Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Angiología
versão On-line ISSN 1695-2987versão impressa ISSN 0003-3170
Angiología vol.75 no.6 Madrid Nov./Dez. 2023 Epub 29-Jan-2024
https://dx.doi.org/10.20960/angiologia.00538
Case Reports
Abdominal aortic rupture in idiopathic retroperitoneal fibrosis
1Angiology, Vascular and Endovascular Surgery Service
2Diagnostic Imaging Service. Diagnóstico Maipú DASA. Autonomous City of Buenos Aires, Argentina
3Interventional Cardiology Unit. Clínica Bazterrica. Autonomous City of Buenos Aires, Argentina
Introduction:
retroperitoneal fibrosis (RPF) is a rare disease characterized by the formation of inflammatory and fibrous tissue in the retroperitoneal space, around the abdominal aorta and iliac arteries, often including the ureters.
Case report:
we present a 90-year-old male patient with RPF treated with meprednisone, who attended to the emergency room due to a ruptured inflammatory abdominal aortic aneurysm.
Discussion:
in RPFs associated with abdominal aortic aneurism, endovascular or surgical treatment is recommended when the aortic diameter is larger than 5.5 cm or when it is rapidly growing (> 1 mm/month) because the danger of rupture would appear to be the same as atherosclerotic aneurysms. However, there are no guidelines or algorithms to follow the vascular management of patients with PRF and a “non-aneurysmal” aorta in the event of failure steroid treatment.
On the other hand, the risk of arterial remodeling and progressive aortic dilatation during steroids treatment has been described. Although the changes are subclinical, there were reported cases in which the patients received surgical treatment due to the rupture, such as in our patient where a complication occurred despite having a maximum aortic diameter of less than 4 cm.
Recently, a series of 6 patients with RPF non-aneurysmal abdominal aorta, that had not responded properly to medical treatment, received infrarenal abdominal aorta endovascular exclusion.
Keywords Idiopathic retroperitoneal fibrosis; Chronic periaortitis; Inflammatory abdominal aortic aneurysms
INTRODUCTION
Retroperitoneal fibrosis (RPF) is a rare condition characterized by the formation of inflammatory and fibrous tissue in the retroperitoneal space, around the abdominal aorta and iliac arteries, often involving the ureters. This is the case of a patient diagnosed with RPF on methylprednisolone who required emergency endovascular treatment due an inflammatory abdominal aortic aneurysm tear.
CASE REPORT
This is the case of a 90-year-old man with a past medical history of hypertension, dyslipidemia, and a 4-year-old diagnosis through a CT-guided biopsy of idiopathic retroperitoneal fibrosis with periaortic region involvement, but spared ureters. The patient had been on 4 mg oral methylprednisolone at a different health center. A recent magnetic resonance imaging (MRI) scan performed 1 month ago revealed the presence of a mildly dilated infrarenal abdominal aorta 34 mm in diameter (Fig. 1).
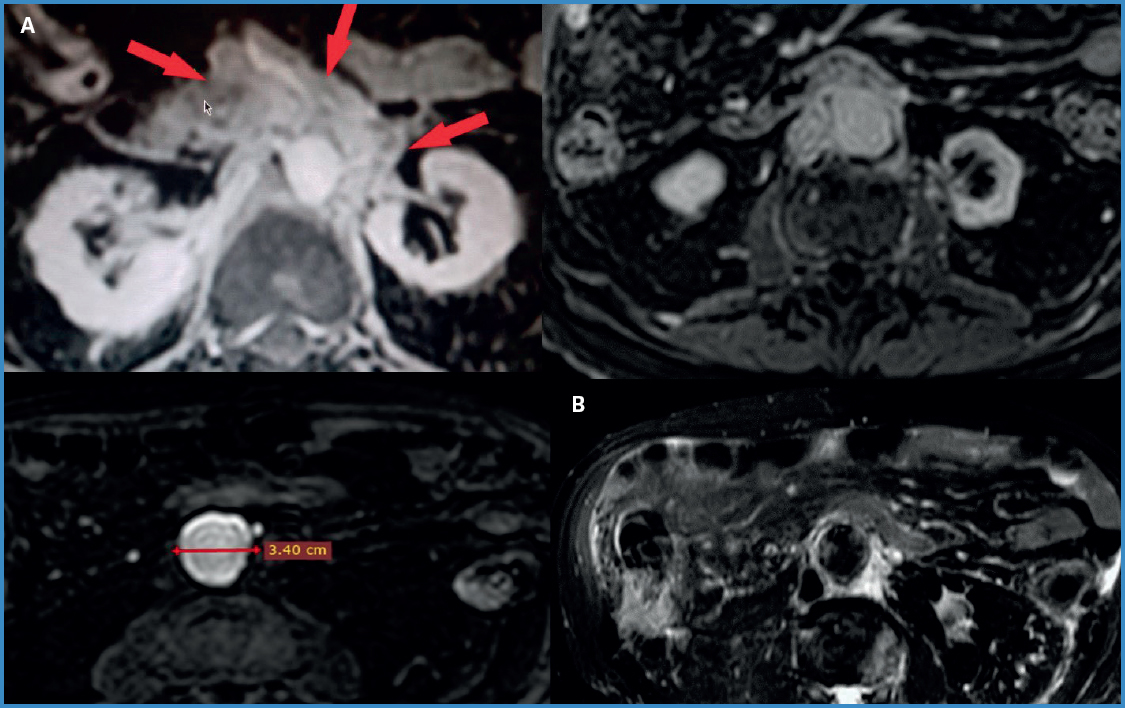
Figure 1. Gadolinium-enhanced MRI. A. T1-weighted sequence. Periaortic enhanced tissue, maximum abdominal aortic diameter of 34 mm. B. T2-weighted sequence. Hyperintense periaortic tissue.
The patient presented to the ER with sudden and severe epigastric pain radiating to the back. The coronary computed tomography angiography (CCTA) performed revealed the presence of an infrarenal abdominal aortic tear with retroperitoneal and mediastinal hematoma associated with free fluid in both the abdomen and the pelvis. We believe the rupture was due to the lateral weakness of the aortic wall following steroid treatment since no increased aortic diameter was seen compared to the previous MRI (Fig. 2). At admission, the patient was hypotensive (60/40 mmHg), required inotropic support and blood transfusion plus an additional maintenance dose of IV hydrocortisone due to the patient’s past medical history of chronic corticosteroid use. Emergency endovascular treatment was decided with 2 Endologix VELA™ cuffs because there were no stent grafts available at the moment. The procedure was uneventful. The patient had an interrecurrence of atrial fibrillation of high ventricular response that responded to bisoprolol. The patient was discharged 1 week later on anticoagulation (acenocoumarol). Ten months later, he passed away due to a hemorrhagic stroke.
DISCUSSION
Two-thirds of RPFs are idiopathic, and the remaining ones are due to various causes, such as malignant tumors (lymphoma, sarcoma, carcinoid tumor, and metastatic tumors) and, less frequently, to trauma, radiation therapy, infections, or drug-related causes (ergot alkaloids, methysergide, beta-blockers, or dopamine agonists). Men are affected 2 to 3 times more often than women (1,2).
Diagnosis and follow-up are performed through CT scans or MRIs. However, in novel cases of RPF, neoplastic causes should be the first thing to rule out (2).
Idiopathic RPF is an autoimmune disease, which can occur in isolation, associated with other autoimmune diseases, or in the context of a fibroinflammatory disorder involving various organs such as the pancreas, or salivary glands. Idiopathic RPF is histologically characterized by a lymphoplasmacytic infiltrate of IgG4-bearing cells and described as an IgG4-related disease. Although the rate of IgG4-related idiopathic RPFs is still to be elucidate, retrospective cohorts in Japan (10 out of 17), the United States (13 out of 23), and Argentina (10 out of 19) demonstrated that over 50% of the patients with idiopathic RPF had histopathological findings of IgG4-related disease (3-5). Although treatment modalities for idiopathic RPF do not differ, differentiation is essential since the availability of serum IgG4 levels to monitor treatment response and follow-up can reduce the need for repeated radiological imaging modalities and contrast exposure. Additionally, the diagnosis of IgG4-related RPF should initiate the search for extraretroperitoneal disease.
Some authors have described subtypes of urogenital and vascular RPF based on clinical characteristics. In the vascular subtype, they have observed that retroperitoneal fibrosis can develop around a non-dilated or dilated aorta, distinguishing “non-aneurysmal” from “perianeurysmal” forms of RPF (5).
However, there are currently no standardized criteria to categorize idiopathic RPF, and this entity is included in the spectrum of chronic periaortitis (CP), defined as a set of idiopathic diseases whose common denominator is a fibroinflammatory tissue growing in the periaortic retroperitoneum that can compromise the ureters and the inferior vena cava. CP includes idiopathic retroperitoneal fibrosis (IRPF), inflammatory abdominal aortic aneurysms (IAAA), and a combination of both diseases called perianeurysmal retroperitoneal fibrosis (1-6).
The first-line therapy to treat RPF is corticosteroids. The goals are to induce regression of the retroperitoneal mass, reduce the inflammatory response, alleviate symptoms such as abdominal or lumbar pain, manage obstructive complications, and prevent relapses.
In cases of RPF associated with aortic aneurysms, called aneurysmal CP, imaging follow-up is advised. The additional therapeutic goal is to prevent aneurysm rupture. Therefore, surgical or endovascular intervention is advised for aortic diameters > 5.5 cm or rapid diameter growths (> 1 mm per month), since the risk of rupture does not seem to be higher than that of atherosclerotic aortic aneurysms (1-7).
However, there is not such a thing as a fixed set of clinical practice guidelines or algorithms that should be followed in case of failed treatments for the vascular management of patients with RPF with non-aneurysmal abdominal aorta.
Back in 2022, Sultan et al. treated 6 patients diagnosed with refractory idiopathic RPF and medical therapy-resistant persistent abdominal pain with stent grafts. They reported that all patients remained asymptomatic at the 53-to-84-month follow-up and experienced a two-thirds reduction of the periaortic soft tissue cross-sectional area within the first 6 months, almost going back to normal at 2 years (8).
On the other hand, when studying corticosteroid therapy in patients with idiopathic RPF, arterial remodeling should be considered because progressive aortic dilation can occur during steroid therapy. Although such changes are often subclinical, cases requiring surgical treatment following ruptures have been reported, as it was the case with our patient (7,9,10).
Idiopathic retroperitoneal fibrosis is a rare condition that can become complicated if the infrarenal aorta ruptures at a smaller diameter than is often recommended for therapeutic reasons. Endovascular exclusion proved to be a safe and effective alternative.
Further studies are needed to establish vascular treatment indications for patients with RPF and abdominal aortas with diameters < 5 cm.
BIBLIOGRAFÍA/REFERENCES
1. Palmisano A, Vaglio A. Chronic periaortitis:a fibro-inflammatory disorder. Best Practice &Research Clinical Rheumatology 2009;23:339-53. DOI:10.1016/j.berh.2008.12.002 [ Links ]
2. Caiafa RO, Vinuesa AS, Izquierdo RS, et al. Retroperitoneal fibrosis:role of imaging in diagnosis and follow-up. Radiographics 2013;33:535-52. DOI:10.1148/rg.332125085 [ Links ]
3. Khosroshahi A, Carruthers MN, Stone JH, et al. Rethinking Ormond's disease:“idiopathic”retroperi-toneal fibrosis in the era of IgG4-related disease. Medicine (Baltimore) 2013;92:82-91. DOI:10.1097/MD.0b013e318289610f [ Links ]
4. Angarola E, Valeo Chulvi M, Peuchot V, et al. Immunoglobulin G4-related retroperitoneal fibrosis. Medicina (B Aires) 2022;82:91-8. [ Links ]
5. ŁońI, Lewandowski J, Wieliczko M, et al. Retroperitoneal fibrosis, a rare entity with urorenal and vascular subtypes –preliminary data. Renal Failure 2022;44:688-92. DOI:10.1080/08↚2X.2022.2064303 [ Links ]
6. Yardimci GK, Ardali Düzgün S, Farisogullari B, et al. Comprehensive assessment and outcomes of patients with chronic periaortitis. Clin Exp Rheumatol 2022;40:801-10. DOI:10.55563/clinexprheumatol/araba3 [ Links ]
7. Chandna A, Sharma AP, Pareek T, et al. IgG4-related retroperitoneal fibrosis:an emerging masquerader with a sinister presentation. Urology 2019;133:16-20. DOI:10.1016/j.urology.2019.06.007 [ Links ]
8. Sultan S, Acharya Y, Hezima M, et al. Management of retroperitoneal fibrosis with endovascular aneurysm repair in patients refractory to medical management. Front Surg 2022;9:1-22. DOI:10.3389/fsurg.2022.946675 [ Links ]
9. Ikeda A, Mitomi K, Konishi T, et al. Endovascular Repair of a False Aneurysm Developing from IgG4-Related Periaortitis during Corticosteroid Therapy. Ann Vasc Surg 2015;29:1452.e5-9. DOI:10.1016/j.avsg.2015.04.070 [ Links ]
10. Kasashima S, Kawashima A, Kasashima F, et al. Immunoglobulin G4-related periaortitis complicated by aortic rupture and aortoduodenal fistula after endovascular AAA repair. J Endovasc Ther 2014;21:589-97. DOI:10.1583/14-4670R.1 [ Links ]
Received: June 11, 2023; Accepted: September 21, 2023











 texto em
texto em 



