Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Enfermería Global
versión On-line ISSN 1695-6141
Enferm. glob. vol.18 no.55 Murcia jul. 2019 Epub 21-Oct-2019
https://dx.doi.org/10.6018/eglobal.18.3.328791
Originals
Postoperative complications related to intraoperative hypothermia
1Nurse. Master's degree in Nursing, School of Nursing, Federal University of Minas Gerais. PhD student in the Graduate Program in Nursing, School of Nursing, Federal University of Minas Gerais, Belo Horizonte (MG), Brazil. nathaib@hotmail.com
2Nurse. PhD in Nursing from the University of São Paulo. Associate Professor, Department of Basic Nursing, School of Nursing, Federal University of Minas Gerais, Belo Horizonte, State of Minas Gerais, Brazil.
Introduction
Hypothermia is a common event in the intraoperative period, it triggers consequences in the recovery of the patient, with complications in several systems of the organism, such as cardiac, respiratory, integumentary, digestive, immunological and also the coagulation system.
Objective
To analyze the complications presented by the patient in the postoperative period related to intraoperative hypothermia.
Methods
A retrospective cohort study was carried out in a sample composed of 54 patients' files, from a previous experimental study, in which they were submitted or not to warmed intraoperative intravenous infusion and anesthetic recovery. The variables were analyzed at 4 different times, upon arrival at the hospitalization unit, after 17, 32 and 108 hours postoperative. The model used was the marginal logistics.
Results
The majority of patients 40 (74.07%) were female, mean age of 47.06 years, 42 (77.78%) were normothermic patients from the Post Anesthesia Recovery Room, with a mean temperature of 36.2ºC. Regarding the comparison between variables and groups of normothermic and hypothermic patients, over time, the variables that presented statistical significance were the time of hospitalization, pain, nausea, evacuation and surgical wound with presence of secretion, with a p-value less than 0.05.
Conclusion
In view of the complications found in this study, it is necessary to develop preventive and control actions for intraoperative hypothermia aiming at a better recovery of the patient in the postoperative period.
Key words: Hypothermia; Postoperative Complications; Perioperative Nursing
INTRODUCTION
Hypothermia is considered to be a body temperature lower than 36°C, being that a common event, affects 70 to 90% of the patients submitted to the anesthetic-surgical procedure, which may lead to relevant complications1,2.
The surgical center is an environment conducive to the development of hypothermia due to the association between the low temperature of the operating room (OR), the performance of antisepsis of the skin of the patient with the body discovered, the infusion of cold solutions during the procedure, inhalation of cold gases, open cavities or wounds, and the use of anesthetic drugs that alter the mechanism of thermoregulation, inhibit tremors and produce peripheral vasodilation3.
The way by which the organism sets normal limits of temperature is not yet clear, but it is known that several endogenous substances such as norepinephrine, dopamine, serotonin, acetylcholine, prostaglandin E1 and neuropeptides, and also some additional factors such as circadian rhythm, exercise , food intake, infection, thyroid dysfunction, menstrual cycle, anesthetics and other drugs, are known to alter temperature thresholds4.
The rate of enzymatic reactions of the organism, during the metabolism of the compounds administered during anesthesia can be altered, directly affecting the action duration of general anesthetics. Hypothermia is responsible for prolonging the action of most non-depolarizing relaxants and affecting the pharmacodynamics of depolarizing agents. A decrease in body temperature at 3°C below the normal value prolongs the relaxation time by about 60%. In addition, hypothermia changes the action characteristics of inhalational anesthetics, increasing their solubility in the tissues, resulting in the increase of the anesthetic content in the body. Opioid analgesics have also shown prolonged action in hypothermia, which is associated with an increase in plasma concentration on average by 25% compared to normothermia4.
Perioperative nursing seeks the quality of care and safety of the surgical patient. Therefore, the knowledge about the clinical manifestations and the complications of the adverse events resulting from the anesthetic-surgical procedure is essential for the elaboration of effective intervention plans5.
Thus, in view of the complications triggered by intraoperative hypothermia, the following questions arise: what are the postoperative complications presented by the patient related to intraoperative hypothermia? Is there a difference in the complications presented by the patients who left hypothermic and those who left normothermic from the Post Anesthesia Care Unit (PACU)?
The objective of this study was to analyze the complications presented by the patient in the postoperative period related to intraoperative hypothermia.
METHODS
Type and location of study
This is a retrospective cohort study, carried out in a large public university hospital.
The surgical center has 16 operating rooms, with a monthly average of 1,600 surgeries, among them elective and emergency surgeries. The PACU has eight beds and maintains the ambient temperature between 22°C and 24°C and relative humidity between 45 and 60%, according to the recommendations of the Ministry of Health.
Population and sample
Data were obtained retrospectively from the medical charts of 60 patients who participated in a previous experimental study, whose objective was to verify the efficacy of a warmed intravenous infusion in the prevention of hypothermia in patients during the intraoperative period. The results of this research allowed us to conclude that the use of intravenous warmed infusion alone in patients during the intraoperative period does not prevent hypothermia. The operating room temperature at the patient's entrance and the patient's temperature at the entrance to the operating room were statistically significant to influence the occurrence of hypothermia6.
All the available medical records were included, so the sample consisted of 54 medical records of the subjects who participated in the previous study. There were 6 medical records lost, which were not found.
Inclusion and exclusion criteria of the sample
The inclusion criteria of the sample were, being an adult with ages ranging from 18 to 85 years, elective surgical procedure with conventional or minimal abdominal surgical access, general anesthesia, anesthetic time of at least one hour, American Society of Anesthesiologists (ASA) I to III, and axillary body temperature upon entering the OP between 36ºC and 37.1ºC .
Patients with predisposition to temperature changes such as thyroid and neurological disorders, weight extremes, ASA IV to VI classification, and axillary body temperature below 36°C or higher than 37.1 ° C, were excluded.
Ethical aspects
The research project was approved by the Research Ethics Committee of the Minas Gerais Federal University (UFMG), CAAE 43451815.6.0000.5149, in compliance with the Resolution 466/2012 of the National Health Council.
As it was secondary data, there was a release of the Informed Consent Form.
Data collection and Analysis
The data was collected from April to June 2015, through the patients' medical charts.
In order to collect the data on the complications presented by the patients in the postoperative period, a structured instrument was elaborated, containing data related to vital signs changes, being Temperature (T), Heart Rate (HR), Respiratory Rate (RR), blood Pressure (BP) and pain, urinary, bowel and flatus elimination, nausea, vomiting, changes in appetite and sleep, bleeding, and phlogistic signs in Surgical Wounds (SW).
The database was composed of 11 characterizing variables and 14 variables that change over time.
For the analysis, arterial hypotension or hypertension at 20% lower or higher BP, respectively, were considered than the BP measured in the preanesthetic period, HR for bradycardia less than 60 beats per minute (bpm) and HR for tachycardia greater than 100 bpm and normal RR between 12 and 22 respiratory incursions per minute (ripm)7.
Regarding the variables pain, nausea, vomiting, diuresis, evacuation, flatulence, insomnia, inappetence and bleeding, the presence or absence of these variables were verified, and if there were devices which would give propensity of the event such as Straight catheter (SC), Nasoenteric Tube (NET) and Nephrostomy.
The SW variable was evaluated according to the appearance of the surgical wound, that is, if the appearance was clean/dry, if there was presence of local heat/hyperemia or if there was any secretion.
To compare the variables between the groups related to temperature (Hypothermic and Normothermic) over time, marginal models were adjusted. The variables were treated as categorical dichotomous, considering as a response variable the most frequent category. In this way, the model used was the marginal logistics.
To compare the groups over time, 4 different times were considered. These times were chosen based on the quartiles of the hospitalization time: the baseline is zero time, in other words, the arrival in the Inpatient Unit (IPU), the first quartile equals 17 hours of hospitalization, the second quartile equals 32 hours of hospitalization and the third quartile equals 108 hours of hospitalization.
RESULTS
The presentation of the results was performed according to the sociodemographic and clinical characterization of the patients, analysis of the complications presented during the period of postoperative hospitalization and comparison between the normothermic and hypothermic patients in relation to the presented complications.
Sociodemographic and clinical characterization of patients
The majority of the patients were female, 40 (74.07%), mean age 47.06 years, with a standard deviation of 14.96 and ASA score equal to II, 32 (59.26%).
The most frequent comorbidities were Systemic Arterial Hypertension (SAH) with 18 (56.25%) patients, followed by Diabetes Mellitus (DM) with 4 (12.50%) patients.
The most common medical diagnoses were Cholecystitis due to Cholelithiasis with 7 (12.96%), followed by female infertility with 6 (11.11%), and the surgical specialty was Digestive System Surgery (DSS) with 28 patients (51, 85%), followed by Gynecological Surgery with 16 (29,63
The systolic BP in the preoperative period was verified as a characterizing variable, to serve as a parameter for the analysis of its alterations during the period of hospitalization. It had an average of 124.8 mmHg (100-150).
Analysis of the complications presented during the postoperative period
In these results, 13 (24.09%) patients were discharged with up to 17.33 hours of hospitalization, 27 (50.00%) with up to 32.25 hours of hospitalization and 49 (90.74%) patients had hospitalization time less than 167 hours.
The "n" refers to the number of measures over time, thus obtaining, BP (n = 475), HR (n = 473), RR (n = 467), temperature (n = 470), pain (n = 478), flatulence (n = 478), nausea (n = 478), vomiting (n = 478), diuresis (n = 478), bleeding (n = 478), and SW (n=281), as shown in Table 1.
Table 1. Distribution of the frequency of the variables throughout the time of postoperative hospitalization. Belo Horizonte (MG), 2015.

SC:Straight catheter
IC:Indwelling catheter
NET:Nasoenteral tube
In the analysis of the vital signs, it has been noted that over time, the mean systolic BP was 118.9 mmHg (70-180), the mean HR of 79.8, with standard deviation equal to 13.1, mean RR of 19.7 irpm (15-26), and the mean T was 36.4°C, with a standard deviation of 0.5ºC.
It is observed that over time, 64 (13.62%) of the measurements (n = 480), patients were hypothermic. Regarding the evaluation of pain 95 (19.87%) (n = 478) was present. The presence of SW secretion was verified in 37 (13.40%) of the cases (n = 281).
Comparison between normothermic and hypothermic patients in relation to the complications presented
Of the 54 patient’s medical charts analyzed, 42 (77.78%) left normothermic and 12 (22.22%) hypothermic from the PACU. The mean temperature at the time of discharge from the PACU was 36.2°C with a standard deviation of 0.5°C.
For the comparison of the results of normothermic and hypothermic patients were considered 4 distinct times, which were chosen based on the quartiles of the hospitalization time, time zero on arrival in the Inpatient Unit (IPU), the first quartile equals 17 hours of hospitalization, the second quartile equals 32 hours of hospitalization and the third quartile equals 108 hours of hospitalization.
Table 2 refers to the time of hospitalization of normothermic and hypothermic patients. Patients who presented hypothermia at least once were classified as hypothermic. There was a significant difference (p = 0.024) in the hospitalization time between the groups, being that of the hypothermic patients, 30 (55.56%), had a longer stay with a mean time of 84.60 hours.
Table 2. Comparison between hypothermic and normothermic patients, according to length of hospital stay. Belo Horizonte (MG), 2015.
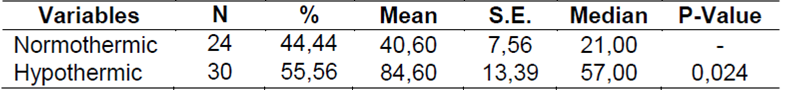
D.E.:Standard Error
As regards to the analysis of BP, HR, RR, vomiting, diuresis, flatus, insomnia, inappetence and bleeding, the groups of normothermic and hypothermic patients were homogeneous.
In the variables pain, nausea, evacuation and surgical wound, the groups were heterogeneous.
Table 3 shows the groups that were heterogeneous in relation to the percentage of patients without pain on arrival at IPU (p = 0.026), being that on arrival at IPU the chance of not having pain in the normothermia group was 3.57 times the chance in the group hypothermia.
Table 3. Comparison between hypothermic and normothermic patients, according to the presentation of pain, throughout the hospitalization time. Belo Horizonte (MG), 2015.
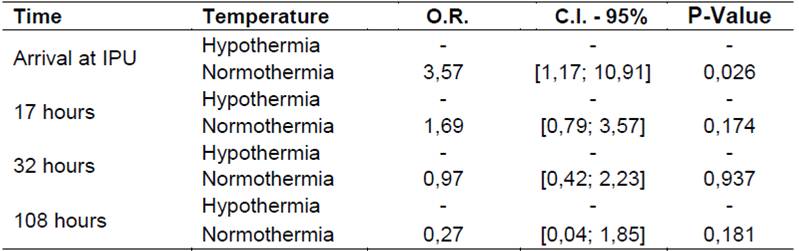
IPU:Inpatient UnitO.R.: Odds RatioC.I.: Confidence Interval
In the nausea’s analysis the category "absent" was considered as response variable. The effects of time and temperature on nausea are presented in Table 4. The groups of patients with hypothermia and normothermia were not homogeneous in relation to the percentage of patients without nausea at the time of arrival at IPU (p = 0.002), 17 hours ( p = 0.001) and 32 hours (p = 0.006), being that on arrival at IPU, the odds of not having nausea in the normothermia group were 5.14 times that of the group with hypothermia, where as in 17 hours the odds of normothermia group were 3.51 times that of the group with hypothermia and in 32 hours the odds of the normothermia group were 2.50 times that of the hypothermic group. At 108 hours, the groups were homogeneous in relation to the percentage of patients without nausea.
Table 4. Comparison between hypothermic and normothermic patients, according to the presentation of nausea, throughout the hospitalization time. Belo Horizonte (MG), 2015.

IPU:Inpatient UnitO.R.: Odds RatioC.I.: Confidence Interval
Table 5 shows the effects of time and temperature on the absence of evacuation. There was no homogeneity between the groups in relation to the percentage of patients without evacuation at the time of arrival at IPU (p = 0.024) and at 17 hours (p = 0.035), and at the time of arrival at IPU and at 17 hours, the chance of not evacuating in the normothermia group was equal to 0.13 times and 0.23 times respectively, the chance of the group with hypothermia.
Table 5. Comparison between hypothermic and normothermic patients, according to the presentation of evacuation, throughout the hospitalization time. Belo Horizonte (MG), 2015.

IPU:Inpatient UnitO.R.: Odds RatioC.I.: Confidence Interval
Table 6 shows the comparison of the SW between the groups through the marginal logistic regression method.
Table 6. Comparison between hypothermic and normothermic patients, according to operative wound conditions, throughout hospitalization time. Belo Horizonte (MG), 2015.
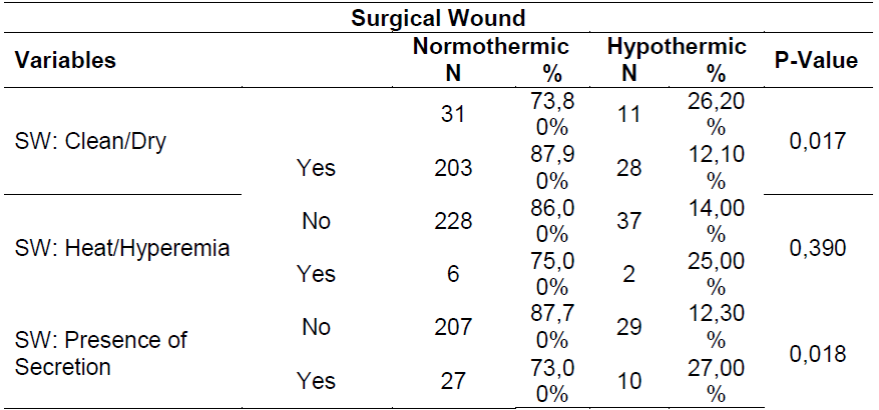
SW.:Surgical Wound
In the SW model, the variables "clean/dry", "heat / hyperemia" and "secretion present" Were considered.
There was statistical significance in the clean/dry SW variables (p = 0.017) and SW with prexence of secretion (p=0.018).
From the evaluations of the hypothermic patients, in the classification of clean/dry SW, 11 (26.20%) SW were not clean/dry, and SW with presence of secretion, 10 (27.00%).
DISCUSSION
Regarding the sociodemographic and clinical aspects, in this study the gender with the highest frequency was female, this is justified by the fact that one of the most frequent medical diagnoses was female infertility.
Studies indicate that females are more likely to develop hypothermia because women have less muscle mass and higher body surface index, leading to greater heat loss to the environment1,8.
The mean age was 47.06 years and the most frequent ASA classification was II. Older patients with higher ASA scores are at increased risk for developing hypothermia8.
The most common comorbidities were SAH and DM. One study demonstrated that diabetic patients with no target organ damage submitted to elective surgeries were less likely to develop hypothermia and associated to this fact was the improvement of the quality of follow-up protocols for diabetic patients, providing better medical practice and improvements in the general state of health of patients with diabetes9.
The most frequent medical diagnoses were cholecystitis due to cholelithiasis, followed by female infertility, in this way, the most frequent surgical specialties were DSS, followed by Gynecological Surgery. Studies have shown that surgery in the abdominal cavity predisposes the development of hypothermia10.
A study on the occurrence and factors associated with intraoperative hypothermia of elective abdominal surgeries demonstrated that at the end of the anesthetic procedure, 93 (88.6%) patients had hypothermia with a minimum value of 31.4ºC5.
In the analysis comparing the normothermic and hypothermic patients regarding complications presented during the postoperative hospital stay, were statistically significant, the length of hospitalization, pain, nausea, lack of evacuation and conditions of SW.
The hospitalization time, when compared between normothermic and hypothermic patients, was statistically significant (p = 0.024), that is, hypothermic patients had longer hospitalization time compared to normothermic patients. This finding is confirmed in the literature, in which it is mentioned that hypothermic patients present an increase in the infection rate, providing a delay in the removal of SW sutures and consequently, these factors generate an increase of approximately 20% in the time of hospital stay11,12.
When we analyzed the patients' hospitalization time, 50.00% of the patients were discharged with 32.25 hours of postoperative period. When comparing the hospitalization time of the group of normothermic and hypothermic patients, it was observed that hypothermic patients had longer hospitalization, with a mean of 84.60 hours.
These results are corroborated by a study which concluded that normothermic patients had shorter hospital stay, spent 43% less time in ICU and were discharged from the hospital with 40% of the time of hypothermic patients13.
In a study, the authors report that there are major concerns in patients undergoing general anesthesia and surgical procedures, because it can increase patient discomfort, higher complication rates, delayed hospital discharge and increased care costs14.
Scarce are the recent studies that relate perioperative hypothermia with discomforts such as pain, nausea, vomiting, evacuation, inappetence and insomnia.
In the pain variable, the groups were heterogeneous, with statistical significance (p = 0.026), on arrival at IPU, demonstrating that hypothermic patients had a greater chance of developing pain in the first postoperative hours.
This result reinforces the need for the application of preventive measures to avoid the development of intraoperative hypothermia. The level of postoperative pain is significantly reduced with the application of two hours of warm-up after surgery15.
The presence of nausea was also statistically significant (p = 0.002, 0.001 and 0.006), on arrival at IPU, 17 hours and 32 hours, respectively. Hypothermic patients were more likely to develop nausea. Nausea and vomiting in the postoperative period has a high incidence ranging from 20 to 30% after general anesthesia, and these values may reach 70% in high-risk patients16.
Although the presence of diuresis was not statistically significant between the groups, one study concluded that mild hypothermia causes increased diuresis due to inhibition of renal tubular sodium reabsorption and peripheral vasoconstriction increases glomerular filtration, and when moderate hypothermia is present, diuresis is reduced by hypoperfusion, leading to the secretion of renin and may lead to the appearance of acute tubular necrosis17.
The absence of evacuation was statistically significant (p = 0.024 and 0.035). Although no evacuation was expected in the first few hours of the postoperative period, hypothermic patients had more evacuation events on arrival at IPU and at 17 hours. The comparison between groups in relation to the presence of flatus did not present statistical significance.
An experimental study found that the administration of ghrelin in the postoperative period accelerates the rate of gastric emptying and reduces the time for the onset of bowel movements18.
The inappetence variable was not statistically significant between normothermic and hypothermic patients. A common problem after abdominal surgeries is the postoperative ileus, a pathology in which the gastrointestinal tract motility is delayed for reasons not yet understood. Satiety is associated with gastric volume, rapid gastric emptying, and motility of the upper gastrointestinal tract19.
The groups were homogeneous in relation to insomnia. A study performed in patients undergoing cardiac surgery, showed that noise in the hospital environment is an important factor in causing discomfort and anxiety to the patient and the main physiological responses related to noise were insomnia, tachycardia and fatigue20.
Regarding the variable bleeding, there was no statistical significance, only one patient presented vaginal bleeding. Studies indicate that the reduced temperature affects the coagulation process in several phases: it impairs platelet function, prolongs prothrombin time and partial thromboplastin in proportion to the extent of the temperature reduction by reducing the activity of the enzymatic processes, and consequently increases the coagulation time. Detection of the above changes under clinical conditions is very difficult because all coagulation tests are performed in the laboratory at 37°C, which does not reflect the actual image4.
The comparison between the groups of normothermic and hypothermic patients with respect to the aspect of the surgical wound, it was observed that hypothermic patients had a lower chance of having a clean/dry wound and a higher chance of having an surgical wound with some type of secretion and covered with dirt.
The healing process of SW is affected by the occurrence of hypothermia due to the fact that immune defense cells are altered by the reduction of temperature and also by the reduced supply of tissue oxygen due to vasoconstriction induced by hypothermia21. One study describes that the manifestation of hypothermia is directly related to numerous patient disorders, including SW infection3.
In this study sample size can be considered as being a limitation, a fact that reduces the possibilities of generalizations for other populations. However, methodological rigor and statistical analysis ensured the reliability of the results.
CONCLUSION
Postoperative complications related to hypothermia are common complications in the postoperative period and this study evidenced some of them.
Hypothermic patients had longer hospitalization, greater chance of developing pain, nausea, evacuation present on arrival at the Inpatient Unit, and surgical wound with presence of some secretion.
Hypothermia entails numerous complications from the moment it is installed in the individual, either in the intraoperative period, or in the postoperative period. In view of the complications found in this study, it is necessary to develop preventive and control actions for pre and intraoperative hypothermia, aiming at a better recovery of the patient in the postoperative period.
REFERENCIAS
1. American Society Perianesthesia Nurses (ASPAN). Clinical guideline of the prevention unplanned perioperative hypothermia. J Perianesth Nurs. 2001 [cited 2016 May12];16(5): 305-314. Available from: http://or.org/pdf/HYPOTHERMIA_GUIDELINE10-02.pdf [ Links ]
2. Torossian A, Bräuer A, Höcker J, Bein B, Wulf H, Horn EP. Preventing inadvertent perioperative hypothermia. Dtsch Arztebl. 2015 [cited 2017 May 12];112(10): 166-172. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4383851/pdf/Dtsch_Arztebl_Int-112-0166.pdf [ Links ]
3. Silva AB, Peniche ACG. Hipotermia perioperatória e aumento de infecção da ferida cirúrgica: estudo bibliográfico. Einstein 2014 [citado 2016 abr 13];12(4):512-517. Disponível em: http://www.scielo.br/scielo.php?pid=S1679-45082014000400513&script=sci_arttext&tlng=pt [ Links ]
4. Horosz B, Malec-Milewska M. Inadvertent intraoperative hypothermia. Anaesthesiology Intensive Therapy. 2013 [cited 2016 Apr 10];45(1):38-43. Available from: https://www.ncbi.nlm.nih.gov/pubmed/23572308 [ Links ]
5. Prado CBC, Barichello E, Pires PS, Haas VJ, Barbosa MH. Ocorrência e fatores associados à hipotermia no intraoperatório de cirurgias abdominais eletivas. Acta paul enferm. 2015 [citado 2018 abr 13];28(5): 475-481. Disponível em: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S0103-21002015000500475&lng=en [ Links ]
6. Mattia AL, Barbosa MH, Freitas Filho JPA, Rocha AM, Pereira NHC. Infusão venosa aquecida no controle da hipotermia no período intraoperatório. Rev Latino-Am Enfermagem. 2013 [citado 2017 out 03];21(3):[08 telas]. Disponível em: http://www.scielo.br/pdf/rlae/v21n3/pt_0104-1169-rlae-21-03-0803.pdf [ Links ]
7. Potter PA, Perry AG, Hall AM, Stockert PA. Fundamentos de Enfermagem. Rio de Janeiro: Elsevier, 8ªed, 2013. [ Links ]
8. Monzón Castillo CG, Candida Arana CA, Marroquín Valz HA, Aguilar Rodríguez F, Benavides Mejía JJ, Alvarez Gómez JA. Manejo de la temperatura en el perioperatorio y frecuencia de hipotermia inadvertida en un hospital general. Rev Colomb Anestesiol. 2013 [citado 2016 abr. 12];41(2):97-103.Disponible em: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-33472013000200004&lng=en&nrm=iso&tlng=es [ Links ]
9. Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC Jr. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery. 2014[cited 2016 Apr 12];156(5): 1245-1252. Available from: http://www.surgjournal.com/article/S0039-6060(14)00194-9/pdf [ Links ]
10. Tanaka N, Ohno Y, Hori M, Utada M, Ito K, Suzuki T. A randomised controlled trial of the resistive heating blanket versus the convective warming system for preventing hypothermia during major abdominal surgery. J Perioper Pract. 2013 [cited 2016 Apr 12]; 23(4):82-6. Available from: https://pdfs.semanticscholar.org/a86f/42c62c6a2e101574654d44b60fb240424849.pdf [ Links ]
11. Sessler DI. Temperature monitoring: the consequences and prevention of mild perioperative hypothermia. South Afr J Anaesth Anal. 2014 [cited 2016 Apr 12]; 20(1);25-31. Available from: https://www.tandfonline.com/doi/pdf/10.1080/22201173.2014.10844560 [ Links ]
12. Luís C, Moreno C, Silva A, Páscoa R, Abelha, F. Inadvertent postoperative hypothermia at post-anesthesia care unit: incidence, predictors and outcome. Open J Anesthesiol. 2012 [cited 2016 Apr 12]; 2(5):205-13. Available from: https://pdfs.semanticscholar.org/512d/d4428cca5a68a1d1ecaad7bda97c87720bef.pdf [ Links ]
13. Good KK, Verble JA, Secrest J, Norwood BR. Postoperative hypothermia - the chilling consequences. AORN Journal.2006 [cited 2017 May 10];83(5):1055-1066. Available from: https://aornjournal.onlinelibrary.wiley.com/doi/epdf/10.1016/S0001-2092%2806%2960116-6 [ Links ]
14. Kim SH, Oh CS, Yoon TG, Cho MJ, Yang JH, Yi HR. Total intravenous anaesthesia with high-dose remifentanil does not aggravate postoperative nausea and vomiting and pain, compared with low-dose remifentanil: a double-blind and randomized trial. The Scientific World Journal. 2014 [cited 2017 Apr 12]; 2014. Available form: https://www.hindawi.com/journals/tswj/2014/724753/cta/ [ Links ]
15. Melling AC, Ali B, Scott EM, Leaper D. Effects of preoperative warming on the incidence of wound infection after clean surgery: a randomized controlled trial. Lancet. 2001 [cited 2016 May 12]; 358(9285): 876-880. Available from: http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(01)06071-8.pdf [ Links ]
16. Wengritzky R, Mettho T, Myles PS, Burke J, Kakos A. Development and validation of a postoperative nausea and vomiting intensity scale. Br J Anaesth. 2010 [cites 2016 May 10]; 104(2):158-166. Available from: http://bjanaesthesia.org/article/S0007-0912(17)34625-1/pdf [ Links ]
17. Crisóstomo MM, Hernández AL, Ordóñez G, Riera C. La hipotermia y sus efectos durante la anestesia em niños. Rev Mex Pediatr. 2011 [citado 2016 mar 10]; 78(4):131-138. Disponible en: http://www.medigraphic.com/pdfs/pediat/sp-2011/sp114b.pdf [ Links ]
18. Falkén Y, Webb DL, Abraham-Nordling M, Kressner U, Hellström PM, Näslund E. Intravenous ghrelin accelerates postoperative gastric emptying and time to first bowel movement in humans. Neurogast & Motility. 2013 [cited 2016 May 10]; 25(6):474-e364. Available from: https://onlinelibrary.wiley.com/doi/pdf/10.1111/nmo.12098 [ Links ]
19. Mans E, Prat MS, Palomera E, Suñol X, Clavé P. Sleeve gastrectomy effects on hunger, satiation, and gastrointestinal hormone and motility responses after a liquid meal test. Am J Clin Nutr. 2015 [cited 2016 Oct 20]; 102(3):540-547. Available from: https://academic.oup.com/ajcn/article/102/3/540/4564278 [ Links ]
20. Hsu SM, Ko WJ, Liao WC, Huang SJ, Chen RJ, Li CY, Hwang SL. Associations of exposure to noise with physiological and psychological outcomes among post-cardiac surgery patiants in ICUs. Clinics (São Paulo) 2010. [cited 2016 Oct 20];65(10):985-989. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2972598/ [ Links ]
21. Qadan M, Gardner SA, Vitale DS, Lominadze D, Joshua IG, Polk HC Jr. Hypothermia and surgery: immunologic mechanisms for current practice. Ann Surg. 2009 [cited 2016 Oct 20];250(1):134-140. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2811072/ [ Links ]
Received: April 20, 2018; Accepted: August 07, 2018











 texto en
texto en 


