Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.33 no.6 Madrid nov./dic. 2016
https://dx.doi.org/10.20960/nh.801
TRABAJO ORIGINAL / Epidemiología y dietética
Abandonment to therapeutic diet on patients at risk cardiovascular in a health care clinic
Abandono de la dieta en pacientes con riesgo cardiovascular en una clínica de cuidado de la salud
Tatiana Pizzato Galdino1, Vanessa Cristina Oliveira de Lima2, Iasmin Matias de Souza2 and Ana Paula Trussardi Fayh2
1Centro Universitário Metodista IPA. Porto Alegre - RS, Brazil.
2Department of Nutrition. Health Sciences Center. Federal University of Rio Grande do Norte. Natal, RN, Brazil
ABSTRACT
Background: Cardiovascular diseases are the leading cause of death among adults and measures to reverse this situation go through changes in lifestyle, among them adopt healthy eating through professional counseling. To do this we need to keep the patient engaged in treatment, and the abandonment of treatment is an important risk factor in this population.
Objectives: To assess abandonment to dietary treatment of patients with cardiovascular risk treated on an outpatient basis, and identify the reasons for the abandonment of treatment.
Methods: Participants were patients between 18 and 70 years, of both sexes, who held their first nutritional consultation and had two or more cardiovascular risk factors. A telephone contact was made by applying a questionnaire on the withdrawal of reasons for treatment and encouraging them to return to the health service by checking the return after three months of telephone contact.
Results: Of the 142 patients with cardiovascular risk, 61.26% did not return to the service after the first visit, a percentage similar to that found in other studies, and contacted by telephone 64.37% of them. Regarding the main reasons for the withdrawal, difficulty following the diet and individual/behavioral characteristics of the patient were the aspects that contributed to the abandonment (57.14%), corroborating the findings that show the influence of cultural and socioeconomic factors on the therapeutic adherence. Although 92.86% of patients have been satisfied with the service and 75% have reported interest in resuming treatment, only 5.36% patients returned to service after the phone contact.
Conclusion: There was a high drop-out from nutritional treatment, mainly because of the difficulty of organization required to follow the diet. The motivational intervention was not enough to motivate a return to treatment.
Key words: Adherence. Abandonment. Diet therapy. Cardiovascular disease. Counseling.
RESUMEN
Introducción: las enfermedades cardiovasculares son la causa principal de muerte entre los adultos y las medidas para revertir esta situación se aplican a través de cambios en el estilo de vida, entre ellos, adoptar una alimentación saludable a través de orientación profesional. Para hacer esto, necesitamos mantener al paciente comprometido con el tratamiento, ya que el abandono de dicho tratamiento es un factor de riesgo importante en esta población.
Objetivos: evaluar el abandono al tratamiento con dieta de pacientes con riesgo cardiovascular tratados de manera ambulatoria e identificar las razones del abandono del tratamiento.
Métodos: los participantes eran pacientes entre 18 y 70 años de edad, de ambos sexos, que recibieron su primera consulta nutricional y poseían dos o más factores de riesgo cardiovascular. Un contacto telefónico se realizó aplicando un cuestionario al abandono sobre las razones para el tratamiento, y aconsejándolos que regresaran al servicio de salud comprobando si efectivamente regresaban a los tres meses del contacto telefónico.
Resultados: de los 142 pacientes con riesgo cardiovascular, 61,26% no regresó al servicio posterior a la primera visita, un porcentaje similar al encontrado en otros estudios, y fueron contactados por teléfono 64,37% de ellos. En relación a la razón principal para el retiro o abandono, dificultades siguiendo la dieta y características individuales/de comportamiento del paciente fueron los aspectos que contribuyeron al abandono (57,14%), corroborando los hallazgos que muestran la influencia de factores culturales y socioeconómicos en la adherencia al tratamiento. Aunque el 92,86% de los pacientes mostraron estar satisfechos con el servicio y 75% han reportado interés en retomar el tratamiento, solo 5.36% de los pacientes regresaron al servicio posterior al contacto telefónico.
Conclusión: hubo un alto abandono del tratamiento nutricional, principalmente debido a la dificultad de organización requerida para seguir la dieta. La intervención motivacional no fue suficiente para motivar un regreso al tratamiento.
Palabras clave: Adherencia. Abandono. Terapia de dieta. Enfermedad cardiovascular. Orientación.
Background
According to the World Health Organization, estimated that 17.5 million people die annually victims of cardiovascular disease (1) being the leading cause of death in adults (2). Among the risk factors for developing cardiovascular disease, modifiable risk factors related to nutrition and lifestyle, such as poor diet, sedentary lifestyle, obesity, hyperglycemia, dyslipidemia, hypertension are of greater importance than non-modifiable factors (age, sex and genetic predisposition) (3-5). The modification of lifestyle and adopting a healthy diet are understood as an essential part in the prevention and treatment of chronic diseases (4). Given this context, the dietitian, in the role of counselor or nutritional educator, is one that actually helps your client to select and implement desirable changes in nutrition and lifestyle that lead to adhesion of a new food behavior (6,7).
Adherence is a complex behavioral process that involves a number of factors related to the patient and their environment in addition to their clinical condition (8). In individual nutritional care in patients with or without associated diseases, interaction and mutual respect between client and counselor are essential for compliance. Thus, nutritional counseling focused on the individual extends the knowledge about the risks of an unhealthy diet, discusses nutritional aspects related to their health, increases self-confidence to introduce changes and improves understanding of the importance of treatment, increasing adherence (9).
Abandonment or non-adherence to treatment has been considered a problem among patients with risk or patients with cardiovascular disease (10-13). Data in the literature shows that 16.4% of patients fail to follow the diet prescription by difficulties to leave old lifestyle habits, 5.5% by financial constraints and 6.8% reported other difficulties such as food monotony, amount of food prescribed and not enough time to consume all meals (11). Although clinical studies continue reporting a low adherence to nutritional treatment (13-15), there are few reporting its prevalence and the reasons why patients abandon treatment.
Thus, this study aimed to evaluate the abandonment to dietary treatment of patients at risk for cardiovascular disease treated in an outpatient unit and identify its main reasons.
Methods
This study has an exploratory descriptive nature and was conducted in a nutrition clinic located in Porto Alegre, Rio Grande do Sul, Brazil. In this clinic, individual consultations are conducted with adult and elderly patients, of both sexes, and all patients receive an individualized diet according to their goals, and are instructed to return for monthly visits to the clinic to check the progress of their treatment.
The study population was all patients aged 18 to 70 years, treated in a 12-month period, which had two or more risk factors for cardiovascular disease and who did not return to the clinic within three months of his first visit. The sample was composed of patients who successfully contacted by and agreed to participate. The study protocol was approved by the Research Ethics Committee of the Rede Metodista de Educação do Sul (protocol 186/2007). All patients signed in the first consultation, consent form showing permission to access their medical records for research purposes.
In the analysis of medical data, the following information was collected: sex, age, weight and height to characterize the sample, reason for consultation and identified the number of cardiovascular risk factors that the patient had: high blood pressure (16), dyslipidemia (17), hyperglycemia or diabetes (18), obesity or high waist circumference (19), sedentary lifestyle (20) and smoking (16).
If the patient did not return to the second nutritional consulting after a period of three months, a telephone contact was made to the implement the questionnaire and collect data. On five occasions and on different days and times tried to establish telephone contact with the patient; after the fifth attempt unsuccessfully, the patient in question was excluded from the study.
All telephone calls were conducted by the same researcher, who has been properly trained and kept identical sequence of the questionnaire to all patients, exposing the issues clearly and demonstrating understanding the patient to listen and respond in a phone call that had approximately the duration of ten minutes.
The data collection instrument consists of a semi-structured questionnaire not validated and previously developed by the researchers, which comprised three distinct variables: professional relationship health-patient, single and behavioral characteristics of the patient and physical health system structure (in this case, outpatient nutrition) (8,21-23). The questionnaire was composed of six closed questions, one of which includes sub-issues relating to the identification of the reasons for the nutritional treatment abandonment, and an open question about the reason for the abandonment.
At the end of the interview, the researcher emphasizes the importance of nutritional treatment for patients with cardiovascular risk, and all patients were encouraged to return the unit to continue their treatment. Three months after telephone contact, enough time to schedule a new appointment according to the schedule of the service; it was investigated as to whether the patient had made a new nutritional consultation.
The data collected in the examination of medical records and telephone contact were structured and analyzed using the SPSS (Statistical Package for Social Sciences) version 19.0 for Windows. Descriptive statistics were used to express the results as mean, standard deviation, absolute frequency and relative frequency.
Results and discussion
Within a year, nutritional care was given to 226 patients aged between 18 and 70 years, and 142 had two or more risk factors for cardiovascular disease. After the first visit, 87 (61.26%) patients with two or more risk factors for cardiovascular disease did not return to the health service for a new nutritional consultation. The telephone call was successfully established in 56 patients. In the remaining patients, telephone contact was not successfully made for the following reasons: mobile or landline non-existent or out of service or off (64.5%) did not meet the connection (16.1%), change of residence (12.9 %), hospitalization (3.2%) and death (3.25%). Anthropometric data characterizing the sample are described in table I.
The demand for nutritional care at the clinic, reported by patients, was mainly driven by reduction in body weight (82.14%), followed by dyslipidemia correction (8.93%), nutritional education (5.36%) and control diabetes mellitus (3.57%).
The data collection instrument showed that most patients (98.2%) reported that they were well received in the clinic and 92.86% were satisfied with the nutritional care. When asked about the difficulties of nutritional treatment, the majority of respondents (98.21%) reported no difficulty as to the understanding of the list of substitutes and the size of food portions, and 43 patients (76.78%) felt they were motivated to do it. Still, 34 patients (60.71%) report having time to make meals proposed and only four patients (7.14%) sought nutritional care at another health center.
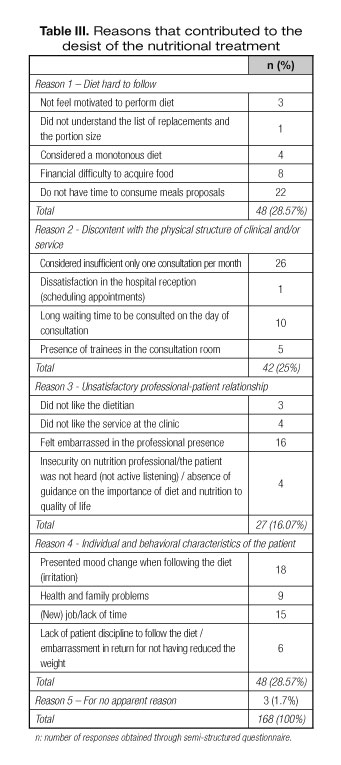
In order to check the maintenance of the prescribed diet, the patients were asked how long they were following the diet after the nutritional consultation. Table II shows the results categorized according to the main responses. In addition, table III shows the reasons given by patients which have contributed to the abandonment of the dietary treatment.
Although all patients reported satisfaction with telephone contact and 42 (75%) of these reported intention to return to the health service for a new nutritional consultation, after a period of three months after the phone call, only three patients (5.36%) returned to the clinic.
Non-adherence to treatment by patients with chronic diseases has been widely reported in the literature (23-27). In this study there was a considerably high rate of abandonment, more than half of the patients (61.26%) did not return for reassessment after the first consultation. Although the results are worrying, unfortunately they are similar to other previously published studies on adherence and treatment abandonment.
A longitudinal study by Busnello et al. (2001) in the same city as this study involving a representative sample of 945 hypertensive patients seen at a referral clinic revealed that 533 patients (56%) left the outpatient follow-up to antihypertensive treatment (28). High percentages of poor adherence were also found in another cross-sectional study involving 252 patients aged over 18 years and who had decompensated heart failure. The results showed 11% of the sample had low adherence to drug treatment, while 82% reported low adherence to non-pharmacological treatment (29).
Santos Araujo and Cabral (2013) assessing patient adherence to nutritional treatment, found that of 550 patients who started treatment, less than 50% attended the second consultation, and only about 20% continued until the third month. These results are quite similar to those found in this study, and not attending the new consultation is related to low adherence in following the prescribed treatment (12).
Many factors are related to the abandonment of the dietary treatment for patients with chronic diseases such as difficulty following the recommended diet because of the restrictive nature and financial aspects (30). In addition, other studies point to issues related to the nature of chronic diseases such as the absence of symptoms in the early stages, the lack of severity and chronicity and an unsatisfactory doctor-patient relationship and inadequate multidisciplinary approach (23,25,27,31). Still, Massing and Portela (2015), in a descriptive exploratory study in 3978 hypertensive patients found that the evaluated did not associate the pressure control diet, but only the use of the drug (32).
This study found that the difficulty in following the diet and the individual and behavioral characteristics of the patient were the reasons that contributed to the abandonment of the dietary treatment. A review of the factors that influence adherence to therapy in diabetic patients showed that non-adherence to diet is strongly linked to economic factors (10). The literature has shown that most patients have low income, and a considerable portion of these do not have any source of income. Ramos, Black and Klug (2014) showed that some patients find that some foods entered in the diet are not consistent with their social status, both culturally and financially, which inhibits food variety and motivation, and thus interferes with adherence to diet (33).
In the present study, it was not possible to assess the association between socioeconomic status and treatment abandonment, as the financial factors are not questioned objectively in the delivery of this service, although we recognize that the patient's economic condition has an impact on their adherence to the diet. However, we found that most patients followed the prescribed diet for about two weeks after the consultation. It would be possible to infer that the economic situation has also limited the maintenance of the prescribed diet after this period. For future research, we suggest the authors pay attention to these features.
Other difficulties in following the nutritional treatment that were observed in this study: individual and behavioral characteristics, the lack of time to make meals and mood change while following the diet were the most mentioned factors by patients. Massing and Portela, in a descriptive exploratory study conducted with hypertension showed that cultural factors also exerted a strong influence on adherence to dietary treatment, which requires major change in eating habits, lifestyle and even the personal beliefs (32). It is known that the power related aspects are difficult to be modified, because changing old patterns comprises components of individual history, family and social group (7,22). The way some professionals advise patients, given that the proposal for food is generally restrictive, imposing and full of prohibitive expressions, ends up generating a sense of lack of freedom and anxiety about treatment (10).
It is possible to suggest that behavioral issues have influenced the individual and the implementation of the prescribed diet. It seems that it is convenient for patients, who need to change their eating behavior, to find obstacles that impede them from following the diet. However, this situation may reflect contradictions, such as those found in this study: even if 26.79% of patients have pointed to lack of time as a reason for the withdrawal from nutritional treatment, 46.42% considered monthly consultations as insufficient. Thus, the statement of interest to attend the twice monthly nutrition clinic, as a way to encourage adherence to diet therapy, contradicts the downtime for follow-up treatment.
Treatment success can be achieved by good adherence, this being a function of the relational communication quality between the patient and the professional (8,34). In this study, 28.8% of the sample reported feeling embarrassed at some point of the consultation on professional nutrition. However, only 7.14% of the sample showed dissatisfaction with the service overall. Therefore, satisfaction with the service level and the professional attitude can be factors that influence the continuity of care, reducing abandonment.
Like any research, this study has limitations. Having been held by telephonic means, impersonality in this type of contact can cause the patient to not feel comfortable to expose their feelings or be less interested in contributing substantially to the research. The literature shows that the establishment of the professional-patient relationship is essential to help identify problems and develop mechanisms to overcome them; stimulating the patient and increasing contact with them can become good strategies to prevent poor adherence and succeed in treatment (29). Even if the telephone contact is recognized as a valid method for conducting research in food and nutrition, one phone contact was insufficient to increase the adherence to the dietary prescription in this study (35).
Another limitation of the study was not to check socioeconomic characteristics, education and occupation, even being important variables in treatment adherence (31). However, these features could not be considered in this study because they were not asked specifically in the delivery of the nutritional care.
Conclusion
The study showed a high rate of abandonment of nutritional therapy in patients with cardiovascular risk factors. The main reasons cited by patients were related to individual and behavioral factors, and motivational strategies for the return of the patient to outpatient care showed low effectiveness. Thus we see that professionals should adopt new strategies to facilitate adherence to dietary treatment for the patient and thus reduce the abandonment of this treatment. This includes negotiating priorities with the patient, providing information and clear and objective guidelines on the disease, treatment and clinical condition in which it is located, as well as improving communication in patient outside the clinic whenever possible, and encouraging return to scheduled appointments. Perhaps these actions can help many patients to follow their treatment and thus reduce abandonment in these patients.
References
1. WHO. Global action plan for the prevention and control of noncommunicable diseases 2013-2020. WHO; 2013. [ Links ]
2. WHO. The top 10 causes of death. WHO; 2012. Available in: http://www.who.int/mediacentre/factsheets/fs310/en/index2.html. Acessed in 02/02/2016. [ Links ]
3. Anderson TJ, Grégoire J, Hegele RA, Couture P, Mancini GB, McPherson R, et al. 2012 update of the Canadian Cardiovascular Society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol 2013;29(2):151-67. [ Links ]
4. Perk J, Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). Eur Heart J 2012;33(13):1635-701. [ Links ]
5. Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha, Cushman M, et al. Heart Disease and Stroke Statistics - 2016 Update A Report From the American Heart Association. Circulation 2015;131:e29-e322. [ Links ]
6. Pereira AM, Pereira AA, Leão JM, Elias MAR, Ghetti FF, Nemer ASA, et al. Desafios e reflexões na implantação de um programa de Educação Alimentar e Nutricional (EAN) em indivíduos com excesso de peso. Rev Bras Prom Saúde 2015;28(2):290-6. [ Links ]
7. Rodrigues EM, Soares FPTP, Boog MCF. Resgate do conceito de aconselhamento no contexto do atendimento nutricional. Rev Nutr 2005;18(1):119-8. [ Links ]
8. Sabaté E. Adherence to long-term therapies: evidence for action. WHO; 2003. [ Links ]
9. Filgueira SL, Deslandes SF. Avaliação das ações de aconselhamento. Análise de uma perspectiva de prevenção centrada na pessoa. Cad Saúde Pública 1999;15:S121-31. [ Links ]
10. Espírito Santo MB, Souza LME, Souza ACG, Ferreira FM, Silva CNMR, Taitson PF. Adesão dos portadores de diabetes mellitus ao tratamento farmacológico e não farmacológico na atenção primária à saúde. Enf Rev 2012;15(1):88-101. [ Links ]
11. Pimenta CDZ, Paixão MPCP. Análise da Adesão da Terapêutica Nutricional Proposta aos Pacientes Atendidos na Clínica Integrada de Nutrição de Uma Faculdade Particular em Vitória-ES. Saúde e Pesq 2012;6(1):153-62. [ Links ]
12. Santos CM, Araújo AR, Cabral PC. Evolução antropométrica de pacientes com sobrepeso atendidos em ambulatórios de nutrição. RASBRAN 2013; 5(1): 13-20. [ Links ]
13. Girotto E, Andrade SMD, Cabrera MAS, Matsuo T. Adesão ao tratamento farmacológico e não farmacológico e fatores associados na atenção primária da hipertensão arterial. Ciênc Saúde Colet 2013;18(6):1763-72. [ Links ]
14. Tang L, Patao C, Chuang J, Wong ND. Cardiovascular risk factor control and adherence to recommended lifestyle and medical therapies in persons with coronary heart disease (from the National Health and Nutrition Examination Survey 2007-2010). Am J Cardiol 2013;112(8):1126-32. [ Links ]
15. Vivas EA, Plaza BL, Weber TK, López LB, Milla SP, Catalán AL, et al. Variables predictoras de baja adherencia a un programa de modificación de estilos de vida para el tratamiento del exceso de peso en atención primaria. Nutr Hosp 2013;28(5):1530-35. [ Links ]
16. Sociedade Brasileira de Cardiologia, Sociedade Brasileira de Hipertensão, Sociedade Brasileira de Nefrologia. VI Diretrizes Brasileiras de Hipertensão Arterial. Arq Bras Cardiol 2010;95(1):1-51. [ Links ]
17. Sociedade Brasileira de Cardiologia. V Diretriz brasileira de dislipidemias e prevenção da aterosclerose. Arq Bras Cardiol 2013;101(4):1-20. [ Links ]
18. Sociedade Brasileira de Diabetes. Diretrizes da Sociedade Brasileira de Diabetes 2014/2015. AC Farmacêutica; 2015. [ Links ]
19. WHO. Physical status: The use and interpretation of anthropometry. Geneva: WHO; 1995. [ Links ]
20. Martin SB, Morrow JR, Jackson AW, Dunn AL. Variables related to meeting the CDC/ACSM physical activity guidelines. Med Sci Sports Exerc 2000;32(12):2087-92. [ Links ]
21. Costa JA, Balga RSM, Alfenas RDCG, Cotta RMM. Promoção da saúde e diabetes: discutindo a adesão e a motivação de indivíduos diabéticos participantes de programas de saúde. Ciênc Saúde Colet 2011;16(3):2001-9. [ Links ]
22. Alves BA, Calixto AATF. Aspectos determinantes da adesão ao tratamento de hipertensão e diabetes em uma Unidade Básica de Saúde do interior paulista. J Health Sci Inst 2012;30(3):255-60. [ Links ]
23. Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients' adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. Plos One 2013;8(12):e80633. [ Links ]
24. Quintana JF. A relação entre hipertensão com outros fatores de risco para doenças cardiovasculares e tratamento pela psicoterapia cognitivo comportamental. Rev SBPH 2011;14(1):3-17. Available in: <http://pepsic.bvsalud.org/scielo.php?script=sci_arttext&pid=S1516-08582011000100002&lng=pt&nrm=iso>. Accessed in 01/06/2016. [ Links ]
25. Ritholz MD, Wolpert H, Beste M, Atakov-Castillo A, Luff D, Garvey KC. Patient-provider relationships across the transition from pediatric to adult diabetes care a qualitative study. Diabetes Educ 2013;40:40-7. [ Links ]
26. Zullig LL, Peterson ED, Bosworth HB. Ingredients of successful interventions to improve medication adherence. JAMA 2013;310(24):2611-2. [ Links ]
27. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of Health chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015;17(2):1-36. [ Links ]
28. Busnello RG, Melchior R, Faccin C, Vettori D, Petter J, Moreira LB, et al. Características associadas ao abandono do acompanhamento de pacientes hipertensos atendidos em um ambulatório de referência. Arq Bras Cardiol 2001;76(5):349-51. [ Links ]
29. Castro RAD, Aliti GB, Linhares JCC, Silva ERRD. Adesão ao tratamento de pacientes com insuficiência cardíaca em um hospital universitário. Rev Gaúcha Enferm 2010;31(2):225-31. [ Links ]
30. Assis CN, Navarro F, Bessa F. Fatores associados à adesão e a não adesão do tratamento não farmacológico em usuários com obesidade assistidos pelo Programa Saúde da Família, Complexo do Alemão-RJ. RBONE 2012;6(31):1-8. [ Links ]
31. Pucci N, Pereira MR, Vinholes DB, Pucci P, Campos ND. Conhecimento sobre hipertensao arterial sistêmica e adesão ao tratamento anti-hipertensivo em idosos. Rev Bras Cardiol 2012;25(4):322-9. [ Links ]
32. Massing LT, Portella MR. Fatores determinantes da adesão de hipertensos a conduta dietoterápica. RBCS 2015;13(43):37-45. [ Links ]
33. Ramos CI, Pretto ADB, Klug JC. Adesão às recomendações alimentares de usuários portadores de diabetes tipo 2. Demetra 2014;9(2):561-75. [ Links ]
34. Dimatteo MR, Haskard-Zolnierek KB, Martin LR. Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev 2012;6(1):74-91. [ Links ]
35. IBGE - Instituto Brasileiro de Geografia e Estatística. Pesquisa de Orçamentos Familiares 2008-2009 - POF. Rio de Janeiro; 2010. [ Links ]
![]() Correspondence:
Correspondence:
Ana Paula Trussardi Fayh.
Department of Nutrition.
Health Sciences Center.
Federal University of Rio Grande do Norte.
Avenida Senador Salgado Filho 3000.
Campus Universitário, Natal,
59078-970 RN, Brazil
e-mail: apfayh@yahoo.com.br
Received: 26/03/2016
Accepted: 27/05/2016