INTRODUCTION
Liver transplantation is the treatment of choice for patients with end-stage liver disease with the purpose of improving survival and quality of life. Data of the Brazilian Association of Organ Transplantation 1 have shown an increase in the performance of liver transplantation in Brazil. Only during the months from January to September of 2015, 1,326 transplants were performed.
Nutritional changes may influence on the process of liver transplantation, appearing as an independent risk factor for the patient's stay in the intensive treatment unit and total days of hospitalization, and increasing the complications and mortality in these patients. Adequate nutritional status and food intake are very important both to improve the general condition of the patient candidate for liver transplantation and for a good recovery after surgical trauma 2.
Insufficient or excessive consumption of foods causes widely described damage; however, there is evidence that diet quality characteristics are important in defining health status, particularly with regard to chronic degenerative diseases of adulthood 3.
Thus, better research is necessary in this context, since knowledge of dietary habits and nutritional risk factors associated with this disease are essential for therapeutic strategies aimed at improving the quality of life of this population. The aim of this study was to investigate the influence of liver transplantation in the anthropometric profile and consumption of nutrients in cirrhotic patients.
METHODS
STUDY CHARACTERIZATION
The study is a clinical uncontrolled trial type and was held at the ambulatory of nutrition, Liver Transplant Center, of the Hospital Walter Cantídio Complex in Fortaleza in the period from July 2013 to September 2015. The sample consisted of 23 patients, aged 18 to 65, who were assessed before and three months after liver transplantation in relation to nutritional and anthropometric aspects. The sample size was based on the number of patients in whom tracking was possible. The sample size was calculated considering the following criteria: number of patients who underwent liver transplant in 2012, which was equal to 127, proportion that is expected to be found of individuals with inadequate nutrient intake (50%), and sampling error of 15% and 90% of confidence level. Thus, it was determined that the sample size of this study should be 24 participants. This study was approved by the Ethical Committee of the State University of Ceará (CAAE No 15503213.2.0000.5534) and written consent was obtained from all participants.
DATA COLLECTION
The sociodemographic and clinical data of patients were collected from their charts, including age, sex, origin, ethnicity, schooling, family income, clinical diagnosis, associated pathologies, history of family diseases, blood type, model for end-stage liver disease (MELD) score and Child-Pugh classification. Nutritional and anthropometric data were obtained through interviews and evaluation of individuals in the two periods of work.
ANTHROPOMETRY
Weight, height, arm circumference (AC), abdominal circumference (AbC), triceps skinfold (TSF), biceps skinfold (BSF), subscapularis skinfold (SSSF) and suprailiac skinfold (SISF) were measured in triplicate. Body weight was measured by a scale (Filizola(r) Digital Scale, São Paulo, Brazil) with capacity of 150 kg and precision of 0.1 kg. Height was determined using a stadiometer (1 mm precision) attached to the scale, according to previously described procedures 4. Patients with edema or ascites had their weight discounted according to James 5 and Duarte and Castellani 6. Body mass index (BMI) was calculated and classified according to the World Health Organization criteria (WHO) 7) (8.
The skinfolds were measured on the right side of the body using a Lange(r) adipometer (0.5 mm precision) according to previously described procedures 4. AbC and AC were measured with an unstretched tape measure. AbC was determined at umbilical scar level at the end of normal expiration. AC was measured at the midpoint between the acromial process of the scapula and the olecranon, with the arms loose along the trunk and the hands facing the thigh. The muscle arm circumference (MAC) was calculated according to the following formula: MAC (cm) = AC (cm) - 3.14 x (TSF (mm)/10).
The percentages of adequacy of AC, TSF and MAC were also calculated comparing the results found with the reference values proposed by the National Health and Nutrition Examination Survey using percentile tables 9. Adequacy percentages were classified according to Blackburn and Thorton 10. The percentage of body fat was obtained through the formula proposed by Siri 11, which considers body density estimated from the sum of TSF, BSF, SSSF and SISF. This measure was classified according to Lohman et al. 12. The values obtained from AbC were classified based on the International Diabetes Federation criteria 13.
ASSESSMENT OF FOOD INTAKE
The food intake evaluation was carried out by collecting three food 24-hour recalls of three non-consecutive days, including one weekend day. The energy needs of each individual were calculated based on the estimated energy requirement (EER), proposed by the Institute of Medicine 11. Macronutrients and fat-soluble vitamins were qualitatively evaluated considering the consumption above, within or below the recommended according to the cut-off values recommended by the Institute of Medicine 14) (15) (16) (17.
STATISTICAL ANALYSIS
The statistical analysis of this study was performed using SPSS version 17.0. Data were expressed as frequencies, percentages, means and standard deviations. Data normality was tested using the Kolmogorov-Smirnov test and homogeneity of data, using the Levene's test. The paired Student's t-test was used to compare the means of food consumption and anthropometric variables before and after transplantation. The McNemar and McNemar-Bowker tests were used to compare the proportions of individuals categorized according to the food consumption and anthropometric classifications before and after the transplantation, when the categories were dichotomic and polytomic, respectively. To investigate correlations among variables, a Pearson's correlation test was conducted. Data were considered as significant with p values below 0.05.
RESULTS
Most participants were female (52.2%), aged 40 to 65 years, from northeastern Brazil (where the survey was conducted), brown race or mulatto mainly (65.21%), with High School completed and household income of about one to five minimum wages (Table I). The blood type 0 prevailed among most patients (47.9%), with Child-Pugh B score between 7 and 9 (47.8%) and MELD score between 20 and 24 (78.3%). Viral hepatitis was the most frequent underlying disease, including hepatitis C, which was present in 34.78%, and hepatitis B, in 8.6% of the study population. Hypertension was the disease associated with clinical diagnosis of cirrhosis that affected more patients (17.4%) and was more prevalent in family history (73.9%) (Table II).
Table I Sociodemographic characteristics of the study population (n = 23) of severe cirrhotic patients submitted to liver transplant
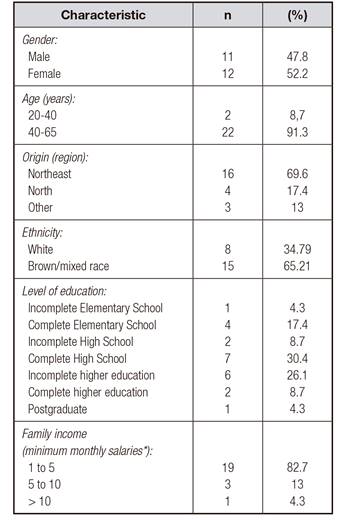
*Value of R$880.00 in 2016, which is equivalent to approximately US$272.00.
Table II Clinical and pathological characteristics of the study population (n = 23) of severe cirrhotic patients submitted to liver transplant
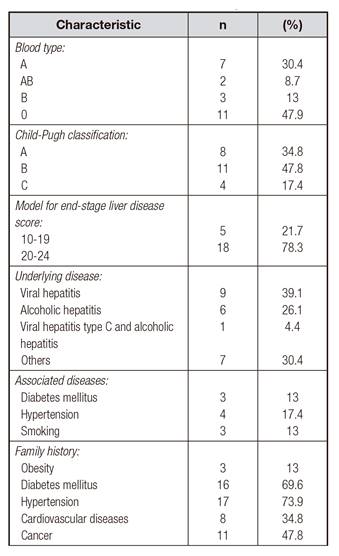
Table III Anthropometric characteristics of the study population (n = 23) of severe cirrhotic patients submitted to liver transplant
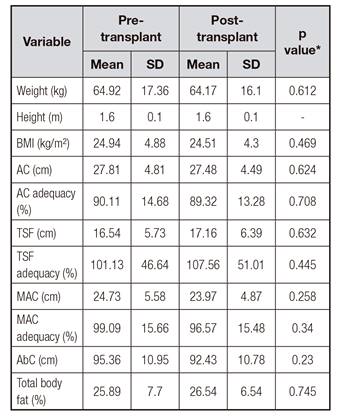
SD: standard deviation; BMI: body mass index; AC: arm circumference; TSF: triceps skinfold; MAC: muscle arm circumference; AbC: abdominal circumference. *Student's t-test for related samples: level of significance set at p ≤ 0.05.
Although the anthropometric parameters showed no statistically significant difference between pre- and post-transplant (Table III), in the proportion comparison analysis a high prevalence of obesity before transplantation (52.17%) and eutrophic after transplantation (56.5%) was observed according to BMI. According to the AC, 52.17% and 56.53% of the participants were malnourished before and after transplantation, respectively. The classification did not changed between the periods in relation to the MAC for most participants, but 82.61% and 56.53% were normal before and after transplantation, respectively. According to the TSF classification, 47.82% of the participants were malnourished before and 52.17% were overweight after transplantation.
The largest proportion of the study participants had body fat percentage above average both before (66.66%) and after transplantation (60%). According to the evaluation of abdominal circumference, 92.85% of patients were at risk for cardiovascular disease due to the accumulation of abdominal fat above ideal on pre-transplant, and this number was reduced to 71.4% after transplantation. There was no significant change between the proportions of classifications of anthropometric parameters before and after transplantation (p > 0.05).
Among nutrients, it was observed that the average consumption of calories, proteins, lipids, cholesterol and monounsaturated fatty acids was significantly higher in post-transplantation than in pre-transplantation (p < 0.05) (Table IV).
Table IV Energy and macronutrient intake of the study population (n = 23) of severe cirrhotic patients submitted to liver transplant
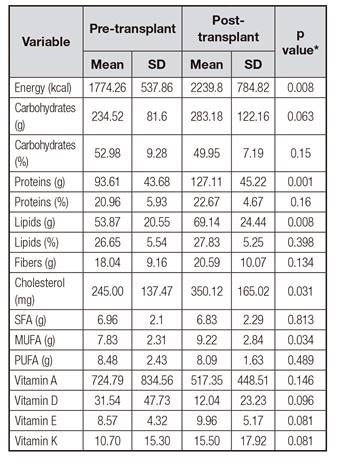
SD: standard deviation; SFA: saturated fat acids; MUFA: monounsaturated fat acids; PUFA: polyunsaturated fatty acids. *Student's t-test for related samples: level of significance set at p ≤ 0.05.
Calorie and fiber consumption was classified as below the recommended, both before (65.22% and 91.30%) and after (91.3% and 82.6%) transplantation for most of the study participants. Regarding the consumption of carbohydrates, proteins and lipids, most of the participants were classified as within the recommended levels both in the pre- (69.57%, 95.70% and 82.60%, respectively) and post-transplant (78.53%, 100 00% and 82.60%, respectively) periods.
Regarding the consumption of lipid fractions, 78% of patients were rated with cholesterol consumption within the recommended values in pre-transplant, but this percentage was reduced in post-transplantation to 47.8%. For saturated and polyunsaturated fatty acids, most participants consumed according to recommended values both before (95.70% and 78.30%, respectively) and after (87.00% and 87.00%, respectively) transplantation. The consumption of monounsaturated fatty acids was lower than recommended for all participants in both periods.
The consumption of vitamins A, D, E and K was lower than recommended for most participants in pre- (95.70%, 60.87%, 95.70% and 100.00%, respectively) and post-transplantation (100.00%, 78.30%, 95.70% and 100.00%, respectively).
There was no significant change between the consumer ratings of the evaluated nutrients in the two periods of work (p > 0.05). There was no significant correlation between energy consumption and anthropometric parameters after transplantation (p > 0.05).
DISCUSSION
The aim of this study was to investigate the influence of liver transplantation on the nutritional status of cirrhotic patients. Although no significant changes in anthropometric ratings or adequacy of nutrients were observed between the periods studied, it was observed that some anthropometric parameters classified most participants as malnourished or overweight after transplantation and that the average consumption of calories, proteins, lipids, cholesterol and monounsaturated fatty acids increased significantly after transplantation.
Most of the participants in this study were between 40 and 65 years old and male. Similar to the study by Boin et al. 18, the most frequent cause of the liver diseases leading to transplantation was hepatitis C virus.
Before liver transplantation, most of the patients in this study had a B score and a score between 20 and 24 according to the Child-Pugh and MELD indices, respectively, which may refer to survival of less than 24 months in 43% of patients and a mortality rate of 76% 19. Tandon et al. 20 observed that severe muscle depletion (more prevalent in males, in patients classified as Child-Pugh class C, and in those with low BMI) is associated with increased mortality of patients on the waiting list for liver transplantation. Testing the association between the anthropometric indicators and the gender or the Child-Pugh and MELD indices with the data of this research was not possible because the sample data did not meet the requirements for association analysis.
Regarding the variations in the classifications of the participants by the anthropometric parameters, there are divergences between the different methodologies, which was also shown in the work of Alves, Mendes and Kruel 21, who found many of their participants in the post-liver transplantation with normal weight according to BMI (41.70%), AC (38.90%) and MAC (69.80%), while malnutrition was more prevalent according to TSF (38.9%).
The study of the prevalence of abdominal obesity in patients undergoing liver transplantation is observed in few studies. Anastácio et al. 22 and Ribeiro et al. 23 showed that 88% and 53.7% of participants, respectively, had some degree of abdominal obesity. These studies reinforce our results, in which patients undergoing transplantation have a body fat percentage and abdominal circumference above the recommended, which may be due to increased energy consumption after transplantation. However, a significant correlation between energy consumption and anthropometric parameters was not seen, probably due to the number of participants.
In relation to food intake, it is assumed that the increase in caloric intake after transplantation is mainly due to improved health and appetite of the patient; return to the diet without restrictions due to the absence of hepatic encephalopathy, edema and ascites; decreased level of physical activity; and the use of immunosuppressants. As this work, Merli et al. 2 proved a significant increase in energy consumption after transplantation.
The consumption of macronutrients was within the recommended values in most patients during the two study periods. The average protein increase is probably due to the increased consumption of meat, milk and its derivatives as seen in the analysis of 24-hour dietary recalls. These foods constitute an excellent source of high quality protein as they contain all the essential amino acids in proportions similar to those required for the synthesis of human tissue proteins. The increase of vegetable oil consumption during food preparation, as well as increased appetite and unrestricted diets, may have also interfered with lipid consumption.
The opposite result was observed by Ferreira et al. 24 in relation to the consumption of proteins, which was inadequate in 72% of patients of their work. However, the percentage of participants with consumption of carbohydrates and lipids was also high.
Fiber consumption below the recommended by the participants of this study can be attributed to low consumption of whole grains, fruits and vegetables, which can influence the cholesterol control, the development of constipation and increased food intake 25.
The consumption of lipid fractions was in line with the recommended for saturated and polyunsaturated fatty acids at the two moments of intervention. Conversely, monounsaturated fatty acids and cholesterol showed a decrease in the proportion of participants with consumption according to the recommended after transplant. However, the average consumption of the latter two was significantly higher after transplantation. Ferreira et al. 24 found similar results in relation to the consumption of saturated and monounsaturated fatty acids, but differ in relation to cholesterol, which was consumed in excess by most participants, and polyunsaturated fatty acids, with consumption below the recommended.
The increase in consumed cholesterol is probably due to increased consumption of foods rich in protein and fat, as observed in the 24-hour recalls, because these foods are similar sources. In the 24-hour recalls the absence of consumption of vegetable oils of good quality, such as olive oil, and other sources such as oleaginous seeds has been observed as well, which may have contributed to the fact that consumption of monounsaturated fatty acids was suboptimal.
The consumption of fat-soluble vitamins below the recommended in the two moments of the study can be explained by the low consumption of fruits and vegetables, which is supported by data of the Family Budget Research 26 that showed low consumption of such foods by the Brazilian population. In addition, participants are advised not to consume raw vegetables after surgery, in order to avoid the risk of contamination.
The liver has an important role in the transport and storage of fat soluble vitamins (A, D, E, K). Insufficient quantities of these vitamins can be related to hepatic dysfunction, and hence changes in the nutritional status 27. It has been reported that vitamin A deficiency is related to hepatitis C and alcoholic cirrhosis 28) (29. Studies have shown that very low concentrations of vitamin D in serum are associated with increased mortality of patients with chronic liver disease and an impaired immune function due to a deficiency of this vitamin has been suggested. Low Vitamin D levels are also associated with worse survival, the degree of hepatic dysfunction and disease severity assessed according to the Child-Pugh score 30) (31.
Vitamin E deficiency has been well documented in alcoholic liver disease. However, the beneficial effect of vitamin E supplementation on liver diseases is dependent on the nature of the disorder 32.
In cholestatic liver diseases or lack of biliary secretion which prevents the formation of chylomicrons, menaquinone and phytoquinones, vitamin K deficiency can be observed, particularly by defect in the absorptive process 33.
As a study limitation, it must be highlighted that three months might not be enough time to observe some metabolic post-transplantation disorders. Therefore, it is suggested that the study be continued, since some studies have reported a year as a time for major changes in nutritional status. In addition, it was not possible to use electrical bioimpedance to evaluate body composition due to the high incidence of ascites and edema in this patients, mainly before transplantation. However, it should be pointed out that the skinfolds evaluation methods used in this research, performed by qualified professionals, are valid and reliable, allowing the analysis of lean mass and fat mass and showing a clear view of the body fat distribution 34.
CONCLUSION
The average consumption of some nutrients was higher after transplantation. There were no changes in nutritional status from the pre to the post-transplant period but, in general, most patients had changes in nutritional status in the two stages, indicating that good guidance and nutrition monitoring is of paramount importance to avoid nutritional risks in order to ensure the success of transplantation and improve survival and quality of life of these patients.














