1. INTRODUCTION
Substantially collected dietary data provide us with a comprehension of common nutritional problems of pregnant women. The Mediterranean diet (MD) model is considered one of the optimal dietary patterns that provides a better source of nutrients. The Mediterranean Diet was first mentioned to describe society's nutrition habits, which scientists recommended in the early 1960s [1]. The Mediterranean diet is optimal during pregnancy [2, 3]. The main components of such a diet are characterized by a variety of fruits, vegetables, legumes, cereals, olive oil, non-refined foods, a limited amount of meat and saturated fat intake, moderate-to-abundant fish intake, and low-to-moderate dairy products intake [4, 5]. This diet model is low in saturated fat, and high in mono-saturated fat, rich in fiber and glutathione, and includes a balanced n-6/n-3 essential fatty acid ratio and a high amount of antioxidants (especially polyphenols obtained from olive oil, vitamins E and C) [6]. The Mediterranean Diet Quality Index (MDQI) is one of several scales commonly used to assess the quality of an individual.s diet. The score in MDQI ranges from 0 to 9 points, with higher scores indicating greater adherence to MD [7]. A well-balanced macro and micronutrients provide all the energy and nutrients needed for fetal growth and development. It also protects from the development of obstetric pathologies, including birth complications, infections, and changes in fetal growth [8].
Several studies have shown that following a MD during pregnancy can reduce the risk of developing gestational diabetes (GD) and common pregnancy complications [9, 10]. A study has suggested that following MD during pregnancy may be associated with healthier weight gain [11]. Evidence suggests that following the MD during pregnancy can positively impact maternal and fetal health outcomes, including a reduced risk of preterm birth and improved fetal [9, 12, 13].
This study aimed to investigate the nutritional status and problems of pregnant women in the middle and low-income groups and obtain information about the MD diet of pregnant women using MDQI.
2. MATERIAL AND METHODS
In this cross-sectional follow-up study, 132 pregnant women between the ages of 17 and 45 were recruited from the Department of Obstetrics and Gynecology Outpatient and Inpatient Clinics of Aydın Adnan Menderes University Hospital. Pregnant women with chronic or any other diseases were excluded. Participation in the survey was voluntary, and written informed consent was received from each participant. Data were collected face-to-face in March-September 2021.
Aydın Adnan Menderes University, Faculty of Medicine Non-invasive Clinical Research Ethics Committee (Date:11.03.2021, No: 2020/203) approved the study. The principles of the Declaration of Helsinki were followed. Completing the questionnaire confirmed consent to participate in the study.
Baseline demographic and clinical data and biochemical variables were recorded from the institutional patient verification system. The perceived financial status of the participants was estimated based on income/expenditure: Poor (Income<expenditure), Moderate (Income=Expenditure), and Rich (Income>Expenditure) [14].
The 24-hour dietary recall (24 HR) method was used to evaluate food consumption. A questionnaire form was applied via face-to-face interviews to collect information on dietary intake and nutritional habits.BeBis 2.0 (Bebis) (The German food code and nutrient database BLSII.2 Turkish version) (Pasifik Elektrik ve Elektronik ve Çevre Teknolojisi Ürünleri San. Tic. Limited Şirketi, Istanbul, TURKIYE) program was used to calculate the daily energy and nutrient intakes and the consumed food amounts [15]. Energy and nutrients intakes were evaluated using Turkey Dietary Guideline (TUBER)-2015.
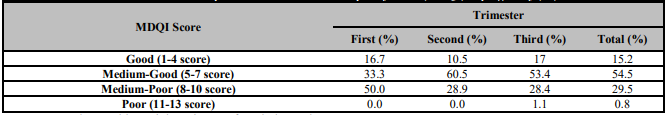
Nutritional habits (regularly consumed meals, skipped meals, food aversion, and cravings) were assessed. During the gestational period, behavioral changes for foods (such as milk, eggs, vegetables-fruit, yogurt, fish and chicken, milk desserts and puddings, sherbet deserts, molasses, sugary products, bakery products, tahini halva) were recorded as increased, decreased, not changed and never consumed [16]. MDQI, developed by Gerber et al., is based on scores for selected nutrient and food consumption levels. Scores of 1-4 were grouped as 'Good MDQI,' scores of 5-7 were grouped as 'medium to-good MDQI,' scores of 8-10 were grouped as 'medium to poor MDQI,' and scores of 11-13 were grouped as 'poor MDQI' [17].
Body weight and height were measured during trimesters. The BMI was calculated by dividing the body weight (kg) by the square of the height (m) and categorizing it as underweight, normal weight, overweight, or obese. Weight gain in the first, second, and third trimesters was recorded [18].
The participants' fasting and two-hour postprandial glucose levels were analyzed in the laboratory of the same institution. The attending nurse recorded pregnant women's systolic blood pressure and body weight during all visits [19, 20].
2.1. STATISTICAL ANALYSIS
The assumption of the average distribution of quantitative data was checked with the Kolmogorov-Smirnov test. Intergroup comparisons were made with the Kruskal Wallis H test. Whether there was a relationship between the variables was determined by Spearman correlation analysis. Descriptive statistics for the variables mean, standard deviation, median (25%-75%), min-max values, numbers, and percentages were given, and a p-value <0.05 was considered statistically significant.
3. RESULTS
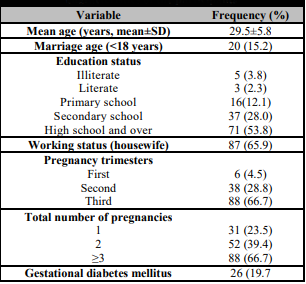
132 pregnant women were included in the study. The mean age of the pregnant women was 29.5±5.8 years and 15.2% of the womans’ marriage age was below 18 years. Of the pregnant women, 28% were below 25, 26.5% were between 26-29, and 45.5% were above 30 years (Table 1).
Of the pregnant women, 3.8% were illiterate, 12.1% were elementary school graduates, 28% were secondary school graduates, and 30.3% were university graduates (Table 1). According to the perceived family income status, 17.4% of the participants were poor; on the other hand, 82.6% were from the low-middle income group. Almost 65% of the participants were housewives (Table 1).
Approximately 5% of the participants were in the first trimester, 28.8% were in their second trimester, and 66.7% were in their third trimester (Table 1).
Overall, 34.8% of the pregnant women were skipping the main meal; lunch was the most skipped, 37.1% consumed three meals, and 20.5% had three meals and one snack daily. Of the total, 37.9% were craving foods, 28.8% were disgusted with some foods, 64.4% were taking vitamin D, and 65.9% took iron supplements.
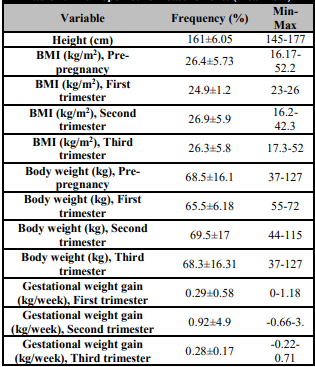
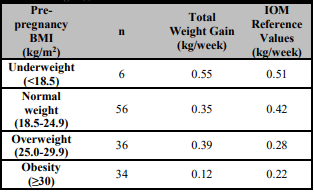
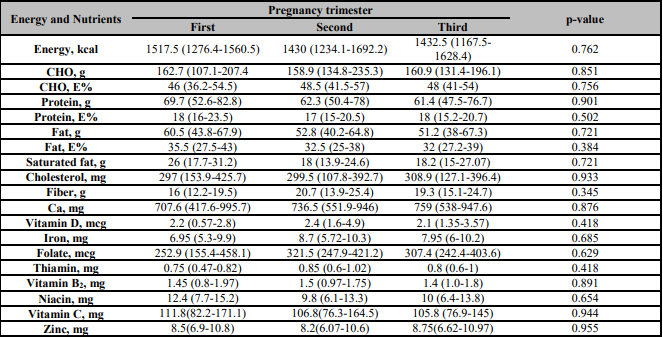
The mean pre-pregnant BMI of the women was 26.4 kg/m2 (overweight). Mean BMI, body weight and gestational weight gain depending on trimesters were given in Table 2. The mean weekly gestational total weight gain for the normal pre-pregnancy BMI level pregnant women was 0.35 kg. According to IOM recommended values, normal and obese pregnant mean weekly gestational weight gain was below the recommended values. However, underweight and overweight pregnant mean weekly gestational weight gain was over the recommended IOM values (Table 3) [17, 18]. The participants' energy, macro, and micronutrient intakes according to trimesters were given in Table 4. There were no statistically significant differences between the trimesters in energy, macronutrient, and micronutrient intakes. However, diet micronutrient intakes were below the recommendations [17].
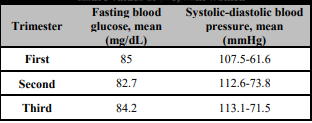
The participant's mean fasting blood glucose levels and arterial blood pressure values were given in Table 5 and mainly found within normal ranges according to AHA and ADA recommendations.
Regarding the adaptation scores of pregnant women to the Mediterranean diet, %15.2 had good, 54.5% had medium-good, 29.5% had medium-poor, and 0.8% had poor adaptation scores (Table 6).
4. DISCUSSION
Nutrition during pregnancy is crucial for both the mother's and baby 's health. MD during pregnancy can provide essential nutrients for both the mother and the developing fetus and may reduce the risk of pregnancy complications [8]. The MD has been associated with several health benefits, including reduced excess weight gain during pregnancy and improved health outcomes for both mother and baby [21]. This study used the MDQI to evaluate the Mediterranean-type nutrition model during gestation. Based on the statement, the literature review conducted in our country has yielded limited studies on the subject researched. Our study found that approximately 30% of the pregnant women had poor, 54% had moderate-good, and 15% had good compliance with MD.
Various countries have different studies on this hot topic in the literature [16, 22, 23, 24, 25, 26]. In a study from the Turkish Republic of Northern Cyprus, the MDQI score of 30 pregnant with 20-35 ages in the first and third trimesters was evaluated as good and moderate, respectively. There was no statistically significant difference between MDQI scores and some biochemical and hemoglobin findings in the first and third trimesters, except that MDQI scores and the AST values were measured in the third trimester [16]. The study conducted with 318 immigrant pregnant women in Spain reported that pregnant women moderately adhered to the MD [22].
Auguštin et al. reported that adherence to the MD was low to moderate among the 500 pregnant women, and there were no significant differences between the mainland and island region on Croatian Island. They also reported that pregnant women with wealthier and generally healthier had the highest adherence to MD. Therefore, they concluded that lifestyle and socio-economic factors such as income, education, and physical activity affected the nutrition style [23]. In another study conducted with 1118 pregnant women, the KIDMED score was used for MD. As a result, it was found that 14.5% had poor compliance with the MD, 34.8% had moderate compliance, and 50.7% had optimal compliance [25].
In our study, the mean pre-pregnancy BMI was 26.4 (overweight). In previous studies, more antenatal, intrapartum, and neonatal complications in pregnancy were observed in women who were overweight or obese compared with women who were not obese before pregnancy, according to pre-pregnancy BMI. In a study conducted in Australia with 2834 women, 11.5% were overweight, and 6.6% were obese, according to the Pre-pregnancy BMI classification [27]. In an Istanbul study of 261 women whose education and economic status were not specified, the mean pre-pregnancy BMI was 23.4 kg/m2 [28].
Pregnancy is one of the most critical periods in life when the body needs micro and micronutrients and increases macronutrients [29]. Deficiencies in essential macro and micronutrients can significantly influence pregnancy outcomes and neonatal health [30]. Women in low-income countries often enter pregnancy malnourished, and the demands of gestation can exacerbate micronutrient deficiencies with health consequences for the fetus. Examples of effective single-micronutrient interventions include folic acid, neural tube defect prevention, iodine for cretinism, zinc for the risk of preterm birth, and iron for the risk of low birth weight reduction [31]. Our study showed that pregnant women's dietary energy and micronutrient intakes were below the reference values recommended by IOM-2009 and TUBER-2015. In the study by Çelikkan in Turkiye, pregnant women's dietary iron, zinc, vitamin D, and thiamine intake levels were found below the recommendations [26].
The body's energy needs increase during pregnancy to support fetal growth and development. In our study, when pregnant women were compared in terms of dietary energy intake levels, they had lower energy intake levels than the reference values. In other studies from Turkiye, pregnant women's daily energy intake level was similar to ours [32, 33]. The pre-pregnancy body mass index (BMI) can influence how much weight a woman gains during pregnancy. However, the participants in our study received lower dietary energy than reference values; underweight pregnant women, normal weight, overweight, and obese class differed in weight gain during pregnancy, according to pre-pregnancy BMI. Several studies have shown a relationship between low adherence to the Mediterranean diet and higher body mass index (BMI) in pregnant women [28, 34, 35]. Our study found the pre-pregnancy mean BMI of the participants to be 26.4 kg/m2. Excessive weight gain during pregnancy is a known risk factor for adverse pregnancy outcomes such as gestational diabetes, preeclampsia, cesarean section, and depression [29, 36], in a recent meta-analysis of 23 studies (n=1,309,136 women) conducted worldwide, including Asia, Europe, and the Americas. Goldstein et al. reported that excessive gestational weight gain is a common problem and that about 50% of women gain more weight during pregnancy than clinical guidelines recommend [37]. In a study conducted in the United Arab Emirates, it was reported that the Mediterranean diet has a protective effect against excessive weight gain during pregnancy [38]. Di Renzo et al. reported that adherence to the Mediterranean diet was not associated with gestational weight gain. Still, it was effective in appropriate weight gain in newborns [38]. According to Wang's review study, which analyzed data from various low- and middle-income countries, gestational weight gain was insufficient in these regions [39]. In our study, pregnant women with normal and obese weight gained less weight during pregnancy than what is recommended by the Institute of Medicine (IOM) reference values. However, pregnant women with overweight more weight gained more than IOM reference values [20].
In Yong's study, weekly weight gain was found above the IOM reference values in pregnant women with obesity according to pre-pregnancy BMI [40]. According to pre-pregnancy BMI in our study, this result is similar to the weekly weight gain of overweight pregnant women.
An optimal model was defined according to the Institute of Medicine's (IOM) recommendation of three meals and two or more daily snacks [24]. In our study, the rate of those who consumed three main meals and two or more snacks was 49%. Bulunç et al. reported that 6.67% of the participants skipped meals, and the most skipped meal lunch at 40% [16]. Our study showed that lunch was the most skipped (32.6%).
Hypertension in pregnancy is generally defined as a systolic blood pressure of 140 mm Hg or higher or a diastolic blood pressure of 90 mm Hg or higher, measured on at least two occasions at least four hours apart, in a woman who was previously normotensive [41]. In our study, participants had blood pressure within the normal range. In the study of Anum, it is reported that compliance with the Mediterranean diet reduces the risk of preeclampsia in pregnant women [42].
As far as we know, we could not find an article in the literature on pregnant women from the middle and low-income groups and the Mediterranean diet. Our study's compliance rate of pregnant women with the Mediterranean diet is similar to those conducted in other countries.
4.1. STUDY LIMITATIONS
There are some limitations in our study. This study consisted of a limited number of participants, and their distribution in the groups of trimesters is not well balanced. The pre-pregnancy BMI constituted overweighed participants, whereas it would be better to have low, normal, and obese pre-pregnant groups and to compare the results of MDQI scores between the groups. More studies with more participants with chronic diseases such as diabetes and/or hypothyroidism would be better to make more robust and promising conclusions.
5. CONCLUSIONS
Adverse pregnancy outcomes are increasing rapidly all over the world. We think that making healthy food choices before conception and during pregnancy is vital for the health of the mother and baby. Including the Mediterranean diet model in the strategies that can be developed to reduce these risks seems appropriate. Due to their high prevalence and public health consequences, pregnancy micronutrient deficiencies are significant. Dietary diversification is an important strategy to address micronutrient and macronutrient deficiencies.