INTRODUCTION
Infantile colic is a behavioral syndrome that manifests as irritable or crying behaviors that are difficult to soothe in healthy babies. It appears for more than three hours a day, lasts for more than three days per week, and lasts for more than three weeks (1). It usually occurs within three months of birth, but approximately 10 % of cases occur after 4-5 months. However, as neurophysiological development occurs, the symptoms of infantile colic will gradually improve, and the symptoms among infants aged three to four months will disappear on their own. In addition, infantile colic can increase the occurrence of psychological distress and depression in caregivers, hinder the development of heathy mother-to-child relationships, and cause infants to suffer accidental injuries and impaired family function (2).
The pathogenesis of infantile colic is unclear. Gastrointestinal motility, lactose intolerance, and psychosocial factors may be involved in the occurrence of infantile colic, but there is no firm evidence (3). Current treatments for infantile colic include dietary adjustments, pharmacological and behavioral interventions, and complementary and alternative therapies, but none of these treatments are effective (4). However, probiotics are viable, nonpathogenic microorganisms that can potentially positively affect a child's body by balancing the intestinal flora. Several beneficial effects of probiotics on the host intestinal mucosal defense system have been identified. These include blocking pathogenic bacterial effects by producing bactericidal substances and competing with pathogens and toxins for adherence to the intestinal epithelium (5-7). The results of research on the treatment and prevention of colic in infants remain controversial. Therefore, this meta-analysis aimed to systematically evaluate the effectiveness of probiotics in preventing and treating infantile colic, to provide evidence-based medical support for clinical practice.
METHODS
DATA SOURCES AND LITERATURE SEARCH
We followed the guidelines of the meta-analysis of observation studies in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). A comprehensive computer search of PubMed, Web of Science, The Cochrane Library, Medline, and Google Scholar databases, collection of published studies on the prevention and treatment of infantile colic as of 2021-11, was performed. Search terms included (probiotic or probiotics or probiotic bacteria) AND (colic or infantile colic or intestinal colic) AND (infant or kid or child and pedia) AND (prevention or treatment or excessive crying or duration of crying or crying time or maternal mental health). The literature was retrieved using the reference backtracking method to avoid missing relevant research as much as possible.
STUDY SELECTION
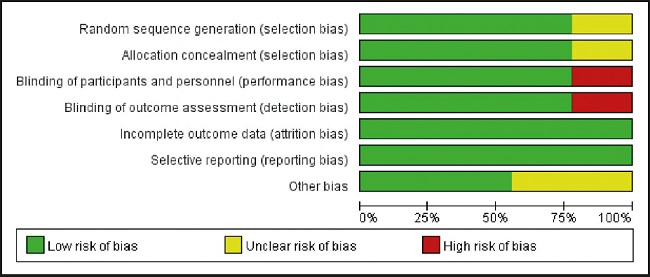
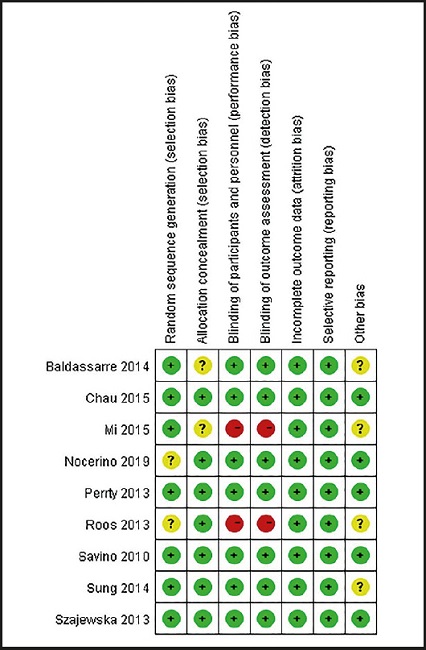
Inclusion criteria were: a) published randomized controlled study (randomized controlled trials [RCTs]); b) assessed association between probiotics and colic in infants; and c) the experimental group was treated with probiotics, and the control group was treated with placebo. In the data, the titles and abstracts of the searched papers were independently screened by two reviewers, and articles that did not meet the above inclusion criteria were excluded. The third person resolved the differences and contradictions between them. The main data extracted include the first author's last name, year of publication, country of study, indication, sample size, interventions, treatment strategy, duration, and outcomes. The overall details of risk of bias were shown (Figs. 1 and 2). Papers selected for retrieval were assessed by two independent reviewers for methodological validity prior to inclusion in the review using standardized critical appraisal instruments for RCTs available through The Cochrane Collaboration. Five trials were categorized as being at low risk of bias, three as being at unclear risk of bias and two as being at high risk of bias. All quality measures recorded, and data extracted for meta-analysis, occurred within Review Manager 5.3.
STATISTICAL ANALYSES
Meta-analysis was performed using Review Manager 5.3. The effect of counting data was RR value and 95 % confidence interval (CI). It was estimated by the Cochran Q test and I2 statistic. Q statistic was considered as significant when the p value was less than 0.10, and the I2 index was used to quantify the extent of statistical heterogeneity. If I2 < 50 %, p > 0.05, it is considered that there is no heterogeneity, and a fixed effect model is used; if I2 > 50 %, p ≤ 0.05, it is considered that there is heterogeneity, and a random effect model is used for analysis. However, there is heterogeneity between the results of each study, I2 > 50 %, p ≤ 0.05; the source of heterogeneity needs to be explored, and sensitivity analysis is necessary if necessary. The publication bias was tested using the Begg method, with a test level of p < 0.05.
RESULTS
STUDY CHARACTERISTICS
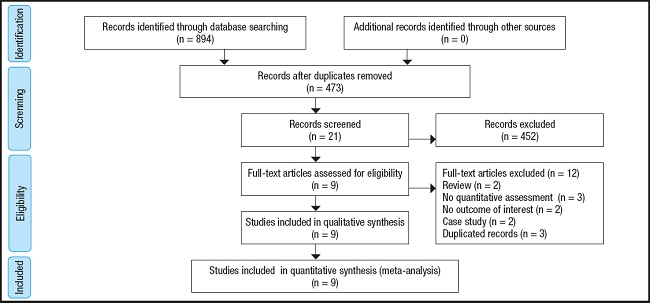
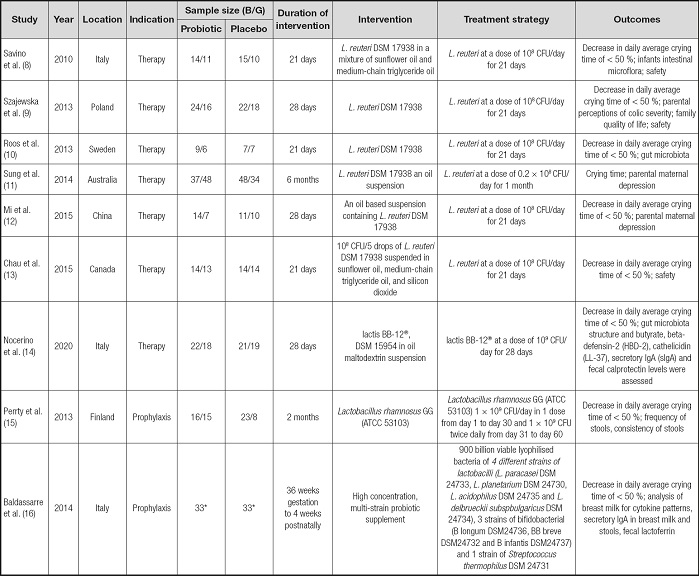
As shown in figure 3, by searching the database, 894 related studies were screened. After reading the title and abstract, 873 studies were excluded. Of the remaining 21 studies, three studies are no quantitative assessment, two studies are no outcome of interest, two studies are review, two studies are case study, and three studies are duplicated records, therefore excluded. Finally, the meta-analysis includes nine RCTs between 2010 and 2020 (8-16), and a total of 587 infant patients. Table I summarizes the characteristics of the studies included. Three studies were conducted in Italy (8,14,16) and one in Poland (9), Sweden (10), Australia (11), China (12), Canada (13) and Finland (15), respectively. All included studies provided probiotic species and application metrics, and most provided number of responders.
PRIMARY END POINT
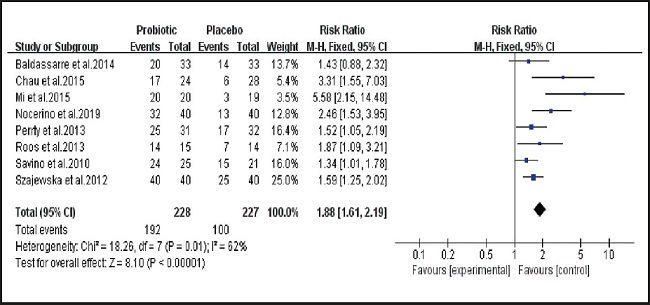
Associations between whole infant colic and the probiotic treatment and prevention
As shown in figure 4, of the nine studies included, eight (8-10,12-16) examined the effectiveness of placebo and probiotics in the treatment and prevention of infantile colic. There was statistical heterogeneity between studies (I2 = 62 %, p = 0.01), and the analysis was performed using a random effects model. The combined effect size (relative risk [RR] = 1.88, 95 % CI: 1.61 to 2.19, p < 0.00001). The results of the analysis suggest that probiotics are generally beneficial for the treatment and prevention of intestinal colic in infants.
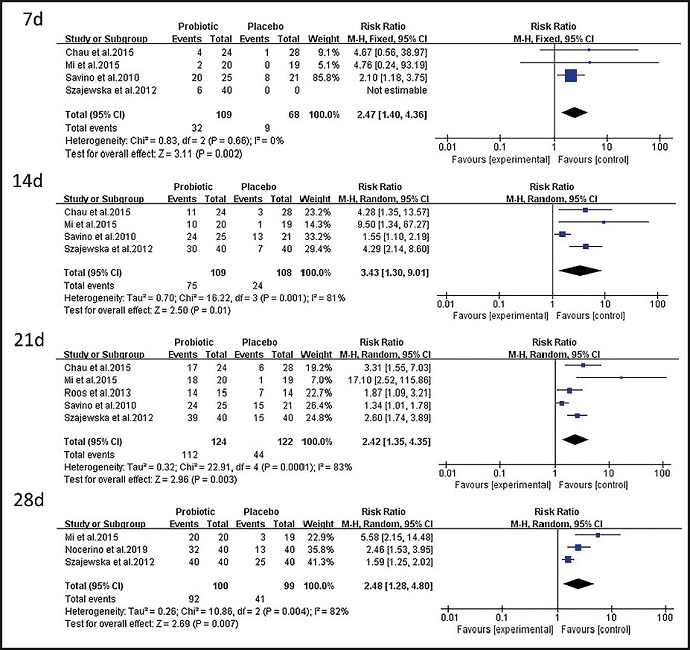
Treatment of infantile colic with probiotics in one month
As shown in figure 5, four of the nine studies included (8,9,12,13) examined the effects of probiotics on infant colic at seven days (RR = 2.47, 95 % CI: 1.40 to 4.36 , p = 0.002); four studies (8,9,12,13) examined the effects of probiotics on infant colic at 14 days (RR = 3.43, 95 % CI: 1.30 to 9.01, p = 0.01); five studies (8-10,12,13) examined the effects of probiotics on infant colic at 21 days (RR = 2.42, 95 % CI: 1.35 to 4.35, p = 0.003); and three studies (9,12,14) examined the effect of probiotics on infant colic at 28 days (RR = 2.48, 95 % CI: 1.28 to 4.80, p = 0.007). The results of the comprehensive analysis suggest that probiotics are more effective than a placebo in treating intestinal colic in infants within seven, 14, 21, and 28 days.
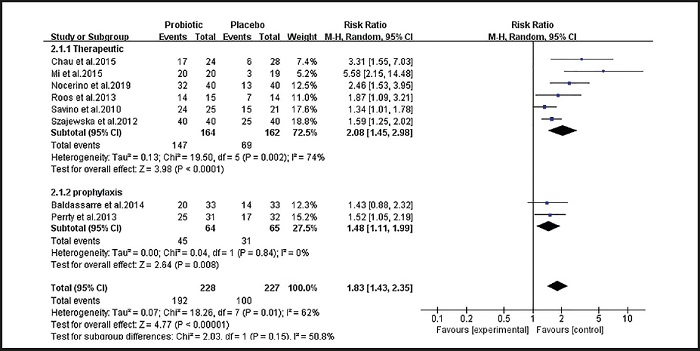
SUBGROUP ANALYSES AND SENSITIVITY ANALYSES
Figure 6 shows the results of a subgroup analysis of the effectiveness of probiotics for treating and preventing intestinal colic in infants. The subgroup analysis examined groups by treatment method. Six studies (8-10,12-14) examined the effects of probiotics on infant colic (RR = 2.08, 95 % CI: 1.45 to 2.98, p < 0.001). There was statistical heterogeneity (I2 = 74 %, p = 0.002). Two studies (15,16) examined the effect of probiotics on the prevention of intestinal colic in infants (RR = 1.48, 95 % CI: 1.11 to 1.99, p = 0.008), and there was no statistical heterogeneity between studies (I2 = 0 %, p = 0.84). The results of the subgroup analysis show that probiotics are effective not only in treating infantile colic, but also in preventing infantile colic. Because there was substantial heterogeneity among the studies that examined treatment, a sensitivity analysis was performed on the treatment group. As shown in figure 7, the overall sensitivity analysis results are stable, and the main sources of heterogeneity are the studies by Mi et al. (12) and Chau et al. (13). After excluding the two studies, the combined effect size reduced the heterogeneity (I2 = 24 %, p = 0.26). However, after excluding any other literature, the heterogeneity did not change significantly.
SECONDARY END POINTS
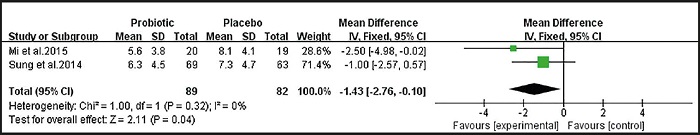
Impact on parent mental health
Figure 8 shows that two studies (11,12) examined the effects of probiotics on the mental health of pregnant women after treatment and prevention of infant colic (WMD = -1.43, 95 % CI: -2.76 to -0.10, p = 0.04). There was no statistical heterogeneity between the studies (I2 = 0 %, p = 0.32). The analysis shows that probiotics can make parents feel happy by affecting the baby's intestinal colic.
PUBLICATION BIAS AND SENSITIVITY ANALYSIS
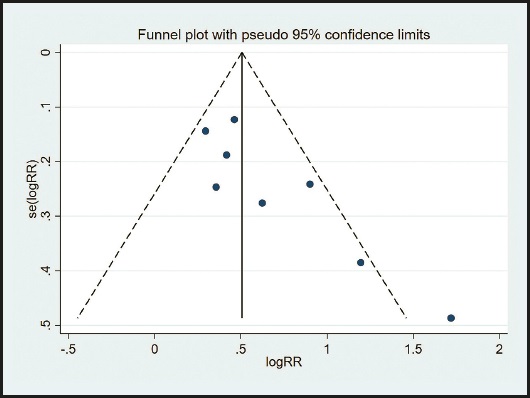
Although the scatter of the funnel plot is slightly asymmetric (Fig. 9), the publication bias was detected by the Begg method. The results showed that the Begg method of the included study was p = 0.063, and there was no evidence of publication bias in the included study.
DISCUSSION
To the best of our knowledge, this is the first meta-analysis examining the effectiveness of probiotics in the treatment and prevention of infantile colic. The results of the meta-analysis show that probiotics are significantly more effective in treating intestinal colic in infants than placebo. Subgroup analysis revealed that probiotics were superior to placebo not only in the treatment of infant colic, but also in prevention. In addition, the use of probiotics to relieve intestinal colic in infants can lead to reduced psychological stress among parents; the results of this study were not found in similar studies.
Infantile colic affects a large proportion of infants. Infants may exhibit symptoms such as uncomfortable crying, painful expressions, high-pitched crying, and curled legs (17). These symptoms are enough to make researchers realize that these infants are in pain. However, in more than 90 % of cases of intestinal colic in infants, the intestinal colic does not need to be treated, but rather, caregivers need to be helped through the challenging period of child growth and development (18). In general, if the symptoms of infantile colic can be relieved and the attention of the caregiver can be appropriately shifted, then infantile colic is not a threat to the baby's body (19). Conversely, an incorrect diagnosis and inappropriate treatment can physically and emotionally harm babies and caregivers unnecessarily (20). Clinicians need to assess caregivers' vulnerabilities, such as depression and lack of social support, and provide sustainable help to the family (21). If attempts to intervene in the baby's intestinal colic are unsuccessful, then it is likely that the caregiver's anxiety and frustration will be increased, eventually impairing the caregiver's ability to comfort the baby and making him/her doubt his/her ability as a caregiver (22).
In our meta-analysis, eight RCTs produced relatively stable results: probiotics can be used to treat and prevent infantile colic, even at seven, 14, 21, and 28 days. A sensitivity analysis revealed that the studies by Mi et al. (12) and Chau et al. (13) affected the stability of the results. Based on the above analysis, we reached a comprehensive conclusion that probiotics can effectively treat and prevent infantile colic, suggesting that probiotics can play an active role in the treatment and prevention of infantile colic. Gerasimov et al. (23) studied the auxiliary application of Lacticaseibacillus rhamnosus (L. rhamnosus) 19070-2 and Lactobacillus reuteri (L. reuteri) 12246 in 84 infants with colic. The mean change in cry and fuss time from day 0 to day 28 was 163 ± 99 minutes in the probiotic group and 116 ± 94 minutes in the control group (p = 0.019). The findings confirm that Lactobacilli can be used to decrease cry and fuss time and to provide dietary support in exclusively breastfed infants with colic. Indrio et al. (24) studied 238 infants who received L. reuteri DSM 17938 probiotics for three months. At three months of age, infants in the probiotic group showed a lower mean duration of crying time (38 vs 71 minutes; p < 0.01), confirming that the use of this probiotic can prevent the incidence of gastrointestinal disorders in infants. In addition, the probiotic strains studied in this paper mainly include Lactobacillus (L. reuteri DSM17938) and Bifidobacterium (B. lactis Bb-12), which are currently the best studied probiotics. Some lactobacilli and Bifidobacterium strains have proven to be most effective if treatment is introduced early (25). In a study by Chau et al. (13), infants took a daily dose of L. reuteri (1 × 108 colony forming units). By 21 days, total average crying and fussing times throughout the study were significantly shorter among infants with colic in the probiotic group compared with infants in the placebo group (29 ± 13 hours vs 37 ± 13 hours, p = 0.028). Infants given L. reuteri DSM 17938 showed a significant reduction in daily crying and fussing times at the end of treatment period compared with those receiving placebo (64 minutes/day vs 87 minutes/day, p = 0.045). On day 21, a significantly higher proportion of infants in the L. reuteri DSM 17938 group responded to treatment with a ≥ 50 % crying time reduction compared with infants given placebo (17 vs 6, p = 0.035). The results of the study by Nocerino et al. (14) showed that infants treated with lactis BB-12 at a dose of 109 CFU/day for 28 days from week 2 had a higher rate of ≥ 50 % reduction in mean daily crying time. After treatment was stopped, no infants relapsed. Mean crying times were reduced in both groups, but the effect was higher in the BB-12 group (-4.7 ± 3.4 vs -2.3 ± 2.2, p < 0.05). Average daily stool frequency was reduced in both groups, but the effect was significantly higher in the BB-12 group; stool consistency was similar in both groups. Bifidobacterium abundance (significantly associated with reduced crying time), butyrate and increased levels of HBD-2, LL-37, sIgA in the BB-12 group were associated with decreased fecal calcin levels.
Although this study has formulated strict inclusion and exclusion criteria, it still has the following limitations: a) statistical heterogeneity has been detected in the current study (heterogeneity may be due to different probiotic types and different sample sizes); b) some studies did not explain randomization methods, distribution methods, and statistical analysis methods; c) due to language restrictions, only English literature was included, and literature in other languages was excluded; d) the quality of different studies varies, which may lead to bias; and e) different research treatments are different.
The differences in treatments may directly lead to the degree of colic in infants and affect the prognosis. Nowadays, the international community has been working to find a specific probiotic strain with good effect and good safety to better treat infant patients, but it seems to be cautious about probiotics treatment and prevention of infant colic. Therefore, in the future, more rigorous multi-center randomized double-blind controlled trials will further clarify the significance of probiotics in preventing and treating colic in infants.
CONCLUSION
In summary, the meta-analysis has extensively evaluated the existing data, and the results show that probiotics have a certain positive effect on infant colic. Probiotics may improve therapeutic and preventive effects, especially within four weeks of probiotic treatment. However, the conclusions of this study are limited by the heterogeneity of the included randomized controlled trials and require careful consideration. Therefore, we must comprehensively consider the situation of the baby and provide the most appropriate treatment plan under the premise of respecting the wishes of the guardian, improving the treatment effects for the baby, and improving the quality of family life.