INTRODUCTION
Physical inactivity and high-calorie foods have increased the prevalence of obesity worldwide above 13% (15% in women) 1. Obesity is a greater risk factor for cardiovascular disease for women than men 2 and it has been associated with multiple comorbidities 3 and adverse effects on physical fitness 4. Frequently, therapeutic strategies are insufficient, since they fail to prevent weight regain 5. Thus, surgical treatments are often adopted for morbid obesity or obesity in the presence of comorbidities 6.
The increase in obesity cases 7 has led to a parallel increase in the number of bariatric surgeries, particularly laparoscopic sleeve gastrectomy (SG), which is currently the most frequent bariatric surgical procedure in the world 8. Although the surgical treatment of obesity has been demonstrated as an effective intervention for weight loss, as well as for remission or improvement of obesity-associated comorbidities 6,9, the impact on some components of physical fitness (PF), such as cardiorespiratory fitness (CRF) and muscle strength (MS), is unclear. These physical factors are important for their predictive health value 10,11). Moreover, so far there is few information about the impact of SG in objectively assessed physical activity (PA) 12.
Cardiorespiratory fitness and muscle strength are strong determinants of morbidity and mortality 10,11,13 and the inclusion of serial CRF testing should be considered in the obese population when an intervention is applied 4. However, there is contradictory information regarding the impact of bariatric surgery on CRF 14,15,16 and MS 14,17,18. The vicious cycle between physical inactivity, obesity and poor physical fitness is well known 19. People with obesity perform less PA compared to eutrophic people 20, but there is contradictory information about changes in physical activity after bariatric surgery 12,18,21,22. Research into physical activity patterns of bariatric patients has primarily relied on self-report questionnaires 18,22, with only one study (n = 4) assessing the impact of sleeve gastrectomy on objectively assessed PA of subjects undergoing this surgery 12.
Considering that physical inactivity is associated with noncommunicable diseases 23 and has been considered by the World Health Organization (WHO) as the fourth risk factor for global mortality, and that cardiorespiratory fitness and muscle strength are indicators of health and life expectancy 10,11,13, the purpose of this study is to describe the changes in physical fitness and physical activity in patients with obesity after undergoing sleeve gastrectomy.
MATERIALS AND METHODS
SUBJECTS
In this observational study, 23 females with obesity who underwent SG were included. Two patients did not receive the second evaluation (one month after surgery). Exclusion criteria were severe cardiovascular diseases, chronic renal insufficiency and exercise-limiting comorbidities such as musculoskeletal impairments. In addition, patients with smoking habits, postmenopausal women and patients with previous bariatric surgery were excluded. Inclusion criteria for adult women patients were a BMI equal to or greater than 30 kg/m2 who were scheduled for sleeve gastrectomy.
Participants were recruited during the years 2015 and 2016, from different clinics in the region of Valparaíso, Chile. Subjects were required at least three hours of fasting, using comfortable clothes and to refrain from drinking coffee and alcoholic beverages and performing intense physical exercise at least 24 hours before each evaluation. Time was given for the familiarization of the participants with the laboratory and each one of the tests. The evaluations were performed in the morning, to avoid variations in circadian rhythm at the Laboratory of Exercise Physiology of Universidad Andres Bello, Viña del Mar, Chile.
Prior to surgery, and at one month and three months thereafter, an assessment of anthropometrics measures, physical fitness and physical activity was conducted.
All procedures performed in studies involving human participants were in accordance with the standards of the Ethic Committee for Research in Human Beings of the Faculty of Medicine of Universidad de Chile (registered number 149-2014) and with the Declaration of Helsinki of 1964 and its later amendments or comparable ethical standards. Informed consent was approved by the corresponding ethic committee and was obtained from all individual participants included in the study.
ANTHROPOMETRICS
Anthropometrics were taken using standardized protocols 24. Body mass index (BMI) and waist circumference (at iliac crests level) were determined using a Detecto 439 balance scale and a Rosscraft anthropometric tape, respectively. Weight loss was expressed as percentage excess weight loss (%EWL) 25.
MUSCLE STRENGTH ASSESSMENT
Static MS was evaluated by measuring the handgrip strength (HGS) with a Dynatron handgrip dynamometer (Dynatronics Corporation, Salt Lake City, USA). Patients stood in the anatomical position, with the elbow extended. The participants were verbally told to produce their maximal force and strongly encouraged to maintain it for five seconds.
Isometric quadriceps MS was assessed with the subjects seated with the hip angle fixed at 100° and knee angle set at 90° of flexion. A padded cuff was secured above the ankle malleolus and attached to the load cell artOficio FMON-1 (artOficio, Santiago, Chile). The subjects were fixed to chair and told verbally to produce their maximal force for five seconds.
For HGS and quadriceps MS, three trials were done (left and right side were alternated) with a pause of about two minutes between trials. The best score was registered and the average strength between both sides was calculated.
CARDIORESPIRATORY FITNESS ASSESSMENT
Patients performed a submaximal cardiopulmonary bicycle test on a cyclo-ergometer Monark 915 E (Monark Exercise AB, Vansbro, Sweden). A gradual protocol was used, starting at 0.5 Watts/kg of body weight with gradual increase of 20 W/2 minutes, with the subjects cycling at 60 rpm, until the stopping criteria (respiratory quotient ≥ 1.1 or modified Borg scale of perceived exertion > 7/10 points). After the patients reached their VO2 peak, determined as the highest attained VO2 over 30 seconds during the test, as previously recommended 4, subjects cycled during three minutes for active recovery with no load.
During the test, gas exchange was measured using an ergospirometry system Cortex Metalyzer® 3B (Cortex Biophysik, Leipzig, Germany) and heart rate was monitored with a Polar H7 telemetry heart rate monitor (Polar Electro Oy, Kempele, Finland).
PHYSICAL ACTIVITY ASSESSMENT
Physical activity was measured using the Actigraph wGT3X monitor (ActiGraph, Pensacola, USA) and magnitude vector activity counts were analyzed. The interval of recorded time (epoch) was set at 60 seconds, shown as valid for measuring PA in adults 26. Participants were asked to wear the monitor on the dominant side, at waist level, during all waking hours for seven consecutive days and to remove it only for water activities. All women with ≥ 10 h/day of monitor wear time for ≥ 3 days at both the pre- and post-surgery assessments were included in the analysis. Non-wear time was defined as 60 minutes or more of consecutive zero counts 26.
Data were analyzed with Actilife 6 software (ActiGraph, Pensacola, USA), and the results were expressed as a percentage of light, moderate and vigorous PA using the cutoff points of Freedson for adults 27).
STATISTICAL ANALYSIS
For data distribution, the Shapiro-Wilk normality test was used. Data for all variables were normally distributed, except for PA parameters. The changes in CRF and MS were evaluated using a repeated-measures ANOVA with the Bonferroni post-hoc analysis. To compare PA non-parametric tests were applied due to their non-normal distribution. Wilcoxon tests were used in cases where Friedman tests found differences in PA between values from the three evaluations. The statistical analysis was performed using SPSS 21.0 software (SPSS Inc, Chicago, IL, USA). A p-value of < 0.05 was considered as statistically significant.
RESULTS
Twenty-three female patients were included in this study. Two patients had a diagnosis of controlled arterial hypertension, seven had controlled hypothyroidism and 14 had hepatic steatosis. All patients underwent laparoscopic SG. The mean age of these patients was 36.1 ± 11.1 years at admission.
ANTHROPOMETRIC CHARACTERISTICS
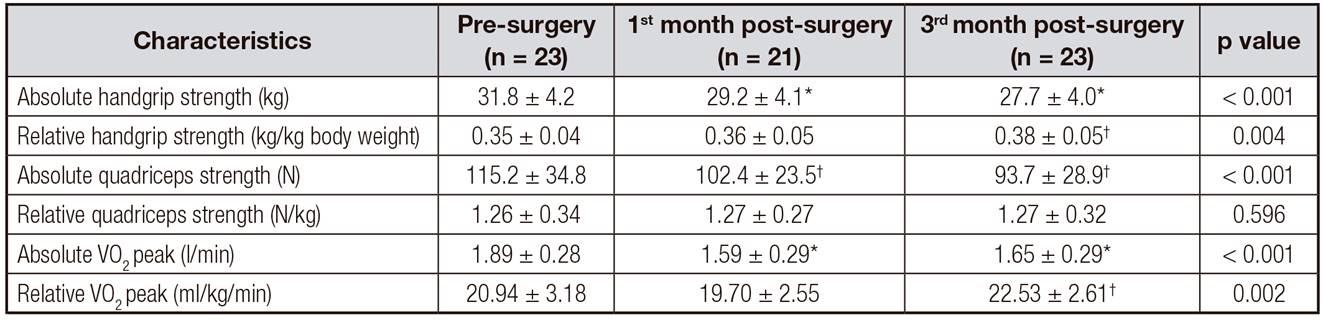
After SG, body weight, excess weight, BMI and waist circumference decreased significantly (p < 0.001) (Table I).
Table I. Anthropometric characteristics in the three moments of assessment
OB: obesity; EW: excess weight; %EWL: percentage excess weight loss; WC IC: waist circumference at the level of iliac crests. Data are presented as means ± SD. ANOVA p value.
*p < 0.001 compared with the preoperative values.
†t-test p value.
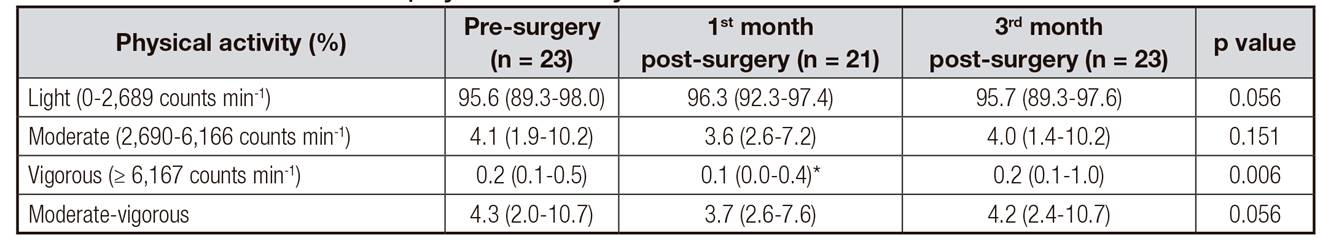
MUSCLE STRENGTH
Patients had a decrease in absolute quadriceps strength one month (p = 0.045) and three months (p = 0.001) after surgery. Patients lost 19% of their quadriceps strength after three months. However, quadriceps strength relative to body weight did not change (p = 0.596) (Fig. 1).
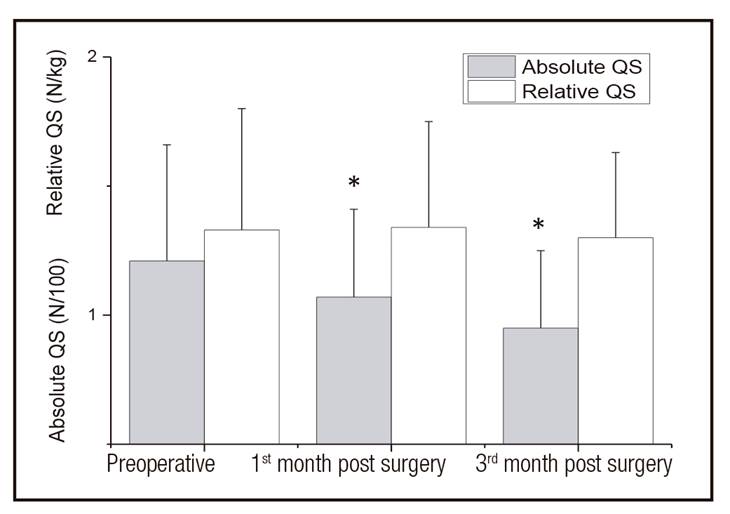
Figure 1. Comparison of quadriceps strength (QS) between the three moments of assessment. *p < 0.05 compared with the preoperative values.
Absolute handgrip strength decreased after both one and three months post SG (p < 0.001). There was also a reduction in absolute handgrip strength after three months post-surgery compared to the first postoperative month (p = 0.003) (Fig. 1). When expressing handgrip strength in proportion to body weight, there was an increase in handgrip strength after three months post-surgery compared to preoperative (p = 0.011) (Table II).
CARDIORESPIRATORY FITNESS
The absolute VO2 peak significantly decreased by the first and third month (p < 0.001) post-surgery with respect to the preoperative assessment, without changes between the two postoperative assessments.
The VO2 peak relative to body weight showed an increase from baseline at third months (p = 0.005) after SG (Table II).
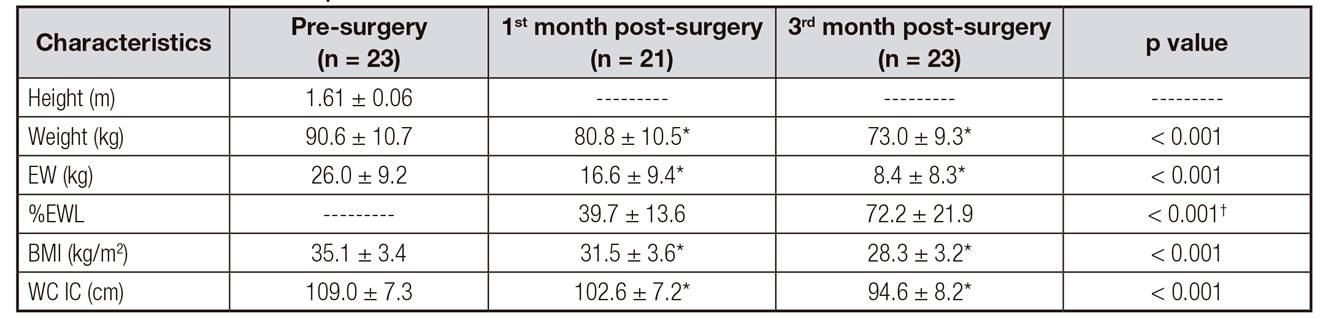
PHYSICAL ACTIVITY
The average number of valid days of PA assessed was six. No significant differences were observed between the three assessment periods for the percentages of light (p = 0.056), moderate (p = 0.151), and moderate-vigorous (p = 0.056) PA. Percent vigorous physical activity decreased only at the first postoperative month compared with baseline (p = 0.022) (Table III).
DISCUSSION
The present study indicates that sleeve gastrectomy results in a considerable decrease in absolute MS in the short term after surgery. This data concurs with another study which found absolute MS decreased four months after gastric bypass surgery 14. It is important to consider that these results were obtained in the periods of greater post-surgical caloric restriction, which may influence the loss of MS 28. However, a reduction of absolute MS in both upper and lower limbs one year after biliopancreatic diversion 17 and gastric bypass was also reported 29. These results are likely a consequence of the decrease in muscle mass that has been previously described 30. A decrease in ghrelin, hormone that has a protective effect against loss of muscle mass after bariatric surgery, could have a role in those changes 31. On the other hand, Otto et al. 32 showed no changes on absolute HGS at six, 12 and 18 weeks after a SG or gastric bypass, and Neunhaeuserer et al. 18 showed no changes in absolute HGS and in quadriceps MS in patients six months after SG.
As a palliative approach, exercise training after bariatric surgery could preserve absolute muscle strength and even increase it 14,33.
In the present study, when expressing HGS according to body weight, an increase in HGS three months post-surgery was observed when compared to preoperative HGS. These observations concur with previous studies evaluating one year after bariatric intervention 17,29. The most plausible explanation is the effect of the magnitude of the reduction in post-surgical body weight patients, thus, overestimating muscle strength by expressing it relative to body weight.
Regarding the evaluation of CRF, our research group suggest the use of cyclo ergometer instead of treadmill or walking test (i.e., six minutes walking test or shuttle walking test) in the evaluation of obese patients, where the impact of body weight is less relevant.
The VO2 peak results in this study from the preoperative assessment are similar to those reported by Wilms et al. 34 and are associated with a high risk of mortality from any cause 35.
Some studies report maintained 14,15 or decreased 18 CRF when expressed in absolute values after bariatric surgery. These results could be explained by considering the significant loss of post-surgical muscle mass 30. Additionally, the reduction of ghrelin 31 could be a factor that would negatively influence myocardial contractility and cardiac output 36).
The results of this study showed an improvement in CRF relative to body weight after surgery, which agrees with those reported from other studies 14,15,18 and differ regarding the lack of changes in CRF related to body weight reported by De Souza et al. 16. The studies that presented VO2 peak related to lean mass did not find changes after surgery 14,15.
On the other hand, bariatric patients should begin the exercise intervention before surgery 37 and continue it as soon as possible after the procedure 33. In addition, it is interesting to note that low values in preoperative VO2 peak have been associated with an increase in short-term complications after bariatric surgery. So it has been suggested that CRF should be improved prior to intervention to potentially reduce postoperative complications 38.
Additionally, the results of this study show that SG does not affect patients' lifestyles, regarding their PA habits. The same has been described by studies of gastric bypass patients who did not change their level of PA, objectively measured, at six (21) and nine months postoperatively 39. However, when PA was subjectively assessed through questionnaires, an improvement in PA behavior was reported 18,21,22.
Given the importance of moderate-to-vigorous physical activity (MVPA) for health outcomes and surgical success, there is a need of using more valid methods for objectively measuring PA. Considering that the objectively measured amount of MVPA of obese subjects is below WHO recommendations for adults aged between 18 and 64 years, the maintenance of physical inactivity following bariatric surgery could mean an increased risk of regaining body weight lost with surgery. Further, there may also be an increased risk of developing non-communicable diseases 23.
For future studies, it is advisable to conduct a body composition evaluation through DEXA in order to express the variables of physical fitness not only in relation to body weight, but also to lean mass, as previously recommended 4.
Considering the fact that MS and CRF do not improve by weight loss only, we suggest adding physical fitness assessments before and after surgery to design personalized specific exercise programs for these patients and also implement PA counselling about the importance of changing their lifestyle 40.
In conclusion, large-scale weight loss through SG results in a decrease in absolute muscle strength. Despite a large decline in quadriceps strength, when it was expressed relative to body weight, its ratio remained unchanged. Also, regarding muscle strength, we observed an improvement in the handgrip strength/body weight ratio. In addition, patients with obesity have very low CRF, which decreases after SG. However, when peak oxygen consumption was expressed as a ratio to body weight, improvement was observed. Finally, no significant differences were observed in objectively measured PA with respect to the preoperative assessment.