Introduction
The Mediterranean Diet (MD) was first defined in the 1960s, mainly based on what is observed in Greece and Southern Italy1,2. The traditional is characterized by high consumption of vegetables, fruits, nuts, legumes and unprocessed cereals and low consumption of meat, meat products; and dairy products3. Several epidemiological studies have shown that the MD is a healthy eating model4,5. The literature suggests that a high degree of adherence to the MD is associated with a lower risk of several types of chronic and degenerative diseases, in turn increasing life expectancy and quality1,6. Despite these benefits, the MD is being abandoned or not adopted by young generations in most Mediterranean countries7. Especially in the younger generation, there has been a shift away from this nutritional pattern towards a high-energy diet, rich in saturated fats and low in micronutrients. This transition has led to an increase in obesity, especially among children and adolescents in the Mediterranean and other industrialized countries8. Although the literature on MD and health is abundant, MD and disordered eating behavior have not been studied sufficiently.
According to the Diagnostic and Statistical Manual of Mental Disorders (5th edition; DSM-5), an eating disorder is a behavioral condition characterized by severe, persistent disturbance in eating behaviors and is associated with distressing emotions and thoughts9. Individuals with eating disorders have abnormal and harmful eating habits. They overthink eating to lose weight and to maintain a low weight, and their behaviors reach dimensions that threaten their general health10. Emotions can alter eating behavior and contribute to eating disorders. In response to stress, emotional eaters consume more high-fat snack items and sweet-fatty foods than individuals who are not classified as emotional eaters11.
Early identification of eating disorders is important for preventing possible health problems12. Adolescence and youth adulthood are periods when people are at relatively high risk in terms of nutritional behaviors. Studies have shown that the risk of eating disorders is higher in younger individuals13,14. Data also show that eating disorders are more common in women15,16.
Ninety-five per cent of eating disorders occur in women, and they are more common in high school and college students17. In addition, there is a strong relationship between anorexia nervosa and bulimia nervosa; both occur mainly in healthy young women who begin to worry excessively about their weight and physique17. Approximately 50% of patients with anorexia develop bulimia and vice versa4,18. Emotional eating might be a predictor for eating disorders and affect eating habits, and people who overeat when feeling down prefer to choose appetizing, energy-dense foods that are thought to have mood-enhancing properties due to their high sugar content19. Eating habits have proved to be an important predictor of eating behavior20.
Young adults transitioning from adolescence to adulthood are referred to as "emerging adults"21 and according to the World Health Organization (WHO), the youth period is an important process in which the long-term eating habits are largely determined from adolescence to adulthood. However, it is known that young people tend to have malnutrition behavior characterized by low consumption of vegetables and fruits, high amounts of fast food and sugary drinks5,22.
Evaluating the eating attitudes and behaviors of young adults and determining the possible factors affecting their food intake is important to prevent health problems that may arise in the future. This study aimed to evaluate the effects of adherence to the MD on eating attitudes and emotional appetite in young women.
Methodology
Participants
This is a cross-sectional study included young women (n=306) aged 18-24 (21.16±1.4 years old) in Ankara/Türkiye. In a random sampling, individuals without a chronic disease, who agreed to participate in the study, and met the age criteria were included. Individuals who did not meet these criteria and/or did not complete the questionnaires were excluded.
Food records
The food intake of individuals was assessed by using the 24-hour record method. Accordingly, individuals were asked to indicate all the food and beverages, in grams and milliliters, respectively, that they had consumed the previous day from midnight to midnight. Food consumption records were evaluated by the Nutrition Information System computer program and energy and nutrients were calculated23.
Anthropometric measurements
Anthropometric measurements were collected according the to the conventional criteria and measuring procedures. Body weight (BW, kg) was measured with a scale and, body height (cm) was measured to the nearest 0.1 cm using a vertical stadiometer. Body mass index (BMI) was obtained by dividing the body weight by the square of the height. BMI values of the participants were evaluated according to the World Health Organization (WHO) classification.
Questionaries
Validated questionnaires were administered to each participant. Eating attitudes and behaviors of individuals were evaluated with the Eating Attitude Test-26 (EAT-26)24 and the Emotional Appetite Questionnaire (EMAQ)25. The Mediterranean Diet Quality Index (MAI)26 was used to determine the level of adherence to the MD. The level of physical activity was measured with the short version of the International Physical Activity Questionnaire (IPAQ), which is validated for the Turkish population27.
The EAT-26 was developed by Garner et al.24 to measure the symptoms of anorexia nervosa; its Turkish validity and reliability were performed by Savaşır and Erol28; The Cronbach’s Alpha was found to be 0.70. The EAT-26 is a 26-item scale, with each item answered on a 6-point Likert scale ranging from ‘never’ to ‘always’. The most symptomatic response receives a score of 3, the next most symptomatic response receives a score of 2 and the least symptomatic receives a score of 1. The remaining three choices receive a score of 0. The total scores are the sum of the composite items, ranging from 0 to 78. Scores ≥20 on the EAT-26 indicate abnormal eating attitudes and behavior, and they may identify those with high disordered eating tendencies28. The Cronbach’s alpha of EAT-26 is 0.898.
The EMAQ was developed by Nolan et al.25, and its Turkish validity and reliability study was conducted by Demirel et al.29. This questionnaire consists of 22 items including the existence of negative or positive emotions (14 items) and negative or positive situations (8 items). In this way, it is designed to reveal the relationship between the eating behaviors of an individual and their emotional state25. Each item is rated from 1 to 9 ‘much less’ (1-4), ‘the same’ (5), and ‘much more’ (6-9). Negative emotions and situations can be assessed together to obtain an EMAQ-negative score, and positive emotions and situations can be assessed together to obtain an EMAQ-positive score. There are no cut-off points for EMAQ scores. Cronbach’s alpha value is 0.839.
The MAI is a calculation tool that indicates adherence to the MD26. A score is obtained by calculating the daily consumption of several foods (in grams) as follows: Cereals + Legumes + Potatoes + Vegetables + Fresh and Dried Fruits + Fish + Olive Oil) / (Milk + Cheese + Yogurt + Meats + Eggs + Animal Fats and Margarines + Sweet Drinks + Cakes / Pies + Cookies or Biscuits). A score of ≤1.75 indicates low adherence to the MD, 1.75-2.75 indicates moderate adherence and >2.75 indicates high adherence.
The IPAQ short form includes seven questions about walking, moderate-intensity activity, vigorous activity metabolic equivalent of task and time spent sitting27. These activities have standard metabolic equivalent of task (MET) scores; 3.3 for walking, 4.0 for moderate intensity, 8.0 for vigorous physical activity. According to the type of activity of individuals, MET scores are multiplied by the number of minutes and the number of days performing the activity (MET-min/week score = MET value X activity minutes X number of activity days). After this calculation, the individuals were divided into groups based on their activity levels: inactive, moderately active, and heavily active according the IPAQ instructions27.
Procedure
Eligible participants were provided a detailed explanation of the aims and implications of the research. Those who decided to participate then provided written informed consent. The participants were instructed on how to fill out the questionnaires. The Ethics Committee of Gazi University granted ethical approval. The study was conducted in line with the Declaration of Helsinki.
Covariates
The following potential confounders of the relation between the EAT-26, the EMAQ, and the MAI were collected: age (years), physical activity level, smoking, alcohol consumption, dieting status as self-declaration, and BMI (kg/m2).
Statistical analyses
Statistical analyses were conducted with SPSS 21.0 (IBM Corp., Armonk, NY, USA). The distribution of the data was evaluated with the Kolmogorov Smirnov test. Leven’s test was used to assess the homoscedasticity. Continuous data are presented as the mean and standard deviation or median and interquartile range; categorical data are presented as percentage. Normally distributed data were analyzed with parametric tests, and non-normally distributed data were analyzed with non-parametric tests. Binary Pearson correlation testing was used to determine correlations between the EMAQ, the EAT-26, the MAI, and BMI with p<0.05 considered statistically significant. The statistical model was adjusted for age, gender, BMI, diet quality, and physical activity (except when the covariate was a dependent variable of the model). The strength of the association was estimated by calculating odds ratios (OR) and 95% confidence interval (CI). Multivariate analyses were performed with and without confounding variables. EMAQ negative and positive scores were selected as predictors due to the possible association with disordered eating, and MAI was added for the determination of possible effect of MD.
Results
The participant characteristics according to EAT-26 scores are shown in Table 1. According to EAT-26, most of the participants (80.3%) with disordered eating tendencies had normal BMI, 9.9% were overweight, 2.8% obese and 7.0% were underweight. No statistical significance was found between groups (p>0.05). There is no difference smoking, alcohol, and meal consumption in terms of EAT-26 groups. The high dieting status was 28.2% in the disordered eating tendencies group and 11.1% in the group without disordered eating tendencies (χ2=12.490, p<0.001).
Table 1. General characteristics of participants according EAT-16 group.
| General characteristics | EAT-26 - <20 | EAT-26 - ≥20 | Total | χ2 | p | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Dieting status | ||||||||
| Yes | 26 | 11.1 | 20 | 28.2 | 46 | 15.0 | 12.490 | <0.001** |
| No | 209 | 88.9 | 51 | 71.8 | 260 | 85.0 | ||
| Smoking | ||||||||
| Yes | 21 | 8.9 | 12 | 16.9 | 33 | 10.8 | 3.596 | 0.079 |
| No | 214 | 91.1 | 59 | 83.1 | 273 | 89.2 | ||
| Alcohol consumption | ||||||||
| Yes | 11 | 4.7 | 6 | 8.5 | 17 | 5.6 | 1.477 | 0.240 |
| No | 224 | 95.3 | 65 | 91.5 | 289 | 94.4 | ||
| Breakfast consumption | ||||||||
| Yes | 197 | 83.8 | 59 | 83.1 | 256 | 83.7 | 0.021 | 0.856 |
| No | 38 | 16.2 | 12 | 16.9 | 50 | 16.3 | ||
| Lunch consumption | ||||||||
| Yes | 208 | 88.5 | 57 | 80.3 | 265 | 86.6 | 3.182 | 0.110 |
| No | 27 | 11.5 | 14 | 19.7 | 41 | 13.4 | ||
| Dinner consumption | ||||||||
| Yes | 232 | 98.7 | 71 | 100.0 | 303 | 99.0 | 0.915 | 0.990 |
| No | 3 | 1.3 | 0 | 0.0 | 3 | 1.0 | ||
| MAI groups | ||||||||
| Low adherence | 118 | 50.2 | 37 | 52.1 | 155 | 50.7 | 1.133 | 0.568 |
| Modarate adherence | 57 | 24.3 | 20 | 28.2 | 77 | 25.2 | ||
| High adherence | 60 | 25.5 | 14 | 19.7 | 74 | 24.2 | ||
| IPAQ groups | ||||||||
| Low physical activity | 203 | 86.4 | 51 | 71.8 | 254 | 83.0 | 9.677 | 0.008** |
| Modarate physical activity | 16 | 6.8 | 7 | 9.9 | 23 | 7.5 | ||
| High physical activity | 16 | 6.8 | 13 | 18.3 | 29 | 9.5 | ||
| BMI groups | ||||||||
| Underweight | 26 | 11.1 | 5 | 7.0 | 31 | 10.1 | 1.985 | 0.576 |
| Normal weight | 174 | 74.0 | 57 | 80.3 | 231 | 75.5 | ||
| Overweight | 31 | 13.2 | 7 | 9.9 | 38 | 12.4 | ||
| Obesity | 4 | 1.7 | 2 | 2.8 | 6 | 2.0 | ||
| Age | 21 (20-22) | 21 (20-22) | 21 (20-22) | 0.367 | ||||
MAI: Mediterranean adequacy index; IPAQ: International Physical Activity Questionnaire; BMI: Body mass index; SD: Standart Deviation. Data are expressed as median (IQR) and percentages for categorical data. Differences between groups were conducted with Chi-Square test and independent T-test. **p<0,001.
The median and interquartile range (IQR) values of MAI, BMI and the EMAQ subscale values according to EAT-26 are presented in Table 2. The EMAQ-negative total scores were higher with disordered eating tendencies than the group without disordered eating tendencies [median 6.80 (IQR 3.91-6.33); median 4.44 (IQR 3.46-5.60), p=0.004, respectively]. Similarly, EMAQ negative emotions and situations were higher in those with disordered eating tendencies (p=0.022, p=0.004, respectively). MAI, BMI values, EMAQ-positive emotions, EMAQ-positive situations, and EMAQ-positive total score did not differ according to EAT-26 groups (p>0,05).
Table 2. MAI, BMI and EMAQ values according to EAT-26 groups.
| EAT-26<20 | EAT-26≥20 | p | |
|---|---|---|---|
| Median (IQR) | Median (IQR) | ||
| MAI | 1.73 (1.03-2.82) | 1.69 (1.12-2.61) | 0.860 |
| BMI values (kg/m 2 ) | 21.48 (19.97-23.33) | 21.64 (20.06-23.43) | 0.729 |
| EMAQ-negative emotions | 2.33 (1.77-2.88) | 2.66 (2.11-3.0) | 0.022* |
| EMAQ-negative situations | 2.0 (1.40-2.60) | 2.60 (1.80-3.40) | 0.004* |
| EMAQ-positive emotions | 3.60 (3.0-4.0) | 3.40 (3.0-4.60) | 0.989 |
| EMAQ-positive situations | 3.33 (2.66-4.0) | 3.33 (3.0-4.0) | 0.847 |
| EMAQ-negative total | 4.44 (3.46-5.60 | 6.80 (3.91-6.33) | 0.004* |
| EMAQ-positive total | 7.0 (5.93-7.93) | 2.0 (2.0-2.0) | 0.898 |
MAI: Mediterranean adequacy index; BMI: Body mass index; EMAQ: Emotional Appetite Questionnaire. Differences between groups were conducted with Mann Whitney U-test. *p<0.05.
Correlations between EAT-26, BMI, EMAQ- negative and positive subscales are presented in Table 3. There was a positive correlation between EAT-26 and EMAQ negative situations (r=0.114, p<0,05). EMAQ-negative emotions were correlated with EMAQ-negative situations (r=0.558, p<0.01) and EMAQ-positive situations (r=0.150, p<0.05). EMAQ-negative situations were correlated with EMAQ-positive situations (r=0.214, p<0.01). BMI was not found to be associated with EAT-26, EMAQ-subscales, and MAI index (p>0.05).
Table 3. Bivariate correlations of the variables of the study.
| EAT-26 | EMAQ | EMAQ | EMAQ | EMAQ | MAI index | |
|---|---|---|---|---|---|---|
| Negative emotions | Negative emotions | Positive emotions | Positive emotions | |||
| BMI | -0.035 | 0.060 | -0.010 | -0.051 | -0.110 | 0.086 |
| EAT-26 | 0.101 | 0.114* | 0.098 | 0.046 | -0.021 | |
| EMAQ-Negative emotions | 0.558** | 0.058 | 0.150* | -0.025 | ||
| EMAQ-Negative situations | 0.041 | 0.214** | -0.075 | |||
| EMAQ-positive emotions | 0.520** | -0.021 | ||||
| EMAQ-positive situations | 0.007 | |||||
| MAI index |
BMI: Body Mass Index; EAT-26: Eating Attitude Test-26; EMAQ: Emotional Appetite Questionnaire; MAI: Mediterranean Adequacy Index. *p<0.05, **P<0.01.
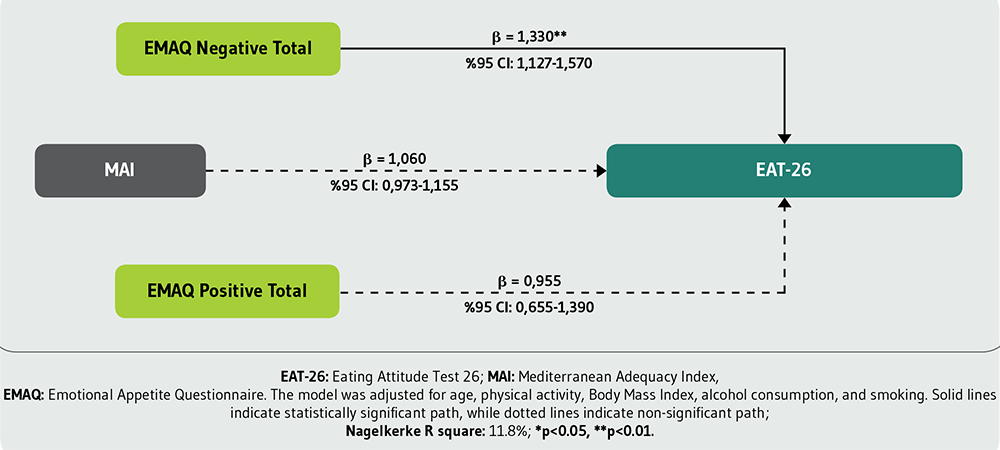
The associations between EAT-26, EMAQ and BMI values (kg/m2) according to binary regression analysis are presented in Figure 1. Accordingly, MAI, EMAQ-negative and EMAQ-positive total scores were considered predictors and EAT-26 a constant. The model was adjusted for age, alcohol consumption, smoking and BMI. As a result, EMAQ-negative scores were found to be predictor for EAT-26 (β=1.330; p < 0.001). Beta estimates revealed that nearly 1.33-point higher EMAQ-negative score (95%CI: 1.127-1.570) was associated with one-point increase in EAT-26 score (p<0.05).
Discussion
The main objective of the present study was to identify the relationships between adherence to the MD, eating attitudes and emotional eating. Half of the participants (50.7%) had low adherence to the MD; the remaining participants had moderate (25.2%) or high (24.2%) adherence. In one study, which included children and youth living in Croatia, the adaptation of individuals to the MD was evaluated with KIDMED. The researchers observed that 39.9% of the university students had have poor adherence to the MD, 46.8% had moderate adherence and 13.3% had good adherence29,30. In another study conducted with 252 university students in Spain, KIDMED showed that 20.7% of participants had poor adherence to the MD, a large proportion of participants (63.7%) had eating habits that needed improvement and only 15.5% have optimal adherence to the MD31. In a study conducted with medical school students in Turkey, 42.7% of the participants had poor adherence to the MD32. In general, research has suggested that university students are at risk from certain unhealthy habits, such as poor diet31. In this study, compliance with the MD was low, similarly to the previous literature. Despite its benefits, the MD has not been adopted by the young population8. We considered the MD to be a healthy eating model, and we investigated its relationship with disordered eating risk, a topic that has not been studied extensively.
The evaluation of various connections between nutritional quality and mental health is an new emerging area of nutritional epidemiology32. Adherence to the MD is associated with better emotional well-being and lower risk for depression31,32. One of the suggested explanations for this inverse correlation is the probable interaction between MD nutrients and the serotoninergic transmission, including metabolism, release, uptake, and receptor activity33. These connections highlight the need for further research into the MD and eating habits. In a 9.4-year follow-up study with 11,800 women, the researchers reported a potential inverse association between the MD eating pattern and the risk of anorexia nervosa and bulimia nervosa33. In another study, emotional eating (assessed with the Three Factor Eating Questionnaire subscale) and uncontrolled eating were negatively associated with the KIDMED score34. In the current study, we no observed an association between the MAI, EAT-26 and EMAQ scores.
Studies have shown that the risk of eating disorders is higher in younger individuals35,36. College students may experience several sociological and cultural changes. Many students move from the family nucleus, move to a new city, and become responsible for their own eating habits, including buying food and cooking independently. These changes can lead to skipping meals regularly, preferring fast food, consuming alcohol and smoking all of which favoring the emergence of eating disorders18. Academic stress can also be another factor and may be associated with bulimic behaviors, as risky behaviors or thoughts can be generated as a factor in combating stress, increasing the possibility of developing an eating disorder17. In this study, we observed that 23.2% (n=71) of the participants were at risk for disordered eating according to EAT-26. In a study conducted with university students, the researchers evaluated eating behaviors with the Eating Attitude Test-40. They found that 12.2% of men and 12.8% of women were at risk of eating disorders. In another study, 34.2% of individuals were at risk of eating disorders35. Saleh et al. also conducted a study like our own and reported that among 2,001 female participants, 28.6% scored ≥20 on the EAT-2636. We have presented our study variables according to the EAT-26 scores, which were different between the groups, and not the MAI scores, smoking, alcohol and meal consumption and BMI which were not different. However, dieting and IPAQ scores were different between the groups. A score of ≥20 for EAT-26 indicates a high level of concern about body weight or problematic eating behaviors as well as dieting37. Consistently, we expected greater dieting behavior in the disordered eating risk group. Alkazemi et al., presented similar results; female Kuwaiti students who perceived themselves as overweight or who incorrectly estimated their weight status had higher odds of disordered eating attitudes and dieting behaviors38. They also reported that such patterns of eating attitudes can be used to identify female undergraduates at particular risk of disordered eating practices. Excessive dieting linked to eating disorders might work against the development of healthy eating behaviors to maintain a normal BMI.
Anthropometric measurements provide important evidence of eating disorders38. Saleh et al. reported a significant positive correlation between BMI and EAT-26 scores among 2,001 female participants36. In our study, BMI values did not differ between the EAT-26 groups. In another study, Nolan et al. evaluated disordered eating with the EMAQ and reported a significant correlation between EMAQ-negative scores and BMI in a non-clinical sample. They claimed that these findings suggest but do not prove, as the data are correlational that the tendency to eat more when experiencing negative emotions may contribute to weight gain and obesity25. Inversely, the tendency to eat less when experiencing negative emotions may contribute to becoming underweight. The number of individuals in the obese and overweight groups is generally low in the entire study population. This may be the reason why there was no significant difference. There is a need for studies with larger samples to evaluate the effect of disordered eating behavior on anthropometry.
In the validity and reliability study of the Emotional Appetite Questionnaire, the authors evaluated the relationship between eating attitudes and emotional appetite. They found that EAT-26 scores correlated with three of the four emotional appetite subgroups (respectively, r=-0.190, r=0.251, r=0.197)29. According to the results of the current study, the EMAQ-negative emotions, EMAQ-negative situations, and EMAQ-negative total score were higher in the disordered eating group. In another study, higher EAT-26 scores (a tendency towards disordered eating) were significantly associated with greater emotional eating39. Sadness, rage, frustration, anxiety, fear, and boredom are some negative emotions that have been investigated and linked to eating habits. Negative emotions may demotivate college students from choosing healthy foods and increase their likelihood of selecting unhealthy foods18. These findings are in line with the current study results. In general terms, it is known that emotions are very important in food selection, and negative moods such as stress, anxiety or psychiatric disorders are linked with obesity and alcohol abuse risk. Emotional eating is eating in response to negative emotions, which increases the risk of excessive consumption of palatable foods, which are not a component of MD, and energy intake40.
This study has several strengths. Young women present a risk group for eating disorders. In this study, the evaluation of the nutritional status of individuals through the MAI, as well as their disordered eating behavior, provides important data for the evaluation of the nutritional habits of individuals with eating disorders. In addition, the inclusion of possible covariates in the study strengthens the statistical analysis. Finally, we selected the participants randomly to avoid bias. As a limitation, for food consumption, the 24-hour record method gives information about a limited period. Individuals do not follow their regular eating habits for this one day. For this reason, record food consumption over 3 days or add a food frequency questionnaire. Including more covariates that affect adherence to the MD and eating behavior would reduce the risk of confusion bias.
Conclusions
In this study, the participants’ adherence to the MD was low. Regarding our main research question, we no observed association between the MAI and impaired eating behavior. It should also be noted that the relationship between the MAI and eating disorders may be bidirectional, and adherence to the MAI may decrease after an individual develops an eating disorder. We predict that it would be beneficial to conduct a study with a similar design with a 3-day food consumption record or a food consumption frequency questionnaire to assess the two-way association. The other important results of this study are the higher percentage of dieting of those with disordered eating behavior, and the negative components of emotional appetite are one of the factors which explain the high EAT-26 scores. These results reveal the role of negative emotional states in impaired eating behavior and general health.