A 13-year-old Caucasian boy was referred with an asymptomatic linear brown discoloration affecting his right fourth fingernail. This discoloration had been present for three months and had not changed in thickness or pigment intensity. The boy was healthy, not taking any medications, and had no personal or family history of melanoma. On examination, a linear band of brown pigment was seen extending from the eponychium to the free edge of the nail plate (Figure 1A). The rest of the mucocutaneous examination, systemic assessment, and routine laboratory investigation were normal. Dermoscopy showed a homogeneous linear pigmentation of the nail matrix visible through the translucent cuticle and proximal nail fold (pseudo-Hutchinson sign) (Figure 1B). We diagnosed longitudinal melanonychia (LM). The patient was followed for 1 year and the discoloration had not changed in thickness or pigment intensity. Despite this, both the patient and his family decided to perform complete excision of the lesion (Figure 1C). Histopathologic examination of the excision specimen was compatible with a subungual junctional melanocytic nevus (Figure 1D).
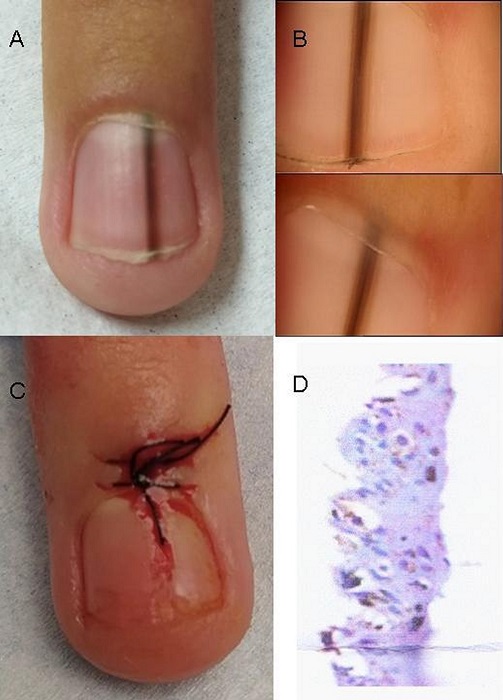
Figure 1 A) Longitudinal melanonychia of the right fourth digit of a 13-year-old boy. B) Dermoscopy image showing homogeneous brown linear pigmentation and pigment visible through the translucent cuticle and proximal nail fold (pseudo-Hutchinson sign). C) Complete removal of the nail matrix nevus. D) Detail of the histopathological characteristics in the basal and parabasal epidermis with typical nevocellular proliferation.
LM refers to a brown or brown-black longitudinal band on a fingernail or toenail [1]. LM is relatively common in African-American, Latino, and Asian patients, especially those over the age of fifty. However, it is infrequent in the Caucasian population (incidence at around 1%), and rare in children [2, 3]. LM is produced by the increased production of melanin in the nail matrix. A number of conditions can cause LM, either by activation or proliferation of melanocytes. When it results from the activation, the main etiologies are ethnic pigmentation, onychotillomania, trauma, medications, and genetic syndromes. When it is secondary to the proliferation, the main etiologies are melanocytic nevus, atypical melanocytic hyperplasia, and lentigo simplex, but its main importance is that it may indicate the presence of subungual malignant melanoma [2, 4]. While approximately 5% of LM in adults correspond to melanoma, it is normally benign in childhood, with melanocytic nevus being the major cause. However, in their early stages, benign melanonychia can share similar clinical, dermoscopic, and histopathological features with subungual melanoma [1, 2, 5]. For this reason, prolonged follow-up is recommended, since cases of melanoma of the nail apparatus have occasionally been reported in adults with a history of childhood-onset LM [5]. This can cause worry and anxiety in patients and their families [4]. Nail matrix biopsy is the gold standard for etiological diagnosis [1, 2, 5]. Considering that the incidence of subungual melanoma is extremely low in the pediatric age group (only 21 cases have been described in the literature) [1], and that nail matrix biopsy is an invasive procedure, often complicated by nail dystrophy and recurrence, and difficult to perform in children, the decision between performing clinical follow-up or biopsy is challenging [1, 2, 4, 5]. Features that should prompt histopathologic examination and that are suggestive of subungual melanoma include increased width or darkening of the lesion, variegated pigmentation, periungual pigmentation, or nail plate dystrophy. The pseudo-Hutchinson sign corresponds to the pigmentation of the nail matrix visible through the cuticle, thus not being a true warning sign. This is distinguished from Hutchinson sign, in which the extension of brown-black pigment onto the adjacent cuticle and nail folds is suggestive of subungual melanoma [1, 2, 5]. In the present case, the decision of the patient and his family to perform the complete excision was to determine the histopathological diagnosis, in order to avoid evolutionary uncertainty and periodic check-ups. In conclusion, LM in pediatric patients represents a challenging diagnosis and clinical management strategy.














