INTRODUCTION
Prostate cancer (PCa) is a most important medical, scientific and public health problem. Worldwide, PCa is the fifth leading cause of cancer deaths and the second most commonly diagnosed cancer in men [1, 2]. PCa is especially prevalent in North America, Northern and Western Europe and Australia [3].
The survival rate is depends on the stage reached at diagnosis, hence early-stage diagnosis using effective diagnostic tools is a key to reducing mortality due to PCa [4]. It is widely acknowledged that screening and early diagnosis of PCa are of vital importance for improving the likelihood of recovery. However, such biomarkers as serum prostate-specific antigen (PSA), and its precursor have not withstood the challenges of providing sensitivity and specificity. Moreover, the PSA screening of PCa has some other significant disadvantages.
Firstly, reliance on PSA testing can result in significant over-detection of alleged PCa and hence inappropriate treatment of non-malignant disease [5]. Nearly 70-75% of prostate biopsies fail to detect PCa in men who undergo prostate biopsy due to elevated PSA levels [4, 6]. In other words, it has been confirmed that only 25-30% of patients with a PSA value ≥ 4 ng/mL were finally diagnosed with PCa, leading to the over‑treatment of low‑risk patients, unnecessary biopsies and nonessential radical prostatectomies [7]. Secondly, the PSA test misses some aggressive tumors. Data from many research shows that only 20-40% of patients with PCa have an abnormal PSA level [5, 8, 9].
The limitations and potential harm associated with PSA screening stimulate investigation of novel biomarkers with superior ability to detect PCa. Other relevant factors of great significance for any novel method of PCa detection include a minimally invasive procedure, cost-effectiveness, capacity to generate real-time results, “simplicity-of-use”, robustness, and functionality without excessive prior-processing of samples [10].
In our previous studies the significant role of Zn and some other trace elements (TEs) in prostatic function was studied in detail for both normal and pathophysiological glands [11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31]. One of the main functions of this gland is the production of prostatic fluid [32]. It contains a high level of Zn and some other TEs, in comparison with their concentrations in prostate tissue, blood serum and other human body fluids.
The first finding of remarkably high levels of Zn in human expressed prostatic fluid (Zn in EPF) was reported in the early 1960s [33]. After this finding several investigators suggested that the measurement of Zn in EPF may be useful as a marker of abnormal prostate secretory function [34, 35]. This suggestion promoted more detailed studies of the Zn in EPF of apparently healthy subjects and in those with different prostatic diseases, including chronic prostatitis, benign prostate hyperplasia and PCa [35, 36, 37]. A detailed review of these studies was given in our earlier publication [36]. Moreover, the method and apparatus for micro analysis of Zn and some other TEs in the EPF samples using energy dispersive X-ray fluorescence (EDXRF) activated by radiation from the radionuclide source 109Cd (109Cd EDXRF) was developed by us [38]. It was found that data on changes of TE content and, particularly, Zn in EPF of patients with PCa are very important, because these significant changes increase our knowledge and recognition of PCa pathogenesis and may prove useful as PCa diagnostic markers [39, 40, 41, 42, 43, 44, 45, 46, 47]. It was concluded that the Zn in EPF, obtained by EDXRF, is a first candidate with the role of offering a new, simple, fast, reliable, and non-invasive diagnostic tool for PCa population screening [47].
However, it was reported about the association between sexual dysfunctions and such diseases as asymptomatic cancer, cardio-vascular conditions and some chronic illnesses [48, 49]. Because, the prostate gland is involved in a man’s reproductive function it was unclear how non-prostatic diseases inherent of the old persons, including heart diseases, atherosclerosis, diabetes, asymptomatic cancer of different localization and some others, impact on the Zn in EPF. The information on subject is very important for using of the Zn in EPF in population screening for PCa.
To study this issue, we performed the Zn level determination in EPF of patients with bladder cancer (BC). All studies were approved by the Ethical Committees of the Medical Radiological Research Centre (MRRC), Obninsk. All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments, or with comparable ethical standards.
MATERIALS AND METHODS
SAMPLES
Specimens of EPF were obtained from 17 patients with bladder cancer (mean age 51±12 years, range 38-77 years) and from 51 men with apparently normal prostates (control group, mean age ± Standard Deviation - 51±16 years, range 18-82 years) in the Urological Department of the Medical Radiological Research Centre (MRRC) using a standard rectal massage procedure. The diagnosis of each prostate and bladder condition was made by qualified urologists. The BC stage ranged from T1N0M0 to T3N0M0 and prostate glands were intact. In all cases the N classification of prostate were confirmed by clinical examination and by cytological and bacteriological investigations of the EPF samples. The diagnosis of BC had been confirmed by clinical examination and morphological results obtained during studies of biopsy and resected materials. Healthy subjects were asked to abstain from sexual intercourse for three days preceding the procedure.
Thus, the inclusion criteria of the study for patients with confirmed BC diagnosis were a possibility to obtain the specimens of EPF before treatment and normal condition of their prostates, confirmed by clinical examination and by cytological and bacteriological investigations of the EPF samples. The exclusion criteria of the study for subjects in control group were abnormal condition of their prostate such as acute and chronic prostatitis, benign prostate hyperplasia, and prostate cancer.
Specimens of EPF were obtained in sterile containers, which were appropriately labeled. Twenty μL (microliters) of fluid were taken in duplicate by micropipette from every specimen for Zn determination, while the rest of the fluid was used for cytological and bacteriological investigations. More detail information about EPF samples preparation for Zn analysis was reported in our previous studies [36, 38].
STANDARDS AND CERTIFIED REFERENCE MATERIAL
To determine concentration of the Zn by comparison with known standards, aliquots of solutions of commercial, chemically pure compounds were used for calibration. The standard samples for calibration were prepared in the same way as the samples of prostate fluid. Because there were no available liquid Certified Reference Materials (CRMs), ten sub-samples of the powdered CRM IAEA H-4 (animal muscle) were analyzed to estimate the precision and accuracy of results. Every CRM sub-sample weighing about 3 mg was applied to the piece of adhesive tape serving as an adhesive fixing backing. More detail information about CRM IAEA H-4 sub-samples preparation for Zn analysis was reported in our previous studies [36, 38].
INSTRUMENTATION AND METHOD
The facility for the radionuclide-induced EDXRF included an annular 109Cd source with an activity of 2.56 GBq, A Si (Li) detector with an electric cooling system and a portable multi-channel analyzer based on a personal computer, comprised the detection system [38]. Its resolution was 270 eV at the 6.4 keV line. The duration of the measurements of Zn concentration was 5 min for each sample obtained from healthy persons and patients with BC. The intensity of the Kα-line of Zn in EPF samples and standards was estimated from a calculation of the total area under the corresponding photopeak in the spectra.
COMPUTER PROGRAMS AND STATISTIC
All EPF samples for EDXRF were prepared in duplicate and mean values of Zn were used in final calculation. Using the Microsoft Office Excel programs, the summary of statistics, arithmetic mean, standard deviation, standard error of mean, minimum and maximum values, median, percentiles with 0.025 and 0.975 levels was calculated for Zn in EPF of healthy males and patients with BC. The difference in the results between two groups of samples (normal and BC) was evaluated by the parametric Student’s t-test and non-parametric Wilcoxon-Mann-Whitney U-test.
RESULTS
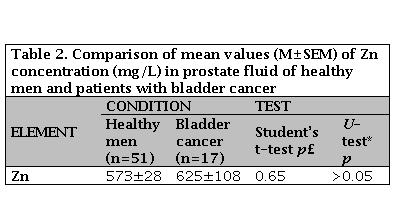
Table 1 presents certain statistical parameters (arithmetic mean, standard deviation, standard error of mean, minimal and maximal values, median, percentiles with 0.025 and 0.975 levels) of the Zn in EPF of healthy persons and patients with bladder cancer.
Table 1. Some basic statistical parameters of Zn concentration (mg/L) in prostate fluid of health men and patients with bladder cancer
M: Arithmetic mean; SD: Standard deviation; SEM: Standard error of mean; Min: Minimum value; Max: Maximum value; Per. 0.025: Percentile with 0.025 level; Per. 0.975: Prcentile with 0.975 level.
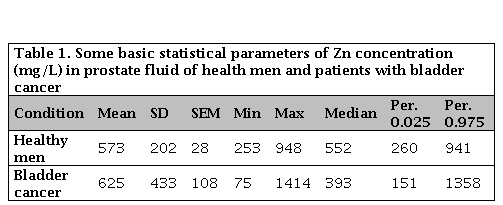
The estimation of the differences between mean values of Zn in EPF of healthy persons and patients with bladder cancer are presented in Table 2.
DISCUSSION
As was shown by us in our previous studies [39, 40, 41, 42, 43, 44, 45, 46, 47] results from the use of CRM IAEA H-4 as certified reference materials for the analysis of samples of EPF is acceptable. Good agreement of the Zn content, analyzed by the 109Cd EDXRF method, with the certified data of reference materials indicates an acceptable accuracy for the results obtained in the study and presented in Tables 1 and 2.
Medians of Zn in EPF of healthy males and, particularly, patients with BC were somewhat lower corresponding means: 552 vs 573 mg/L and 393 vs 625 mg/L, respectively (Table 1). In means that the distribution of Zn in EPF of all subjects in two groups was a little skewed to the left, unlike a normal distribution.
Both mean value of Zn in EPF of healthy males obtained in the study (573 mg/L) agree well with median of means reported in the literature (580 mg/L) [50]. All reported data on Zn in EPF concern the normal prostate of apparently healthy males or the pathological gland (benign prostate hyperplasia, prostate cancer, acute and chronic prostatitis) [50]. No published data referring to Zn in EPF of males with bladder cancer but normal prostate were found.
Because the distribution of Zn levels in EPF of all subjects in two groups was unlike a normal distribution, two group comparisons were performed using both parametric Student’s t-test and non-parametric Wilcoxon-Mann-Whitney U-test (Table 2). It was shown that the Zn in EPF of patients with BC did not differ from that in healthy subjects.
There was also no difference in the H2O content in the EPF of healthy persons and patients with BC. The water content in EPF varied from 85.2% to 92.8% for healthy males and from 86.4% to 93.5% for the patients with BC. The mean water content (M±SD) in EPF for these two group of males were 90.2±2.5% and 89.7±1.5, respectively.
Thus, we can conclude that such serious illness as BC did not impact on the Zn concentration in EPF.
This study has several limitations. Firstly, in this study the Zn concentration was measured only in the EPF of apparently healthy males and patients with BC. Future studies should be directed toward extending the list of diseases, such as heart diseases, atherosclerosis, diabetes, cancer of different localization and some others. Secondly, the sample size of healthy males and patients with BC group was relatively small. It was not allow us to carry out the investigations of Zn in EPF using differentials like dietary habits, smoking, alcohol assumption, and others. Despite these limitations, this study provides evidence on very high stability of Zn in EPF of males without prostatic diseases and shows the necessity to continue Zn research of EPF in norm and different non-prostatic diseases for final conclusion about usefulness of this test for population screening for PCa.
CONCLUSION
For the first time Zn concentration in EPF of males with bladder cancer were investigated. It was found that such serious illness as BC did not impact on the Zn concentration in the EPF. However, further studies are required to determine how other non-prostatic diseases inherent of the old persons, including heart diseases, atherosclerosis, diabetes, asymptomatic cancer of different localization and some others, impact on the Zn level in EPF. Results of such kind studies will clarify a usefulness of the Zn in EPF tests for screening for PCa.