INTRODUCTION
Cerebrovascular disease (CVD) is characterized by dysphagia (1). The prevalence of dysphagia is 10 % among individuals over 50 years of age - it increases with age and is reported to be 35 % to 50 % in patients with CVD (2,3). The most important changes that may cause dysphagia with increasing age are decreased chewing power because of decreased face muscle strength, tooth loss, decreased saliva production, and low fluid intake (4). In patients with CVD, dysphagia may result in malnutrition, dehydration, penetration, aspiration, pneumonia, and death (5), and may adversely affect an individual's anxiety status and quality of life (6).
In dysphagia, the risk of aspiration increases with age and malnutrition (7). Decreased protein intake due to malnutrition leads to muscle loss, which increases the risk of aspiration, causing a decrease in cough and respiratory power (8). About half of the patients with dysphagia aspirate. Silent aspiration occurs when food goes down the vocal cords without cough. Silent aspiration can be overlooked in clinical tests; therefore, advanced instrumental methods are used to evaluate dysphagia. The fiber-optic endoscopic evaluation of swallowing (FEES) test is the most commonly used assessment tool in clinical practice. Using the FEES test, the anatomical and physiological structures involved in the swallowing phases were examined, and nutritional treatment (NT) strategies were determined using a fiber-optic camera and providing the patient with foods with different bolus consistencies (liquid/semisolid) (9). The evaluation is easy and standardized as it is based on scales. The most commonly used scale is the Penetration-Aspiration Scale (PAS). The degree of dysphagia was determined based on the score obtained in this scale (10).
Nutritional treatment is important to increase swallowing efficacy and safety, one of the basic approaches to dysphagia treatment. Nutritional treatment in patients with dysphagia is based on changes in the amount and density of the foods consumed by the patient after clinical and instrumental evaluation. For patients to swallow these foods without aspiration, they need to eat slowly in a sitting position (11).
This study was planned and conducted to evaluate the effects of NT, which is routinely recommended for patients with dysphagia based on clinical and FEES tests, on the nutritional status and anxiety levels of the patients included. The hypotheses determined for this study may be described as follows - First, there is a relationship between the nutritional status of dysphagia patients and their anxiety levels. Second, nutritional therapy provides an increase in food intake and a reduction in risk of malnutrition in patients with dysphagia.
MATERIALS AND METHODS
THE ETHICAL ASPECT OF THE RESEARCH AND DATA COLLECTION
The Toros University Scientific Research and Publication Ethics Committee approved the study (#43-25.09.2019), and an informed consent was obtained from the individuals who participated in this study. Seventy-five patients over the age of 50, who were diagnosed with CVD and hospitalized at the Mersin City Research and Training Hospital, Neurology Clinic, from October 2019 to January 2020, were followed up for the study. Patients diagnosed with CVD for at least 2 weeks and those with dysphagia who could be fed orally were included, and those who were fed only via enteral nutrition (EN), except for oral enteral support, and total parenteral nutrition (TPN) were excluded. Our study was carried out based on a longitudinal design since we worked with the same units at two different time points.
Consent was obtained from all patients who volunteered to participate in the study. First, a FEES test was administered routinely to diagnose dysphagia, and PAS scores were obtained. Then, anthropometric measurements (height and weight) of the patients were taken to calculate their BMI. To determine their daily food intake, 24-h dietary recalls were taken, the NRS-2002 was used to identify patients at risk of malnutrition, and both State and Trait Anxiety Inventories (SAI and TAI, respectively) were used to determine instant and general anxiety levels. They were informed about the importance of consuming food in an upright position. The amounts of energy, nutrients, and fluids specific for each patient were calculated. NT, as modified based on food consistency, was administered. In the second study visit, which took place 8 weeks after the first interview, anthropometric measurements and 24-h dietary recalls were taken again. The NRS 2002 and SAI-TAI assessments were readministered.
ASSESSMENT OF THE SWALLOWING DISORDER
To standardize the FEES and PAS assessments, evaluations were made by a doctor specialist experienced in laryngology-swallowing conditions. During the FEES test, patients were given food in liquid/semisolid form with green food dye, and their food swallowing was monitored with a fiber-optic camera and scored with the PAS.
PAS is reliable and easy to use. It includes a scoring system that allows to obtain a numerical dysphagia level based on the images obtained via the FEES test. There are eight scores on the scale regarding patient penetration and aspiration severity. Higher scores on the scale indicate a higher severity (1, no-penetration-aspiration; 2-5, penetration; 6-8, aspiration) (12).
EVALUATION OF ANTHROPOMETRIC MEASUREMENTS
The body weights of the participants were measured with a sensitive scale, and their height was measured without stretching. Body mass index was calculated using the formula BMI (kg/m2) = body weight (kg) / height (m2) using their body weight and height. If the value obtained was < 18.5 kg/m2, the subject was underweight; if between 18.5 and 24.9 kg/m2, the subject was normal weight; if between 25.0 and 29.9 kg/m2, the subject was overweight; if between 30.0 and 34.9 kg/m2, the subject was included in obesity class 1; if between 35.0 and 39.9 kg/m2, in obesity class 2; if ≥ 40.0 kg/m2, in obesity class 3 (13).
EVALUATION OF NUTRITIONAL STATUS AND POTENTIAL MALNUTRITION
The NRS 2002 test was used to identify patients at risk of malnutrition. An NRS 2002 score ≥ 3 indicates a nutritional high risk (14). To determine daily food intake, 24-h dietary recalls were taken. The data were entered into the Nutrition Information Systems (BEBIS), and daily energy, macronutrient, and liquid consumption status were determined (15). These data, which were collected at the beginning of the study, were recorded again at the end of the study.
The daily energy requirements of the patients were calculated using a practical formula (20-30 kcal/kg of body weight) (16). Energy calculations in patients with body weight below normal (BMI < 18.5 kg/m2) provided a result of > 25-30 kcal/kg of body weight (16). When assessing the energy requirements of obese patients (body mass index [BMI] of 30 kg/m²), their ideal body weight was calculated (17) as: adjusted body weight = [IBW + (ABW - IBW x 0.25)], with IBW = ideal body weight, amd ABW = actual body weight. Daily protein needs were 1-1.5 g/kg, and daily fluid needs were 30 mL/kg (18). Accordingly, appropriate NTs were given considering the safe consistency patterns that they could receive based on FEES results (11).
ASSESSMENT OF ANXIETY LEVELS
In this study, SAI-TAI were used to determine instant emotional and general anxiety levels. A Turkish adaptation, as well as validity and reliability studies were performed in 1985 (19). These inventories contain short statements (20 each) for self-reporting. The SAI evaluates "instant emotional" anxiety levels, and the TAI evaluates the "general" anxiety status. The score ranges from 20 to 80. Although the scales do not have a definite cut-off point, it is generally accepted that 39-40 points are the cut-off point for anxiety (19). Higher scores indicate increased anxiety (20). These scales, which were administered at the beginning of the study, were repeated at the end of the study.
STATISTICAL ANALYSIS OF THE DATA
In the study, a paired-sample t-test, Pearson's correlation analysis, and a reliability analysis were used. We used Pearson's correlation analysis to assess the relationship between energy, macronutrients, and anxiety scores. Shapiro-Wilks normality tests were conducted for quantitative score variables, and it was observed that normality conditions were met. The reliability of state and trait anxiety scales was evaluated according to Cronbach's alpha coefficients. Analyses were applied by considering the total scores of the scale items. The IBM SPSS 20 software was used for the statistical analyses. In addition, correlation difference tests were used to test differences between correlations. At this stage, the psych package included in the R Project software was used (21).
RESULTS
A total of 75 patients with dysphagia, 24 women (32.0 %) and 51 men (68.0 %), with a mean age of 71.15 ± 10.34 years were recruited. The mean body mass index (BMI) of these patients was 26.14 ± 5.57. Although the mean NRS 2002 score was 2.20 ± 0.86, 31 patients (41.3 %) were found to have a NRS 2002 score ≥ 3. Based on the FEES scores, for liquid nutrients 60 patients (80.0 %) had a PAS score of 2-5, and 15 patients (20.0 %) had a PAS score of 6-8. For semisolid foods 72 patients (96.0 %) had a PAS score of 2-5, and 3 (4.0 %) had a PAS score of 6-8 (Table I).
Table I. General characteristics of patients with dysphagia
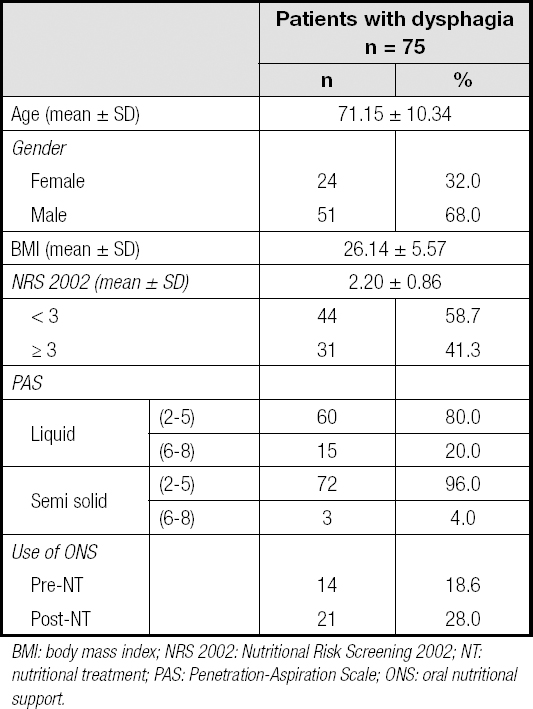
BMI: body mass index; NRS 2002: Nutritional Risk Screening 2002; NT: nutritional treatment; PAS: Penetration-Aspiration Scale; ONS: oral nutritional support.
The comparison of these patients pre- and post-NT based on their PAS scores and rates of meeting their energy and macronutrient needs is shown in table II. According to these results, for liquids there are significant differences between patients with a PAS score of 2-5 and those with a score of 6-8 in terms of the rate of meeting energy, protein, and fluid intake needs pre- and post-NT (p < 0.05). When the scoring for semisolid foods was analyzed pre- and post-NT, there was a significant difference in patients with a PAS score of 2-5 in terms of the percentage that met energy, protein, and fluid intake needs (p < 0.05). There was a significant difference in patients with a PAS score of 6-8 only in terms of their pre- and post-NT fluid intake status (p < 0.05).
Table II. Evaluation of percentages of meeting energy and macronutrients and liquid intake according to PAS in patients with dysphagia before and after nutritional treatment
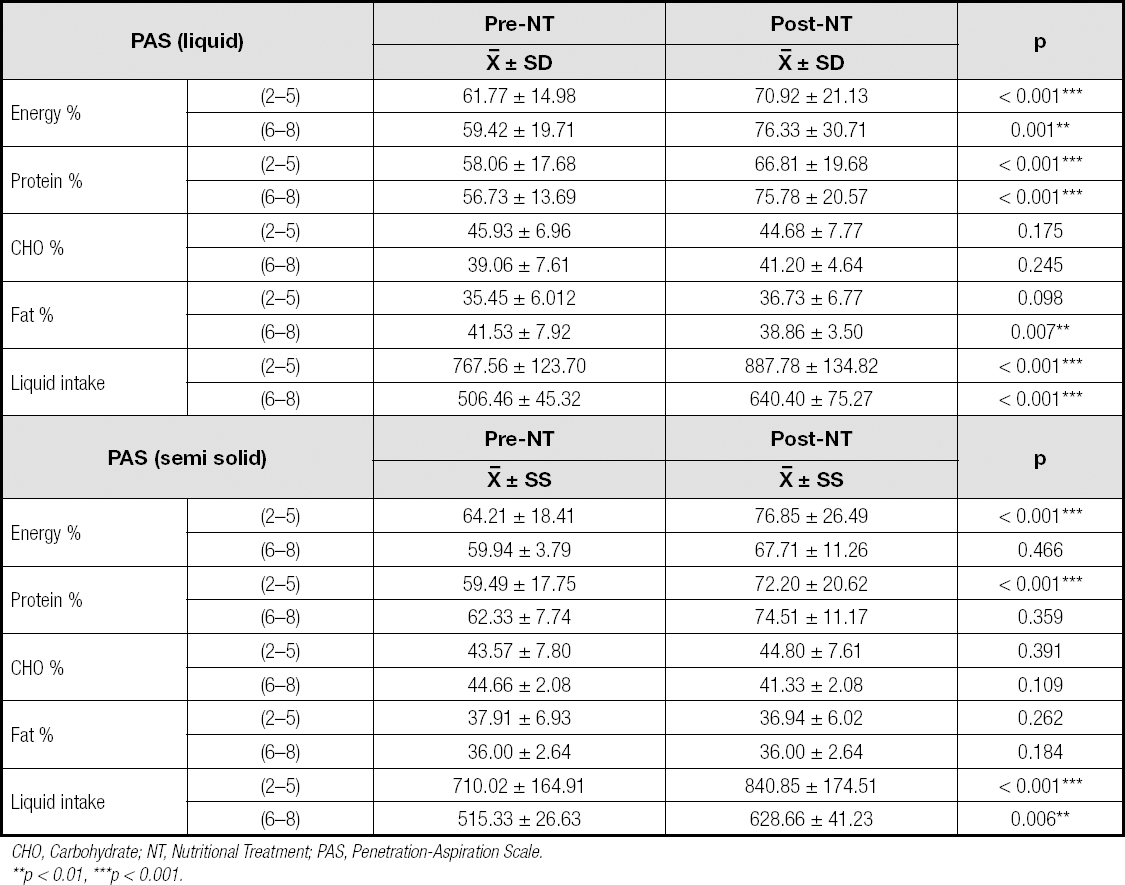
CHO, Carbohydrate; NT, Nutritional Treatment; PAS, Penetration-Aspiration Scale.**p < 0.01, ***p < 0.001.
The comparison of results in terms of NRS-2002 and BMI scores pre- and post-NT are given in table III. According to the results, there is a statistically significant difference between BMI and NRS 2002 scores pre- and post-NT (p < 0.05). In addition, there was no significant relationship between NRS 2002 score groups before and after nutritional treatment (p > 0.05).
Table III. Evaluation of NRS 2002 and BMI values of patients with dysphagia before and after nutrition treatment
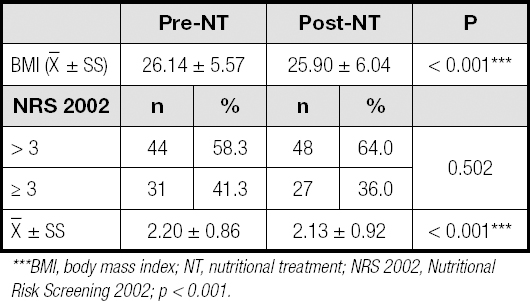
***BMI, body mass index; NT, nutritional treatment; NRS 2002, Nutritional Risk Screening 2002; p < 0.001.
Cronbach's alpha values for the scales, according to the reliability analysis results applied to the SAI and TAI, were found to be 0.845 and 0.903 pre-NT, respectively, and 0.902 and 0.888 post-NT, respectively. The reliability coefficients of the scales were determined. In this study, while the SAI scores of patients with dysphagia were determined before and after nutritional treatment (51.33 ± 6.88; 48.46 ± 7.39, respectively), the TAI scores were determined as 51.42 ± 7.12 and 51.42 ± 4.79, respectively; this appears to be higher than the generally accepted cutoff point. Mean post-NT SAI scores were significantly lower (p < 0.05) than pre-NT values, but there was no significant difference between mean TAI scores (p > 0.05).
Correlations regarding the meeting of daily energy, protein, carbohydrate (CHO), fat, and fluid intake needs, and pre-and post-NT SAI and TAI scores are given in table IV. There is a negative moderate relationship between pre- and post-NT SAI scores and the rate of meeting daily energy and fluid needs, and there is a weak negative relationship between SAI and the rate of meeting daily protein, CHO, and fat needs. There was a negative moderate relationship between TAI scores and the meeting of daily energy, fat, and fluid needs, and a negative poor relationship between TAI scores and the rate of meeting daily protein and CHO needs (p < 0.05). In addition, according to the significance of the differences between pre- and post-NT SAI and TAI scores and nutritional parameters, none of the post-NT correlation increases were significant (p > 0.05).
Table IV. The relationship between energy and macronutrients and anxiety scores of patients with dysphagia before and after nutritional treatment
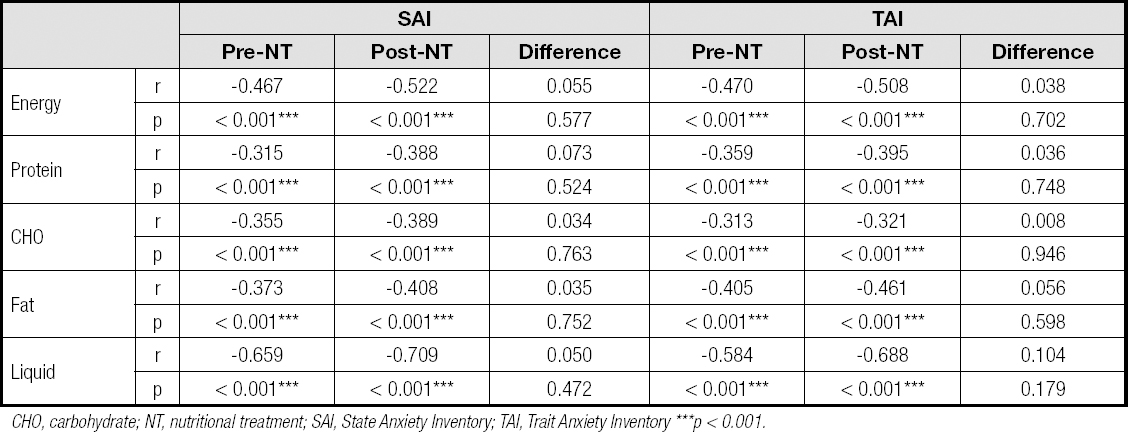
CHO, carbohydrate; NT, nutritional treatment; SAI, State Anxiety Inventory; TAI, Trait Anxiety Inventory ***p < 0.001.
Considering the anxiety scale scores in relation to BMI and NRS 2002 values, it was seen that post-NT SAI scores significantly decreased in terms of NRS 2002 and BMI values (p < 0.05), but there was no significant decrease in TAI scores (Table V).
Table V. Comparison of anxiety scores in relation with NRS 2002 and BMI values before and after nutritional treatment
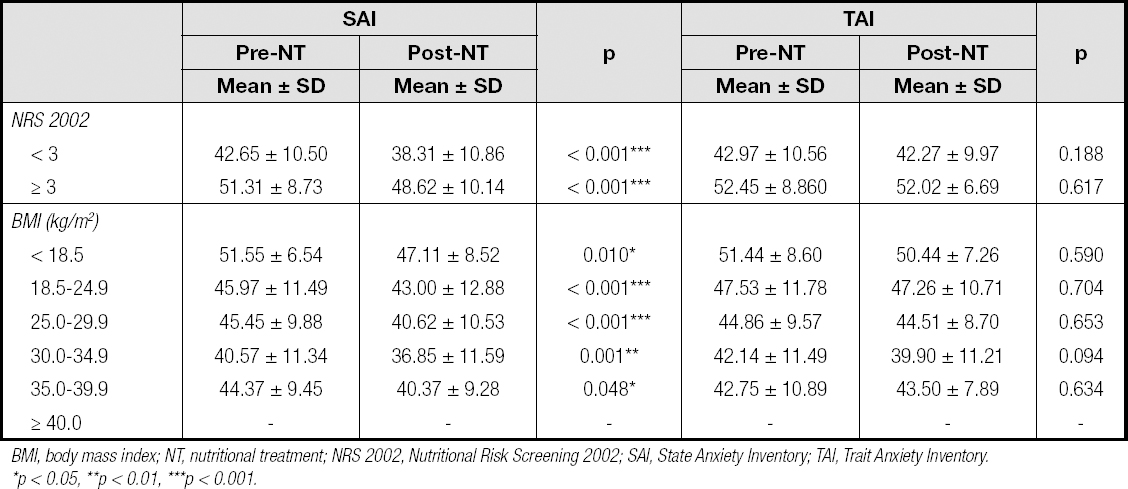
BMI, body mass index; NT, nutritional treatment; NRS 2002, Nutritional Risk Screening 2002; SAI, State Anxiety Inventory; TAI, Trait Anxiety Inventory.*p < 0.05, **p < 0.01, ***p < 0.001.
DISCUSSION
Dysphagia is a disease symptom that requires multidisciplinary treatment, of which a proper dietary intake is an important part. In NT, it is essential to regulate the intake of energy, protein, and fluid in the amount that patients can optimally absorb, and to maintain an optimal consistency to prevent aspiration as well as macro-micronutrient deficiencies (22). In patients with CVD, the frequency of dysphagia increases, and nutritional deficiencies are common (23). The use of oral nutritional supplements to correct nutritional deficiencies in patients with dysphagia, and the use of thickened enteral products to facilitate swallowing are the most effective ways to prevent nutritional deficiency and dehydration in these patients (11). In this study we observed that inadequate pre-NT energy, macronutrient, and fluid intake increased with NT. It may be seen that the increase in the rate of meeting energy and protein fluid intake needs by patients with a PAS score of 2-5 and 6-8 for both liquid and semisolid foods was significant (Table II). In an adequate and balanced diet, in addition to total energy and protein intake, the patterns of other macronutrients such as fat and CHOs in the diet should be taken into consideration. The amount of fat in the diet can increase the severity of dysphagia by changing serum cholesterol, triglyceride, and lipoprotein levels, and by setting the ground for chronic degenerative diseases with increasing age (24). In this study a significant increase was observed in the rate of meeting dietary fat needs in patients with dysphagia (Table II). Increases in energy and nutrient intake are thought to be due to an increase in the consumption of those foods that can be swallowed by patients, awareness of energy-nutrients, and an increase in the consumption of the oral nutritional supports that are recommended to correct the energy and nutrient deficiencies that nutrition cannot amend.
There is a strong link between dysphagia and malnutrition (25). In the available studies the prevalence of malnutrition following CVD was found to be 8 % to 49 % (25,26). In another study involving patients with dysphagia, it was reported that the rate of malnutrition, which was approximately 50 % at 2 weeks after a stroke, decreased to 19 % in the following 4 months (8). NT has a positive effect on weight gain and malnutrition in patients with dysphagia (27). The current NRS 2002 results that changed post-NT also support this outcome (Table III). The decrease in NRS 2002 scores is due to an increase in food intake as a result of the nutritional treatment that patients with dysphagia received at a consistency suitable for their swallowing function status. We think that the decrease in BMI of patients with dysphagia is due to the fact that these patients have different periods of cerebrovascular disease (number of weeks) - rehabilitation at different stages, different course or severity of disease in this period, and presence of an additional chronic disease (DM, etc.). If the nutritional treatment applied to these patients had continued, we think that nutritional treatment would also have had a positive effect on weight gain.
The complications that may occur in patients with CVD also increase the anxiety levels of patients with dysphagia (28). Studies have shown that patients with CVD have higher levels of both state and trait anxiety (29,30). This outcome can be explained by various possible reasons. First, neurological disorders cause physical, physiological, and psychological problems, causing changes in the daily lifestyle of patients. Difficulty in chewing and swallowing may cause additional anxiety due to malnutrition, pneumonia, and fear of death (31). Another possible reason for increased anxiety may be the increased time spent eating due to difficulty in swallowing, which may deteriorate the relationship between patient and caregiver (32). The last possible reason is that patients with dysphagia are embarrassed during eating, so they avoid eating with others (33). It is important to determine the anxiety levels of patients, which also play a vital role in the management of dysphagia. It was reported that 37 % of patients with dysphagia were found to have high anxiety levels (34). NT increases the level of knowledge about safe food intake in both patients and caregivers and thus reduces anxiety levels (35). In this study, a significant decrease was found in post-NT SAI scores. We can attribute this decrease in the scores that reflect immediate anxiety states to the fact that nutritional treatment, which is modified to facilitate chewing and swallowing, both reduces the time spent by the patient with food, and makes the patient feel more secure during this period.
As a result of postural disturbances, visual-perceptual disorders, decreased mobilization, and communication problems in patients with dysphagia and cerebrovascular disease, food consumption begins to decrease, and this situation causes weight loss and malnutrition (25-27), which may be associated with depression and increased anxiety levels (36). In a study examining this relationship, it was found that malnutrition caused increased complications, length of hospital stay/rehabilitation period, and anxiety levels (37). In the present study there was a significassnt relationship between pre- and post-NT SAI/TAI scores and energy and nutrient parameters (p < 0.05) (Table IV). However, according to the significance tests performed on the differences between SAI/TAI scores and nutritional parameters, none of the post-NT correlational increases were statistically significant (p > 0.05). Even if the differences between correlations were not significant, it was seen that NT improved anxiety levels (Table IV). We think that this positive effect on the anxiety levels of patients with dysphagia is due to an increase in the food consumed by the patients, a decrease in risk of complications due to malnutrition, and a decrease in the length of the hospital stay-rehabilitation period, thanks to the consistency changes made to ensure that food intake is safe for each specific patient.
Nutritional status, anxiety level, and quality of life affect each other in neurological patients (38). Nishioka et al. (39) reported that maintaining body weight by improving nutritional status increased quality of life. Serious weight loss or decrease in BMI was associated with anxiety levels (40). In the present study SAI scores decreased post-NT significantly for both NRS 2002 and BMI values (p < 0.05), but no significant decrease was observed in TAI scores (Table V). We think that nutritional treatment, which is given in a consistency that the patient is able to ingest, especially affects the state of anxiety, and that a decrease in the state of continuous anxiety may occur in the future by continuing the same nutritional treatment.
This is an exemplary study showing the effects of nutritional therapy as based on safe food intake on both nutritional status and anxiety levels in patients with dysphagia; however, it has also some limitations. First, no swallowing therapist/physiotherapist experienced in the treatment of dysphagia was included in the study. Second, the patients were at different rehabilitation stages. Another limitation is that the blood parameters that reflect the nutritional status of patients were not examined. Finally, some patients could not be included in the study because they could not be reached. The data of the patients not included in the study could have led to different results, and more patients would have increased the reliability of the results.
Consequently, in this study NT, as based on safe food intake, led to an increase in the meeting of energy and protein requirements, as well as in fluid intake, in patients with dysphagia, which resulted in improvements in patient nutritional status, and a decrease in the risk of malnutrition by causing a decrease in NRS 2002 scores. In addition to the nutritional results, it also showed a positive secondary effect on the state anxiety levels of patients. While these results support the hypotheses of the study, they also emphasize the importance of NT in improving rehabilitation outcomes for patients with dysphagia. Since appropriate posture movements during swallowing, and exercises to reduce swallowing difficulties are important parts of NT for dysphagia, a multidisciplinary approach is required for the management of dysphagia, and more studies are needed on this subject.














