation of the bladder with an antimicrobial solution/iodine solution at least once daily’, ‘Twice daily metal care with an antiseptic solution’, ‘Regular bacteriological monitoring of catheterised patients’, ‘Catheter should be inserted only by personnel proficient in the technique of aseptic insertion’, ‘Isolation of patients known to have urinary tract infection from other no infected patients’, ‘Prophylactic antimicrobials should be given for three days when a catheter is inserted’ and ‘Routinely using antimicrobial coated catheters’ were statistically significant between the doctors and the nurses (p < 0.05). All other answers given to questions regarding indications for preventing CAUTI were not statistically different (p > 0.05) (Table 3).
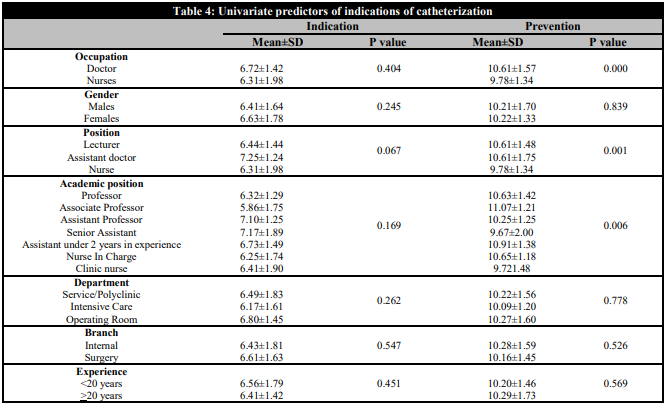
The knowledge level on indications for catheterisation was not significantly different between occupation, gender, position, department, branch and experiment groups (p > 0.05). The knowledge level on prevention of CAUTI was significantly different between occupation and academic positions (p < 0.05), with the doctors having higher scores (Table 4).
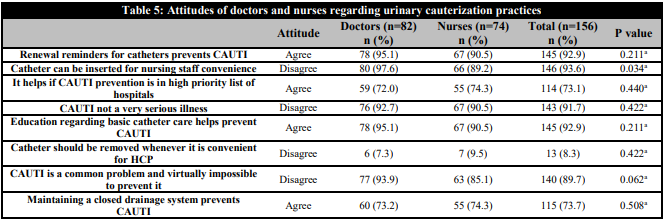
Among the questions about the attitudes of the doctors and the nurses towards urinary catheterisation practices, the answer given to the item ‘Catheter can be inserted for nursing staff convenience’ was statistically significant (p < 0.05). No significant difference was found between all other responses (p > 0.05) (Table 5).
DISCUSSION
To prevent CAUTI, the entire process from insertion to withdrawal should be followed within the framework of the guidelines. It has been shown in the literature that compliance with these rules can reduce the rate of CAUTI by almost one-third [5]. CAUTI rates are thought to be higher than actually reported [8]. Although many factors may play a role in the development of CAUTI, it is known that the most important is the duration of catheterisation. The daily risk for infective consequences is thought to be 5%–10%, which approaches 100% at the end of a monthly period [8]. However, as supported by the literature, the use of urinary catheters in hospitalised patients continues even after the indication for use has expired [1, 9]. To prevent CAUTI, which has an important place among hospital-acquired infections, it is necessary to reduce the duration of cauterisation, and HCPs should have sufficient knowledge of this [10].
It is important to determine the correct indications to prevent unnecessary catheter usage. In general, the knowledge of the doctors and the nurses was similar regarding determining the indications for catheterisation (p = 0.404). However, when the preventive methods were compared, it was observed that the level of knowledge of the doctors was higher than that of the nurses (p < 0.05). Among the nurses, it was found that nurses-in-charge have more knowledge on preventive methods. Considering that clinical nurses have a more active role in patient care, this issue draws attention. Ensuring the knowledge level of nurses is high will help in determining unnecessary catheterisation indications effectively and promote catheter hygiene while nurses are monitoring patients [1, 11, 12].
Approximately 70.3% of the nurses and 54.6% of the doctors stated that the use of a catheter might be necessary for the nursing care of patients with urinary incontinence. Although the level of knowledge of the doctors on this subject seems to be higher, they responded at a lower rate than expected. When the answers given for other indications were examined, the present study revealed that more than half of the nurses and the doctors gave similar answers.
Only one-third of the nurses and the doctors agreed on the need for routine catheter insertion before any surgery, which is more than expected. Although the current study could not show a significant difference between the knowledge levels of the nurses and the doctors of different degrees about urinary catheterisation indication in the univariate analysis, the knowledge levels of assistant professors and assistant doctors with more than two years of experience seemed to be higher in our study. This may be related to the fact that doctors at this level are constantly reviewing their knowledge. Today, where the urethral catheter is widely used, the correct approach will be to review the catheterisation indications and keep the knowledge levels of doctors and nurses up to date always.
Both physicians and nurses have largely responded favourably to the use of alternative techniques (such as condom catheter drainage, suprapubic or intermittent catheterisation) in suitable patients instead of urethral catheterisation. According to the literature, the fact that catheterisation techniques are seen as alternatives to each other in terms of CAUTI prevention can be considered in terms of preventing some complications, but it does not change the infective results [13]. In this regard, it would be beneficial to provide training that will change the perspectives of healthcare professionals.
Considering the working field and departments, we could not see a relationship among the HCPs regarding catheterisation approaches. However, Tabrisi et al., reported in their study that HCPs working in surgical wards were better in compliance with catheter care standards [8]. This difference may have been due to the study design because, while our study focused on the level of knowledge, the related study conducted an application-oriented evaluation.
One-third of the doctors and almost half of the nurses stated that irrigation of the bladder with antimicrobial solution/iodine solution at least once daily can prevent CAUTI, and 67.4% of doctors and 82.4% of the nurses stated that daily meatal care with an antiseptic solution could prevent the development of CAUTI. Furthermore, 59.8% of the doctors and 86.5% of the nurses reported that taking regular culture samples from catheterised patients is a preventive approach. As can be understood from these results, although not effective, HCPs have developed habits that can both increase health expenditure and unnecessary workload, which is consistent with the literature1. While simple precautions are sufficient, complex behaviours of HCPs can be overcome with sufficient training.
In the present study, we could not find a relationship between gender differences and the preventive measures of CAUTI. The absence of gender dominance among HCPs in our country seems to explain this situation. Professional experience did not contribute as a preventive factor, which was consistent with the literature [1, 11, 14]. While it was effective for one parameter where the information is variable, it seemed ineffective for another parameter. In light of evidence-based medicine, it is necessary to renew the knowledge of HCPs from different perspectives.
Of the HCPs, 73.1% reported that if hospitals put CAUTI on a high priority list, it could help to prevent CAUTI, and 92.2% reported that using a catheter reminder could be effective in preventing CAUTI. Although there is an effective infection control committee in our hospital, the use of a catheter reminder is not in practice. Similar problems have been reported repeatedly in the literature [1, 15, 16].
A few of the HCPs (6.4%) stated that the urethral catheter can be inserted for the convenience of the nurses, and most of those who gave this answer were nurses. Similar results have been reported in the literature [17], and people who were primarily concerned with the follow-up of catheterised patients gave this response. Such a rate does not seem surprising since nurses are competent in this regard in our hospital as well.
About 8.3% of the HCPs think that CAUTI is not a serious disease, and 10.3% think that CAUTI is an unavoidable problem. This finding is consistent with the literature [1]. In addition, 7.1% of the HCPs think that catheterisation training cannot prevent infection. About 10% of the healthcare workers have serious concerns about catheter-related infections, and perhaps this reflects their behavioural approaches.
The main limitation of this study is the small number of participants who completed the survey. The low number may be related to the fact that the internet is not a preferred tool. However, this survey further highlighted the lack of compliance of HCPs with catheterisation guidelines. Reaching the participants online was another limitation. However, our approach enabled anonymity and gave participants ample time to reflect on their answers rather than give an immediate response. Another limitation could concern obtaining data directly from individuals in this study. As there may be an incompatibility between application and knowledge, it would be more appropriate to support our finding with an observational study. Since our research was conducted in a single urban, academic medical centre, a multicenter study with large participation will enable us to reach a more reliable conclusion.
CONCLUSIONS
The present study finding revealed that the HCPs were incapable of catheter applications. In our practice also, expanding the indications for catheterization in line with patient demands and unnecessarily prolonging the duration of the catheter instead of using alternative urine collection products might be seen. It seems that education on its own is insufficient to correct this challenge. Presently, we think it would be wiser to use computer-based artificial intelligence for tracking catheterisation time, revising of urethral catheterisation indications and producing alternative products for urine collection, considering the annual costs spent for CAUTI.