Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.101 no.6 Madrid jun. 2009
LETTERS TO THE EDITOR
Bronchopneumonia caused by a perforation in an achalasic esophagus with a focal squamous cell carcinoma
Bronconeumonía secundaria a perforación en carcinoma epidermoide de esófago sobre acalasia
Key words: Esophageal achalasia. Pneumonia. Squamous cell carcinoma.
Palabras clave: Acalasia de esófago. Neumonía. Carcinoma epidermoide.
Dear Editor,
Esophageal achalasia, of unknown etiology, is the most common primary disorder of esophageal motility. A reduced set of patients with achalasia present very dilated esophagus (advanced type IV). We present a case of a 53-year-old male lacking toxic habits. He had lung tuberculosis appropriately treated 26 years previously. There are no other known antecedents or habitual treatments.
The patient came to the hospital for dyspnea of approximately one week evolution, with slight cough, thoracic pain with pleuritic characteristics on the right side and a feverish sensation.
Additional tests performed showed:
-Chest X-ray: multi-lobe lung involvement with right pleural effusion (Fig. 1).
-Hemogram: 33.98 x 109/L leukocytes (91% neutrophil), normocytic-normochromic anemia and 390,00 x 109/L platelets.
-Basic biochemical analyses showed a slight pattern of cholestasis.
-Basal arterial gasometry with moderate hypoxia.
-Legionella and Pneumococcus antigens in urine: negative.
-Pleural fluid with empyema criteria; drainage with thorax tube was instituted and a sample was sent for culture.
-Serology for atypical bacterial pneumonia and secretion culture (including hemoculture and tuberculosis study) were requested.
Following initial improvement in response to antibiotic treatment (ceftriaxone and azithromycin) for severe community-acquired pneumonia, the patient was admitted to the Intensive Care Unit due to acute respiratory insufficiency, shock and renal failure.
Computed axial tomography (CAT) scan of the thorax revealed a very distended esophagus, full of content that filled part of the right chest (Fig. 2).
Upper gastrointestinal endoscopy showed significant dilation of the esophageal lumen, which was filled with food remains, with sigmoid morphology. On withdrawal, purple papilliform tissue compatible with neoplasia was seen; perforation could not be eliminated from consideration.
Anteroposterior thoracotomy was performed, observing the lung adhered to the wall and diaphragm. Megaesophagus with a 4-5 mm perforation in the middle third was found, open at the pleura and the sixth segment of the pulmonary parenchyma; pulmonary necrosis and significant air leakage, with pus and food remains were also evident. Complete pulmonary liberation was performed, with resection of the sixth segment, liberation of the megaesophagus and suture of the perforation, plus gastrostomy feeding tube insertion and pharyngostomy.
The patient was administered broad-spectrum antibiotic therapy and systemic anti-fungicides. He required vasopressor support and continuous venovenous hemodiafiltration. Mechanical ventilation was given for adult respiratory distress syndrome.
Once organ failure was resolved, the patient was operated again for gastrostomy reconstruction and Heller myotomy.
Ten days later, hemodynamic instability with lowered hematocrit appeared. The patient was transferred to surgery, ischemia in the entire upper mesenteric artery being found. The patient died a few hours later in multiple organ failure.
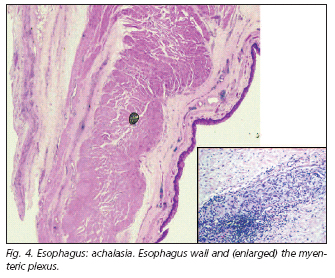
Necropsy confirmed a 4 cm squamous cell carcinoma in the lower-middle third of the esophagus (Fig. 3); there was achalasia infiltration of the entire wall, pleura and right lung, with esophageal dilation of 15 cm diameter and significant muscle layer hypertrophy and absence of ganglion cells in the myenteric plexus (Fig. 4). Diagnosis was acute bronchopneumonia and bilateral hemorrhage with foreign body-type giant cell reaction to food remains; 1-cm perforation in the gastric wall, proximal to the lower esophageal sphincter; mural stomach and small intestine infarct, plus ischemic infarct in liver and spleen.
The main symptom in achalasia is the dysphagia (1) indicated by this patient later in a directed clinical history. There may be chest pain, weight loss, heartburn, regurgitation or symptoms of recurrent bronchoaspiration (1-5). Endoscopy permits evaluating the presence of malignant neoplasia when faced with pseudoachalasia and because 7% of patients having achalasia develop squamous cell carcinoma after 15-25 years (1,6,7).
R. M. Galeiras, P. Rascado, M. J. Lorenzo1, D. Freire and M. J. García Monje
Intensive Care Unit and 1Anatomic Pathology Service. Complejo Hospitalario Universitario A Coruña, Spain
References
1. Robinson GV, Kanji H, Davies RJ. Selective pulmonary fat aspiration complicating esophageal achalasia. Thorax 2004; 59: 180. [ Links ]
2. Akritidis N, Gousis C, Dimos G. Achalasia associated with aspiration pneumonia. Chest 2003; 123: 608-12. [ Links ]
3. Langdon DE. Mycobacterial lung infections. Mayo Clin Proc 1999; 74: 744-5. [ Links ]
4. Maitani F, Iwasaki M, Inoue H. Video-assisted thoracoscopic surgery under local anesthesia for right empyema secondary to aspiration pneumonia caused by esophageal achalasia: case report. Tokai J Exp Clin Med 2005; 30: 183-7. [ Links ]
5. Teramoto S, Yamamoto H, Yamaguchi Y. Diffuse aspiration bronchiolitis due to achalasia. Chest 2004; 125: 349-50. [ Links ]
6. Lehman MB, Clark SB, Ormsby AH, Rice TW. Squamous mucosal alterations in esophagectomy specimens from patients with end-stage achalasia. Am J Surg Pathol 2001; 25: 1413-8. [ Links ]
7. Rosai J. Gastointestinal tract, esophagus. In: Rosai J, editor. Rosai and Ackerman's Surgical Pathology. Edinburg: Mosby; 2004. p. 615-47. [ Links ]











 texto en
texto en