Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Medicina Intensiva
versão impressa ISSN 0210-5691
Med. Intensiva vol.32 no.3 Abr. 2008
REVISIÓN
Significance of venous oximetry in the critically ill
Importancia de la oximetría venosa en el enfermo crítico
P. Bauer; K. Reinhart; M. Bauer
Department of Anaesthesiology and Critical Care Medicine. Friedrich-Schiller-University. Jena. Germany.
ABSTRACT
Critically ill patients are threatened or affected by multi-organ failure (MOF). Tissue hypoxia is one of the most important co-factors of MOF. Venous oximetry allows the critical estimation of the global oxygen (O2) supply-demand ratio and can be gained from mixed (SvO2) and central venous blood (ScvO2). Cellular requirements dominate the feedback hierarchy of the O2-metabolism. This review describes the history and validity of haemodynamic monitoring, illustrates the physiological background and clinical application of venous oxymetry and presents carbon dioxide analysis as evidence of the usefulness of a multi-modal approach in cardio-respiratory monitoring. Variation of cardiac output, optimisation of arterial O2-saturation and adaptation of O2-extraction are shown to be the relevant levels of pathophysiological adaptation as well as therapeutic intervention. We portray the functional equivalence of ScvO2 and SvO2 and analyse their diagnostic, therapeutic and prognostic significance, providing the basis for the efficacy of venous oximetry as an important marker of critical illness. Finally, having drawn an outline of current developments for the better understanding of the oxidative balance of individual organs, we stress the importance of a synoptic O2-monitoring strategy as well as the need to use its beneficial, yet unfulfilled, clinical potential.
Key words: oxygen, monitoring, critical illness.
RESUMEN
Los enfermos críticos tienen riesgo de fracaso multiorgánico (FMO) o ya lo sufren. La hipoxia tisular es uno de los cofactores más importantes de FMO. La oximetría venosa permite la estimación crítica de la ratio de aporte-demanda del oxígeno global (O2) y puede ser obtenida de la sangre venosa mixta (SvO2) y central (ScvO2). Las necesidades celulares dominan la jerarquía de retroalimentación del metabolismo de O2. Esta revisión describe la historia y validez del control hemodinámico, ilustra el fundamento fisiológico y aplicación clínica de la oximetría venosa y presenta el análisis de dióxido de carbono como prueba de la utilidad del enfoque multimodal en el control cardiorrespiratorio. Se comprueba que la variación del gasto cardiaco, la mejora de la saturación de O2 arterial y la adaptación de la extracción de O2 son los niveles importantes para la adaptación fisiopatológica y la intervención terapéutica. Presentamos el perfil de ScvO2 y SvO2 y analizamos su importancia diagnóstica, terapéutica y pronóstica, proporcionando la base para la eficacia de la oximetría venosa como un importante marcador en el enfermo crítico. Finalmente, después de presentar un esquema de los desarrollos actuales para mejorar el conocimiento del balance oxidativo de los órganos individuales, destacamos la importancia de una estrategia sinóptica de monitorización de O2, así
Palabras clave: oxígeno, monitorización, enfermedad crítica.
Oxygen transfer from atmosphere to mitochondria, and back
The cardio-respiratory system provides the infrastructure for the transport of metabolic substrates to and from the capillary beds where cells can perform effectively. Cells are strategically well positioned at the supply-demand interface, presenting a maximal surface area for the exchange of metabolites, and represent the basic functional physiological unit, as they possess the mitochondrial machinery for energy production as well as all other organelles enabling them to perform the functions of life. Oxygen (O2) is of vital importance for the efficient running of these processes.
«Cellular respiration» neatly describes the molecular processes on the final common pathway of O2 following its journey from atmosphere to mitochondria. On this long and complex route, O2 is moved through conducting airways, exchanged against carbon dioxide (CO2) in the lungs along opposing diffusion gradients on either side of the red blood cell membrane (O2-uptake), bound to haemoglobin and convectively transported in the major blood vessels to the tissues, there it diffuses and is distributed in the tissues. The variable fraction of O2 finally taking part in oxidative phosphorylisation to generate adenosine triphosphate (ATP) is the effective oxygen delivery (DO2) for the cells. The arterio-venous difference of 2 describes its extraction from DO2 depending on the level of O2-demand (VO2).
Metabolic autoregulation of the cell
Oxidative ATP production is a highly efficient process governed by metabolic autoregulation of the cell: the cumulative cellular metabolic performance signals a level of VO2-requirement; this global VO2, in turn, is the cellular feedback parameter creating the set point for a minimal DO2 sufficient to satisfy metabolic demand.
Pflüger was the first to realise the feedback hierarchy –cellular requirement > VO2 > DO2– as early as 1872. He described how it was not only the task of the cardio-respiratory system to act as the logistic conduit for substrates of metabolism, but also, and more importantly, that the oxygen requirement of the cells was the paramount regulator of cardio-respiratory physiology: «Herein lies the predominant secret of the regulation of the amount of oxygen consumed by the whole organism, determined only by the cell itself; ( ) arterial oxygen content, aortal pressure, velocity of blood stream, mode of respiration are all incidental and subordinate, they all combine their actions in the service to the cells.»1.
Oxygen supply and demand
Respiration is a tidal process, DO2 and VO2 have to be constantly balanced and energy is permanently generated, chemically bound in and released from its molecular storage form of ATP. Tissue hypoxia ensues when this balance (DO2/VO2) is disturbed and oxygen consumption outstrips delivery. Oxidative phosphorylation stalls, cellular stress programmes are triggered and anaerobic oxidisation occurs. The inefficient anaerobic generation of ATP is quickly exhausted and leads to the development of lactic acidosis representing, and in turn, further worsening, global cellular dysfunction. As tissue hypoxia constitutes one of the most important co-factors of multiorgan failure (MOF)2, it serves to illustrate the paramount regulatory function of the cell in its strategic frontline position.
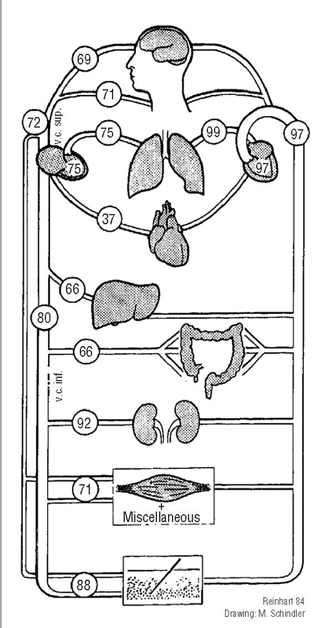
Of all metabolic substrates, O2 has the highest percentage of extraction and O2-reserves are exhausted within a few minutes3. While this physiological fact renders O2, together with its immense biological importance, a very precious commodity, the phenomenon also promotes measurement of arterial and venous O2-saturation as a highly effective clinical tool to monitor the cardio-respiratory system. Different organ systems display heterogenous oxygen extraction levels, representing their differential metabolic activity as well as their respective position in various capillary zones of the circulation together with the unhomogenous share of cardiac output (CO) they receive per unit weight. The spectrum of venous saturation figures for different organs is, therefore, wide already under physiological conditions (fig. 1) and can be further varied by pathophysiological adaptation.
Figure 1. Average percentage figures of
physiological arterial (right) and venous (left)
oxygen saturation of various organ regions: their
heterogenous O2-extraction levels explain the wide
venous O2- saturation spectrum.
Venous oximetry
The two principal sources for venous oximetry at the bedside are either a pulmonary artery catheter (PAC) or a central venous catheter, generating mixed (SvO2) and central venous saturation (ScvO2) measurements, respectively. ScvO2 is clinically more readily available as it is less invasive. It forms a constituent part of SvO2, rendering the true mixed venous saturation the more representative indicator of global tissue oxygenation. As various organs display physiological differences in DO2/VO2, and DO2 as well as VO2 can both individually fluctuate acutely under pathophysiological conditions, SvO2 does not yield information on oxygen reserves or adequate tissue oxygenation of individual organs. Furthermore, several disease states, such as hepatic failure or severe sepsis leading to arterio-venous shunting, limit the interpretation of absolute SvO2 values as indicators of tissue oxygenation. Here, normal or even supranormal SvO2 levels can co-exist with severe tissue hypoxia. This is also possible for conditions disturbing the unloading of oxygen from haemoglobin through left shift of the oxygen dissociation curve or blockage of the respiratory chain, such as in cyanide poisoning and, less well defined, in distributive, for example septic shock.
In 1870, Fick explored the relationship between CO, global oxygen demand and oxygen extraction and stated that «total uptake or release of any substance by an organ is the product of blood flow to the organ and the arterio-venous concentration difference of the substance» (Ficks principle)4. As O2 is in global cellular demand and the whole CO passes the entire cardio-respiratory system, mathematical rearrangement of the physiological equation deducing VO2 illustrates the clinical usefulness and monitoring potential of SvO2: VO2= CO ×(CaO2 - CO2) [Ficks principle]vCO = VO2/(CaO2 - CO2) ~ CO = VO2/13.4 ×Hb ×v(SaO2 - SO2) and hence: v~ SO2 - (VO2/CO) ×k
In other words: for a given VO2, SvO2 represents the supply-demand ratio of oxygen. A DO2/VO2 imbalance indicates mismatch: in clinical terms, shock. Notwithstanding some methodological limitations, as with all technology, venous oximetry provides extremely useful information for the evidence-based evaluation of the critical global oxidative balance and, therefore, makes for a good monitor.
Validity and history of haemodynamic monitoring
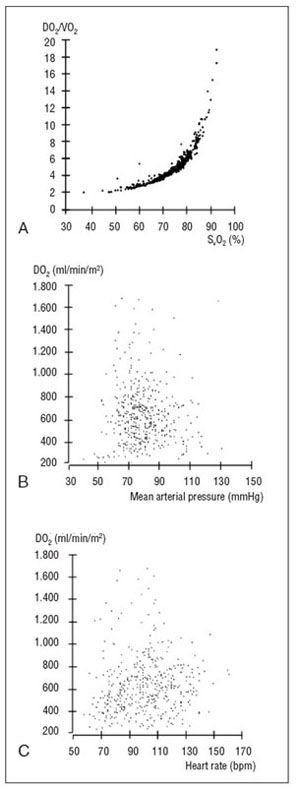
Sophisticated monitoring greatly enhances speed and quality of diagnosis and allows to guide and control therapy, provided it is based on validated parameters. The Latin monitor translates as I am being warned/reminded. Critical synoptic analysis of the correlation coefficients of the haemodynamic parameters SvO2, mean arterial pressure (MAP) and heart rate (HR) for DO2/VO2 (fig. 2) demonstrates that while the first is a reliable warning sign of oxidative imbalance, the latter two are no reminders of oxygen delivery.
Figure 2. Critical synoptic analysis of the
correlation between the haemodynamic
variables mixed venous oxygen saturation
(SvO2) (A), mean arterial blood pressure
(MAP) (B), as well as heart rate (HR) (C) and
oxygen supply/demand (DO2/VO2) reveals
that SvO2 accurately reflects oxidative
balance while the most frequently measured
parameters MAP and HR deliver the least
information on O2- transport and cellular
oxygenation.
The most frequently measured monitoring parameters deliver the least information on oxygen transport and cellular oxygenation. In the cellular regulation framework of cardio-respiratory pathophysiology, however, evidence of O2-transport and requirements carries the highest validity, as information on the oxidative state of the cells most closely reflects their bioenergetic status, and those surrogate parameters, in turn, indicate most accurately what constitutes «critical» illness.
While MAP, especially if measured directly arterially, remains a valuable clinical parameter and firmly established in haemodynamic monitoring, a further problem of validity arises with its use. In 1928, Jarisch pointed out that «for the development of the science of circulation it was fateful that it is comparatively so awkward to measure flow, yet so easy to measure pressure: this is why the blood pressure manometer gained almost fascinating influence, while most organs do not require pressure, but flow volume»5.
The second half of the twentieth century ushered in an era of wider distribution and greater understanding of monitoring technology for the reduction of morbidity and mortality, stimulated particularly by anaesthesiological practice in peri-operative and intensive care medicine. Pulse oximetry (SpO2) for the continuous, real-time measurement of peripheral arterial oxygen saturation, as well as capnography (respiratory [end-tidal] CO2-monitoring, ETCO2) are noninvasive and have both proven so significant as to have been promoted into the rank of obligatory monitoring standards for the safe conduct of clinical anaesthesia.
The carbon footprint of cellular respiration
CO2-monitoring offers a perspective of demand orientation not dissimilar to that of venous oximetry, as the amount of carbon dioxide produced (VCO2) for oxygen consumed are intrinsically linked through the respiratory quotient: RQ = VCO2/VO2. The RQ describes the carbon footprint of oxidative phosphorylisation depending on the substrates used for ATP-pro-duction; for a diet of pure carbohydrates the RQ is 1 as the exothermic conversion of glucose (C6H12O6) with oxygen produces equimolar quantities of carbon dioxide (and water [H2O]): C6+ 6O2 =6CO2 +H12O6 6H2O + Δheat. As the average diet in the industrialised world consists of a mix of carbohydrates (50%), fatty acids (30%) and proteins (20%) as sources for energy conversion, and the caloric value of fats and proteins is higher than that of sugar, the mean RQ of a healthy male European (75 kg) at rest is approximately 0.8, that is 200 ml/min of CO2 generated for 250 ml/min of O2 consumed (basal metabolic rate). Looking at the substrate-specific conversion formula for oxygen is instructive in several ways. It sheds light on the alveolar gas exchange where, on the one hand, water and heat serve to humidify and warm the gases, O2 and CO2, taking part; on the other, however, CO2 and water vapour, along with nitrogen, occupy volume that cannot be used for optimised alveolar O2-uptake (Boyles law of partial pressures). The disturbance of the evolutionarily old pulmonary unit, filled with high concentration nitrogen displaying a splinting effect, and protected by the physicochemical properties of water on the alveolar fluid-gas interface with low-concentration CO2 and mediumconcentration O2, partially explains the detrimental long-term consequences of the exposure of the lungs to high O2-concentrations by way of denitrogenation, with the therapeutic intent to maximize SaO2. Exceeding a threshold of the fractional concentration of inhaled O2 (FiO2), in addition, has a negative feedback impact on the CO. Trying to increase the effective DO2 can thus paradoxically lower it. While a synoptic analysis of O2-monitoring including capnography is, therefore, highly desirable, diet-dependency of the RQ represents only one of the methodological problems for the indirect monitoring of O2-supply-demand adequacy via CO2-monitoring. The elegant idea of gauging dysoxia via PCO2 gradients (ΔPCO2) provides the basis for gastro-intesti-nal tonometry, one of the few clinical tools presently available for the monitoring of tissue oxygenation6. At first regarded as a promising candidate for the early detection of dysoxia and regional hypoperfusion, critical concerns about methodological inaccuracies7 suggest a reduced, albeit still valuable role of ΔPCO2 for the monitoring of the microcirculation only. However, as it cannot reliably detect anaerobic metabolism when flow is preserved, gastro-intestinal tonometry fails to reflect the oxygen supply dependency during hypoxic episodes witnessed under conditions of oxidative stress in the critical vascular bed of the gut. Nevertheless, additional surrogates of impaired oxygen supply to peripheral tissues, such as ΔPCO2 or plasma disappearance rate of indocyanine green (PDRicg)8, help to widen the scope of the global oxygenation parameter S(c)vO2, adding valuable information on individual organ regions.
Levels and levers of pathophysiological adaptation
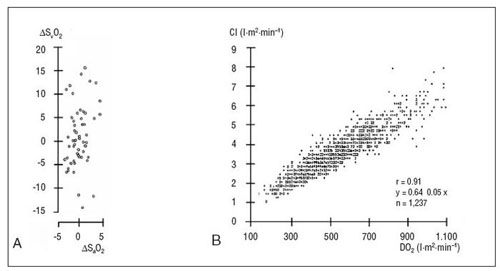
When the variation of SO2 (ΔSO2) is correlated to that of SO2(ΔSO2) in the critically ill, it becomesapparent that venous saturation fluctuates much more than its arterial equivalent over time (fig. 3), illustrating the functional importance of O2-extraction as well as rendering ΔSO2 the more specific and sensitive parameter to indicate adaptive changes, particularly in times of oxidative stress.
Figure 3. Arterial oxygen saturation (SaO2), cardiac index (CI) and
oxygen extraction, here represented by mixed venous saturation
(SvO2), are the three relevant systemic mechanisms of adaptation
to demand-supply-fluctuations (DO2/VO2). A) Correlation between
the respective variations of saturation ( ΔSvO2/ ΔSaO2) illustrates the
functional importance and monitoring capability of SvO2 as it fluctuates
much more than SaO2. B) Tight positive correlation of DO2 and CI marks
their physiological interdependence.
Optimisation of arterial O2-saturation, variation of CO and adaptation of oxygen extraction are the three relevant systemic mechanisms to adjust the organism to fluctuations in DO2/VO2; they present themselves at the same time as therapeutic levers for haemodynamic management.
Without evidence of venous saturation, cardio-res-piratory monitoring, based solely on the measurement of heart rate and rhythm, arterial blood pressure and oxygen saturation, central venous pressure and CO, be it invasive or non-invasive, is half blind. Information on oxygen supply does not answer the decisive question whether it is sufficient to meet cellular oxygen demand. While clinical monitoring that allows the satisfactory quantification of the bioenergetic status of the cells is still some way off, it is all the more regrettable that venous oximetry has not yet attained the position befitting a global monitoring parameter of such relevance and importance.
In view of the astonishing technological progress revolutionizing the generation, acquisition, processing, display and analysis of monitoring information, it is important not to forget the original meaning of «monitor» as an aid supporting the human decision-making process. The first Harvard criterion for good monitoring practice is, therefore, the constant presence of adequately qualified anaesthesia personnel throughout the course of any anaesthetic intervention. «Keeping a finger on the pulse» means just that.
SVO2 and SCVO2 – not identical, but functionally equivalent
While SvO2 is the true mixed venous parameter, indicating global oxidative balance and correlating best with DO2/VO2, ScvO2 is its constituent part and as such only representative of the organs of the upper body. At the same time, ScvO2 measurements are less invasive and widely and quickly attainable in clinical reality; SvO2 necessitates an intensive care environment. Frequently, neither the time nor the place for PAC-dependent monitoring are available.
What is more, PAC usage, per se, has been shown not to affect outcome in critically ill patients9, whereas the implementation of treatment strategies that incorporate ScvO2 (or SvO2, where available) monitoring as part of a dynamic monitoring philosophy along the lines of bioenergetic cellular integrity have succeeded in reducing their mortality considerably10-14.
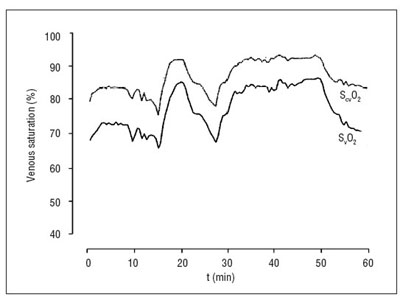
«Critical illness» can be defined as a state of disease that threatens the life of a patient by endangering the function of one or more vital organ systems. Tissue hypoxia is a pivotal co-factor of multi-organ dysfunction syndrome (MODS), and venous oximetry, therefore, well suited to describe this situation. Critical, in this context, is not only the biographic nadir as such, but also the narrowness of the window of opportunity and with it the timing of therapeutic interventions: sub-stratification analysis of haemodynamic strategy in high-risk patients15 reveals that optimisation attempts are futile once organ failure is firmly established. ScvO2 serves as an early warning sign for the developing shock entity; it has the potential to drag cryptic shock out into the open. It allows the monitoring of the critical oxidative balance in the decisive period before both MODS and a PAC are established on the intensive care unit. Herein lies the beauty and main advantage of ScvO2 over SvO2. The long-running discussion about the equivalence of SvO2 and Shas been addressed in severalcvO2 studies16-18. These have illustrated ScvO2 and SlevvO2 els to be numerically different, yet consistently parallel. Recognising a discrepancy of absolute numbers is primarily of academic interest when their correlation is tight and, as a consequence, their physiological trend patterns are equal as demonstrated in animal studies19as well as human clinical observations20(fig. 4). «Mixed vs central venous oxygen saturation may be not numerically equal, but both are still clinically useful»21 was the the blunt title of a recent editorial summing up conclusively the supposed dilemma of lack of absolute congruence between ScvO2 and SvO2.
Figure 4. Simultaneous registration of SvO2 and ScvO2;
numerically different, consistently parallel, functionally equivalent.
Significance of venous saturation monitoring
It is of much greater value for the clinician to know to what extent CO and SO2 are able to meet the oxygen requirements of the capillary beds dictated by global cellular VO2 (Pflüger) than just to know the supply side values in isolation, and nowhere more so than in critically ill patients constantly threatened or affected by MOF.
In addition, valuing trend lines over absolute figures is an important principle of clinical measurement where biosensitive systems have to be calibrated often by multi-point analysis to detect and correct shift and drift, as well as in biostatistics where only a satisfactory quantity of data allows the description of a phenomenon as a trend or correlation in the first place.
Continuous measurements display real-time trends on-line and lead, as a consequence, to more sensitive and powerful monitoring data records than the discrete numbers generated by intermittent gathering of reference points. This is of particular importance for the close, accurate and precise monitoring of episodically and unforeseeably fluctuant parameters such as DO2 and VO2. As VO2 exerts a physiological feedback on DO2, it is instructive to measure and correlate them both. If an increase in DO2, that is a raised CO, leads to a relevant increase in VO2, then this O2-flux test indicates the improvement of a previously inadequate tissue oxygenation22.
Altogether, there can be no doubt that the benefits of (trend analysis of continuous) ScvO2-monitoring by far outweigh the slight, predominantly academic and clinically irrelevant discrepancy in absolute numerical values when compared to SvO2.
Deduction from Ficks principle elucidated the role of SO2 as a functional monitoring parameter for the critical estimation of the global balance of DO2 and VO2. Three components of the equation (balance, supply, demand) on one side find their numerical expression in the venous saturation on the other.
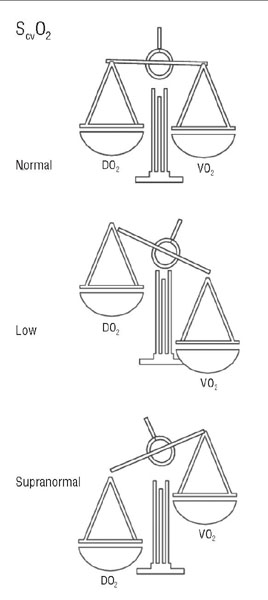
Oxidative balance in the critically ill is represented by a S(c)vO2 level of 70%. If oxygen demand outstrips supply the saturation scales are slanting towards tissue hypoxia - S(c)vO2 figures less than 65% are an early and urgent warning sign pointing towards development of MODS and shock. The (physio)logical interpretation of S(c)vO2 levels exceeding 75% is that of a reverse imbalance with DO2 greater than VO2 (fig. 5). As long as all metabolic requirements are being met, this imbalance is irrelevant: supranormality accounts for physiological reserve. Not so in shock, though, where insufficient metabolic performance is the very defining, pathognomonic feature. The patients maximal oxygen uptake and metabolism (VO2[max]) cannot fulfill the acutely increased mitochondrial requirements in critical illness. Supranormal venous saturation in this context cannot be regarded as a useful or luxury reserve. Rather, it represents a desperately needed, yet unused resource.
Figure 5. Disease-induced oxidative stress in
critical illness: oxidative balance (ScvO2 70%)
indicates an adequately raised DO2 in response
to an increased VO2. Tissue hypoxia ensues when
VO2 outstrips DO2: ScvO2 < 65%, an urgent warning
sign. Supranormality is a marker of poor prognosis too,
as it highlights a reverse imbalance (ScvO2 > 75%): VO2
cannot be adequately up-regulated to satisfy cellular
metabolic requirements and is outweighed by a raised DO2.
Focussing on the supply side alone does not meet excessive demand requirements. The balance is not right: oxygen uptake is too low, indicating either shunts forming at the level of the micro-circulation (effective DO2 too low) or highlighting the inability of the mitochondria to pass electrons through the respiratory chain, that is a utilisation disturbance (effective VO2 too low)23.
Cardio-pulmonary exercise testing (CPET) pro-vides a constructive analogy, as it is a clinically validated protocol stratifying at-risk-patients into categories with prognostic relevance based on their capacity to mount a measurable response (VO2[max]) to a potentially life-threatening situation of oxidative stress (major surgery). A patient presenting with signs of MODS is, in contrast to the elective setting of CPET, a medical emergency and necessitates a robust and streamlined approach. ScvO2 is currently the best evidence-based parameter to guide and monitor the direction of treatment strategies in critical illness towards the goal of an adequately raised DO2/VO2 ratio dynamically balanced on the level of a higher metabolic set point as dictated by the disease-induced surge in oxidative stress.
Between a rock and a hard place: a safety corridor of ScvO2-values
This is why ScvO2 is a cornerstone of an outcomeoriented algorithm such as early goal-directed therapy (EGDT) as a constituent part of the Surviving Sepsis Campaign. Furthermore, obtaining a specimen for blood gas analysis to establish a ScvO2 in the critically ill should be a primary motivation when indicating the need for the placement of a central venous catheter. What is more, persistent signs of tissue hypoxia should then prompt continuous monitoring of the SO2, underpinning its importance as an end point of critical and early prognostic, diagnostic and therapeutic significance.
In a series of 205 patients undergoing elective cardiac surgery we observed a similar hypoxic burden as indicated by increased lactate levels (> 4 mmol/l) along with comparable morbidity and mortality in patients with ScvO2 measurements below 65% as well as above 75%, respectively (own unpublished observation). These data suggest a three-tiered sub-stratifica-tion along ScvO2 cut-off points gained by trend analysis of continuous measurements: while the well oxygen-balanced patient cohort had the best chances of survival, both cohorts with ScvO2 values falling outside a «corridor of safety» of 70 ± 5% performed significantly worse and similarly to each other.
Importance of a synoptic monitoring strategy of O2 in dynamic equilibrium
Contemporary oxygen monitoring is sophisticated, universally available and yields important information to put intensive care for the critically ill on a sound and solid evidence base as an eminent part of a synoptic evaluation strategy for a substrate in dynamic equilibrium. Despite its great significance, (patho)physiological plausibility and clinical practicability, venous oximetry is not used to its full potential yet.
Additional surrogates of impaired oxygen supply to individual organs and functional cellular units, such as PDRicg or gastro-intestinal tonometry, are technically achievable and clinically available today at least for some capillary beds. The near future will see the introduction of more devices for the specific surveillance of organs and their functions in relation to their individual DO2, VO2, their respective interaction and further important O2-dependent variables. These highly desirable instruments for prognostic, diagnostic and therapeutic management of the critically ill threatened or affected by MOF allow a direction of focus away from what Pflüger so poignantly defined as «incidental and subordinate».
The challenge today is to move on from this state of affairs and to raise understanding of the existing possibilities of O2-monitoring and its significance for survival of the critically ill, characterised by a heterogeneity of outcome which has less to do with access to high-tech medicine than with the will to consequently implement, at local level and into clinical routine, what has to be regarded as best practice at the present time.
Venous oximetry should play the role of the first violinist in the orchestrated approach necessary to do justice to the complex and dynamic network of interactions that classifies oxygen metabolism and its clinical monitoring as a symphony constantly in the making –or breaking– in the critically ill patient.
Conclusion
The cardio-respiratory system provides the infrastructure for the transport of O2 from atmosphere to mitochondria, and back. Global cellular requirement determines effective VO2, setting the point for a minimally sufficient effective DO2. The cell is at the top of the feedback hierarchy of metabolic autoregulation. Tissue hypoxia ensues when global and/or individual organ DO2/VO2-balance are disturbed; it constitutes one of the most important co-factors of MOF with highly significant morbidity, mortality and cost implications for the critically ill. Of all metabolic substrates, O2 has the highest percentage of extraction. It is further characterised by heterogenous organ saturation levels and a quickly exhaustable reserve. This dynamic equilibrium promotes monitoring of arterial and venous O2-saturation as a very effective clinical tool. Arterial O2-saturation is routinely monitored invasively (SaO2) or non-invasively (SpO2); in contrast to that, venous oximetry is not used as consistently or effectively. There are two principal sources for venous oximetry: SvO2 and S. SvO2 is cvO2 the more representative indicator of global tissue oxygenation; ScvO2, however, is less invasive and more readily available (they are not identical, but functionally equivalent). Both represent the supplydemand ratio for O2 and, therefore, provide highly significant evidence for the critical synoptic analysis of cardio-respiratory monitoring data. Unfortunately, the most frequently measured haemodynamic parameters -arterial blood pressure and HR- deliver the least information on cellular oxygenation. Furthermore, a multi-modal O2-monitoring approach elucidates the useful function of CO2-monitoring with its perspective of demand orientation similar to that of venous oximetry; VO2 and CO2-flux (VCO2) are intrinsically linked through alveolar ventilation in the respiratory quotient: RQ = VCO2/VO2. Optimisation of SO2, variation of CO and adjustment of oxygen extraction (ΔS(c)vO2) are the three relevant systemic physiological mechanisms of adaptation as well as therapeutic levers for haemodynamic management. They are half blind without evidence of venous saturation, as it is much more important to establish to what extent CO and SO2 are able to meet oxygen requirements than just to know the supply side values in isolation. In the critically ill, sustained ScvO2 levels below 65% indicate ineffective DO2 while those above 75% characterise an ineffective VO2, with a safety corridor of 70 ± 5% in between. ScvO2 is currently the best evidence-based parameter to guide and monitor treatment strategies of patients threatened or affected by MOF. Obtaining ScvO2-values should be a primary motivation when indicating the placement of a central venous catheter. Contemporary, multimodal O2-monitoring is sophisticated, widely available and (patho)physiologically highly relevant. Despite its great clinical significance, plausibility and practicability, it is not yet used to its full potential. Additional surrogates of impaired oxygen supply to individual organs are promising more conclusive answers to the supply-demand question: micro-circula-tory insufficiency or utilisation disturbance? at the mitochondrial level as the final common pathway of O2-metabolism.
References
1. Pflüger EFW. Über die Diffusion des Sauerstoffs, den Ort und die Gesetze der Oxydationsprozesse im tierischen Organismus. Arch Gesamte Physiol. 1872;6:43. [ Links ]
2. Marshall JC. Inflammation, coagulopathy and the pathogenesis of multiple organ dysfunction syndrome. Crit Care Med. 2001; 29(7 Suppl):S99-106. [ Links ]
3. Reinhart K, Schäfer M, Rudolph T, Specht M. Mixed venous oxygen saturation. Applied Cardiopulm Pathophys. 1989;2:315-25. [ Links ]
4. Fick A. Über die Messung des Blutquantums in den Herzventrikeln. Sitzungsber Phys Med Ges Würzburg. 1870;BdII:XVI. [ Links ]
5. Jarisch A. Kreislauffragen. Dtsch Med Wochenschr. 1928;29: 1211-3. [ Links ]
6. Third European Consensus Conference in Intensive Care Medicine: Tissue hypoxia: how to detect, how to correct, how to prevent? Am J Respir Crit Care Med. 1996;154:1573-8. [ Links ]
7. Dubin A, Murias G, Estenssoro E, Canales H, Badie J, Pozo M, et al. Intramucosal-arterial PCO2 gap fails to reflect intestinal dysoxia in hypoxic hypoxia. Crit Care. 2002;6:514-20. [ Links ]
8. Sakka SG, Reinhart K, Meier-Hellmann A. Prognostic value of indocyanine green plasma disappearance rate in critically ill patients. Chest. 2002;122:1715-20. [ Links ]
9. Harvey S, Harrison DA, Singer M, Ashcroft J, Jones CM, Elbourne D, et al. Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomized controlled trial. Lancet. 2005;366:472-7. [ Links ]
10. Kortgen A, Niederprüm P, Bauer M. Implementation of an evidence-based standard operating procedure and outcome in septic shock. Crit Care Med. 2006;34:943-9. [ Links ]
11. Otero RM, Nguyen HB, Huang DT, Gaieski DF, Goyal M, Gunnerson KJ, et al. Early goal-directed therapy in severe sepsis and septic shock revisited: concepts, controversies, and contemporary findings. Chest. 2006;130:1579-95. [ Links ]
12. Nguyen HB, Corbett SW, Steele R, Banta J, Clark RT, Hayes SR, et al. Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit Care Med. 2007;35:1105-12. [ Links ]
13. Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, et al. Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32: 858-73. [ Links ]
14. Shapiro NI, Howell MD, Talmor D, Lahey D, Ngo L, Buras J, et al. Implementation and outcomes of the Multiple Urgent Sepsis Therapies (MUST) protocol. Crit Care Med. 2006;34:1025-32. [ Links ]
15. Kern JW, Shoemaker WC. Meta-analysis of hemodynamic optimization in high-risk patients. Crit Care Med. 2002;30:1686-92. [ Links ]
16. Chawla LS, Zia H, Gutiérrez G, Katz NM, Seneff MG, Shah M. Lack of equivalence between central and mixed venous oxygen saturation. Chest. 2004;126:1891-6. [ Links ]
17. Dueck MH, Klimek M, Appenrodt S, Weigand C, Boemer U. Trends but not individual values of central venous oxygen saturation agree with mixed venous oxygen saturation during varying hemodynamic conditions. Anesthesiology. 2005;103:249-57. [ Links ]
18. Tahvanainen J, Meretoja O, Nikki P. Can central venous blood replace mixed venous blood samples? Crit Care Med. 1982; 10:758-61. [ Links ]
19. Reinhart K, Rudolph T, Bredle DL, Hannemann L, Cain SM. Comparison of central-venous to mixed-venous oxygen saturation during changes in oxygen supply/demand. Chest. 1989;95: 1216-21. [ Links ]
20. Reinhart K, Kuhn HJ, Hartog C, Bredle DL. Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004;30:1572-8. [ Links ]
21. Rivers E. Mixed venous vs central venous oxygen saturation may not be numerically equal, but both are still clinically useful. Chest. 2006;129:507-8. [ Links ]
22. Reinhart K, Hannemann L. Klinische Einschätzung der Gewebeoxygenierung. Anaesthesiol Reanimat. 1991;16:184-201. [ Links ]
23. Bauer P, Reinhart K, Bauer M. Early goal-directed therapy and outcome in septic shock. Int J Intensive Care. 2007;14:19-23. [ Links ]
![]() Correspondence:
Correspondence:
Dr. M. Bauer.
Department of Anaesthesiology and Critical Care Medicine.
Friedrich-Schiller-University.
07740 Jena. Germany.
E-mail: Michael.Bauer@med.uni-jena.de
Manuscript accepted on 19-X-2007.