Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.29 no.4 Madrid Jul./Ago. 2007
ARTÍCULO CLÍNICO
The use of lyophilized bovine collagen (Colloss®) for treating mandibular cysts. Description of a clinical series
Utilización de Colloss® para el tratamiento de quistes mandibulares. Descripción de una serie clínica
J. Arias Gallo1, J.M. López-Arcas Calleja2, T. González Otero1, E. Gómez García1, M.J. Morán Soto1
1 Médico Adjunto.
2 Médico Residente.
Servicio de Cirugía Oral y Maxilofacial. Hospital Universitario La Paz, Madrid,
España
ABSTRACT
The
treatment of mandible bone cysts commonly leads to the development of bone
defects. When the defects are less than 3 cm and located away from the alveolar
ridge, they usually heal spontaneously within a 6 to 12 month period. However,
if the defect is larger, the regenerative ability of the body is overcome.
Colloss® appears to be an interesting osteoinductive biomaterial. It
is a lyophilized complex from extracellular matrix proteins of bovine bone. It
is composed primarily of type I collagen and variable amounts of BMPs.
Between February 2002 and January 2004, 7
patients with mandible cysts were treated with lyophilized collagen to enhance
bone regeneration. In some of the cases this was combined with autologous bone
or a titanium mesh. We observed incompatibility with autologous bone and a
slight tendency for intraoral exposure of the titanium mesh. Apart from this, we
noted adequate bone healing and regeneration in all the cases. For the authors
of this paper, the advantages of lyophilized collagen are the following:
osteoinductive capacity, absence of any major adverse effects and the role
played in the early detection of recurrence. Its possible disadvantages are its
difficult handling and the inherent complications related to bovine xenografts.
Key words: Colloss®; Mandible bone cyst; Lyophilized collagen; bone regeneration.
RESUMEN
La enucleación de quistes óseos conlleva la aparición de defectos óseos. Se acepta que los cuando son menores de 3 cm. de diámetro y están alejados del reborde alveolar se rellenan de hueso neoformado en unos meses. Por el contrario, defectos óseos mayores no regeneran completamente. "Colloss®" parece ser un interesante material osteoinductivo. Se trata de un complejo liofilizado de las proteínas extracelulares extraídas del hueso bovino diafisario. Contiene fundamentalmente colágeno tipo I y cantidades variables de BMPs. En el período comprendido entre Febrero de 2002 y Enero de 2004 se utilizó colágeno liofilizado bovino para la reconstrucción ósea de 7 pacientes con quistes mandibulares tratados en el Hospital Universitario La Paz (Madrid). Este material se combinó con injertos óseos autólogos o con mallas de titanio en varios de los casos. Se observó en la totalidad de los casos una adecuada regeneración ósea. En dos de los casos, en los que se mezcló Colloss® con hueso autólogo se produjo el rechazo de este último. Tras sus retirada el proceso curativo discurrió sin incidencias. También se constató una tendencia a la exposición intraoral de las mallas de titanio sin que ello se viese reflejado en el proceso de curación. Podemos señalar como ventajas de la utilización del colágeno liofilizado bovino (Colloss®) para el tratamiento de quistes odontogénicos: su capacidad osteoinductiva demostrada; la ausencia de efectos adversos de importancia y su utilidad en la determinación precoz de recidivas. Como posibles desventajas destacaríamos: su difícil manejo; la conveniencia de encontrar un carrier adecuado que permitiese una manipulación más sencilla, la necesidad de ajustar la dosis necesaria de forma precisa y, por último, las complicaciones potenciales relacionadas con cualquier tipo de xenoinjerto de origen bovino.
Palabras clave: Colloss®; Colágeno liofilizado; Quiste mandibular; Regeneración ósea.
Introduction
Bone defects are the result of treatment for certain diseases in the maxillofacial area. Although bone tissue has the capacity to regenerate completely after an aggression, this ability may be insufficient when the size of the defect is too large. In these situations the healing process will ultimately lead to a fibrous scar.
The appearance of bone defects is a consequence of the enucleation of bone cysts. It is accepted that bone defects measuring less than 3 cm in diameter, and which are away from the alveolar ridge, will be filled with newly formed bone in a few months. Larger bone defects however, do not regenerate completely because the regenerative capacity of the organism is surpassed.1 In addition, the frequency of postsurgical infections is higher in large cavities. Many surgeons agree, that for treating these bone defects, there should be some type of graft material.
Autologous bone is essential for the grafts in the maxillofacial area. Unfortunately, compared with empty cavities, the infection of cavities filled with autologous bone is common, especially when used in blocks. In addition, morbidity in the donor area, the unpredictable resorption of grafts, together with the difficulties for contouring and maintaining the position of the grafts, are substantial reasons for exploring new bone regeneration methods.
"Colloss®" appears to be an interesting osteoinductive material. It is a lyophilized complex of extracellular proteins extracted from bovine diaphyseal bone, essentially of type I collagen.2 Its native collagen structure facilitates the growth of cells and blood vessels within it. In addition, it contains various growth factors such as BMPs, TGF-b1 and EGF,3 which could explain its osteoinductive behavior. This material is currently used in human clinical situations for filling cavities and bone defects, as well as for inducing spinal arthrodesis.4 There is little literature on its potential use in cavity renovation of the jaws. This article gathers together the experience of a tertiary hospital on the use of lyophilized bovine collagen for this therapeutic indication.
Material and method
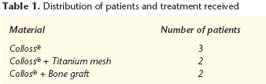
Between February 2002 and January 2004 lyophilized bovine collagen was used for reconstructing bone in 7 patients with mandibular cysts who were treated in the "Hospital Universitario La Paz" (Madrid). This material, in various cases, was combined with autologous bone grafts or with titanium mesh (Table 1).
Patients with large bone defects were included
in the study (the largest diameter had to be over 3 cm). The need for
accelerating bone regeneration in patients at risk of mandibular fractures, or
for reconstructing alveolar ridges for dental implant placement, were additional
indications.
Patients with a history of protein allergy to cows milk or those who rejected being receptors of xenografts, were excluded. The surgical interventions were all carried out under general anesthesia, essentially because of the size of the lesions and the proximity of the lower alveolar neurovascular bundle. Antibiotics were used together with perioperative corticotherapy.
The approach to the cysts was carried out by means of medial incisions into the crest. After the complete enucleation of the cyst, lyophilized collagen with a cotton-like appearance was used to fill the resulting cavity. These particles were introduced into the defects without exerting any pressure in order to avoid compacting them. Given the inherent characteristics of the material with regard to having no compression resistance, in those cases in which the surrounding material was considered excessive, this was secured with a titanium mesh so that the material remained in its original position without compacting.
As can be seen in table 1, lyophilized collagen on its own was used in the defects in five cases. In cases 1 and 2, together with lyophilized collagen, marrow/cortical bone blocks and spongy bone chip were grafted. Infection of the recipient bed occurred in both cases during the immediate postoperative period, together with exposure of the cavity contents and, as a result, prolonged marsupialization of the cystic cavity. Both cases were considered failures due to the absence of any bone regeneration, and they corresponded to the first two patients in the study. As a result it was decided that, from this point on, the lyophilized collagen and autologous bone combination would not be used.
In other two cases titanium mesh was used as a physical barrier. This was to avoid the biomaterial collapsing as a result of the prolapse of the soft tissue in its interior. Mesh exposure occurred in one case after 6 weeks, which required removal under local anesthesia (Fig. 8). Bone regeneration, in any event, evaluated, by means of an orthopantomography, proved satisfactory (Fig. 7).
In the other three cases, the healing process passed without any major incidences, and bone regeneration was considered to be practically complete in the radiographic evaluation.
Three cases that are representative of the three groups appearing in table 1 are discussed:
• Case 1 (Colloss® + autologous bone graft). The patient, 29 years old, attended our department because of an asymptomatic enlargement of the mandibular symphysis. The orthopantomography showed a multilocular cystic cavity (Fig. 1). Under general anesthesia, and through a sulcus incision, the cyst and the teeth involved were extracted. The intraoperative biopsy gave a diagnosis of odontogenic keratocyst. The cavity was treated with Carnoy solution and, after this, exhaustive curettage was carried out of the remaining bony walls. Considerable loss of the vestibular ridge was observed. The bony defect was filled with two spongycortical bone blocks of iliac crest that were fixed with screws to the cavity bed (Fig. 2), and 20 mg of lyophilized collagen was added. Wound dehiscence occurred ten days after the intervention and there was active infection and graft exposure. The patient was reoperated. The grafts were removed and the wound was resutured. Dehiscence occurred once again and closure was achieved by second intention healing over 11 weeks.
• Case 2 (Colloss®). The patient was 81 years old and he was suffering from asymptomatic bulging of the right mandibular angle (Fig. 3). At the consultation he was diagnosed by means of FNA as having a benign cystic lesion. Due to the risk of a pathologic fracture during the postoperative period, it was decided that the cyst should be removed under general anesthesia. After using a vestibular approach and removing the bony roof, an intraoperative biopsy was carried out that gave the result of follicular odontogenic cyst. The enucleation of the cyst was then completed and the cavity was filled with 40 mg of lyophilized collagen (Fig. 4). The postoperative period was incident-free. A soft diet was recommended for eight weeks, at the end of which the patient resumed his normal diet. After 6 months bone regeneration, evaluated by orthopantomography, was practically complete (Fig. 5).
• Case 3 (Colloss® + titanium
mesh). The patient was 40 years old,
with radiolucency in the mandibular body region that corresponded to an
odontogenic keratocyst that had previous been removed (Fig. 6). With the
presumed diagnosis of a recurring keratocyst, a new extraction of the cyst and
teeth involved was carried out. The cavity was treated with Carnoys solution
and aggressive curettage of the cavity was carried out. The defect was filled
with 40 mg of lyophilized collagen. A titanium mesh was placed in order to avoid
soft-tissue interposition in the cavity (Fig. 7). After 6 weeks the mesh became
exposed. The rest of the healing period was incident-free. The follow- up
orthopantomography a year later showed completed bone regeneration with slight
loss of alveolar bone height (Fig. 8). The patient is still awaiting implant-supported
rehabilitation because of financial reasons.
Discussion
The treatment for mandibular cysts is controversial. There is a wide range of possibilities that include: enucleation with exhaustive curettage, treatment with Carnoys solution, marsupialization and decompression.5 In the literature conservative treatment by means of decompression or marsupialization is positively viewed. These treatments clearly require a high degree of cooperation by the patient over extensive time periods that can sometimes be for over 3 years, and which on many occasions have to be complemented with surgical treatment. For these reasons, the treatment of choice is surgical enucleation of the whole cyst followed by pathologic examination. The authors of this article are of the opinion that most surgeons prefer surgical treatment. The use of complementary measures such as treatment with Carnoys solution, aggressive curettage of bony walls, or radical resection, will depend on the degree of aggressiveness of the primary lesion. With odontogenic keratocysts and ameloblastomas, the treatment should be more aggressive than with follicular and periapical cysts. The need for using a surgical procedure for facilitating bone regeneration after cyst removal, is not always obvious. In those cases where the bone defect is located at a sufficient distance from the alveolar ridge of the mandible, the defect can be left to heal spontaneously, providing a sufficient amount of bone remains to prevent the mandible from fracturing.
However, if the remaining bone is thin and with insufficient thickness, the use of procedures that permit the acceleration of bone healing is recommended. Possible complications will in this way be avoided. In addition to those cases in which posterior rehabilitation with implant-supported prostheses is envisaged, attempting to maintain the thickness and height of the alveolar crest is fundamental. In addition, recurrence assessment (such as a new area of osteolysis) by means of radiological tests is made easier if the bone defect has been filled completely with regenerated bone from the beginning.
Autologous bone continues being the first option for filling bone defects. Unfortunately, there are various situations in which autologous bone grafts are not recommended. Being elderly, patient preferences, or possible donor area disturbance, are some of the reasons for the contraindication of these grafts.
In addition to this, as we have verified with two of the patients in our study, the combination of lyophilized collagen and autologous bone produced dehiscence and infection of the surgical wound, and it was for this reason that this system stopped being used. We believe that the infections were produced as a result of poor vascularization of the receptor bed. Also large graft blocks were needed given the considerable size of the defects and, in addition, there was probably oral flora contamination.
In cases in which the bone defect is very large, using a collagen form biomaterial is probably recommended instead of a bone graft. Colloss® absorbs blood and liquid from the surgical bed, which is integrated quickly into the clot in the bed. In this situation we have the impression that the surgical bed has considerable resistance to infection.
Guided bone regeneration techniques tend to be used in small sized defects, as in larger defects, immobilizing membranes and avoiding their collapse is very difficult. Moreover, possible membrane exposure can lead to local infection, which reduces the underlying bone regeneration.
We have used titanium meshes for trying to stabilize the volume of the filling material, as this biomaterial has no mechanical resistance to compression whatsoever. Thus, from this study we can deduce that the presence of periosteum cells in the wound margins does not inhibit lyophilized collagen induced bone regeneration.

Of all the materials available in the market for maximizing bone regeneration, those derived from collagen are the most used. In addition to being useful as hemostatic agents, their composition and physical structure permits growth through them. Unfortunately, the products derived from collagen that are routinely used, are not osteoinductive as their processing entails variable levels of protein denaturation. As a result of this, they are generally used as a vehicle for osteoinductive molecules or as a maintenance system for these molecules.
Colloss® is a lyophilized extract of bovine bone. In this process there is no protein denaturation, and it is presumed that the biological properties of collagen and other bone proteins are kept in tact.4 In standard production of collagen or gelatin processes, protein is denatured and, as a result, its osteoinductive capacity (that depends on non-collagenous proteins) is lost. Probably other native bone proteins and growth factors are maintained in its structure that could help in the reparative process. Although the exact quantity of growth factors present in lyophilized collagen has not been determined,6 it is thought that the material contains significant quantities of BMPs and TGF-b1. These growth factors have been demonstrated to be strong osteoinductive factors in experimental conditions.
The commercial appearance of lyophilized collagen is that of a material with a cotton-like texture that has no resistance whatsoever to pressure. As a result of this, packing the material into the defect is not recommended as the final volume will be very much reduced, and its regenerative capacity will be limited to a more reduced area. Some authors proclaim the advantages of maintaining the porous structure for stimulating its role as a vehicle of different materials.7 Given these reasons, when the biomaterial starts to become compressed because of the shape and borders of the cavity (a situation that arose in two patients), the use of a titanium mesh is recommended in order to halt any collapse. Mesh exposure is a complication that often appears in the literature, and it occurred in our series. In any event, the healing process was not altered by this circumstance in any of our patients. We believe that the fact that mesh exposure occurred some weeks afterwards, allowed the soft tissue to grow under the mesh, and this in turn favored the bone regeneration.
Lyophilized collagen produces an amount of regenerated bone that is comparable to autologous bone in experimental studies in animals with critical bone defects.8 Due to its cotton-like appearance, it is used principally for treating stable bone defects. The presence of acid pH levels in the receptor bed, which is characteristic of infected tissue, inactivates this biomaterial.9
The principal indication of lyophilized collagen is for filling cystic cavities of the jaws, for filling osteotomy gaps, for reconstructing periodontal bone defects and for use as a local graft in the alveolus.
A common complication that has been described is the appearance of significant local edema after insertion.4 On the other hand, other authors do not reflect the specific complications related to this biomaterial.7 In any event, the patients in our series, did not indicate that this occurrence was particularly bothersome given the context of the surgery carried out. Perhaps the use of corticoids in the perioperative period would have reduced the degree of edema. In none of the cases was the mean hospital stay increased. There was, on the contrary, a tendency for this to be shortened. There were no cases of bleeding or delayed infection.
In all cases, bone regeneration evaluated using a series of orthopantomographies in series, was considered sufficient. In two of the cases implant supported rehabilitation has been completed.
There are very few clinical trials in the English literature on the use of Colloss® in the maxillofacial area.
Conclusions
In conclusion, the advantages of using lyophilized bovine collagen (Colloss®) for treating odontogenic cysts are: its demonstrated osteoinductive capacity; the absence of adverse effects of any importance, and its usefulness in the early identification of recurrences.
The possible disadvantages that could be pointed out are: difficult handling; the need for finding a suitable carrier that would permit simpler handling, the need for adjusting the necessary dose in a precise fashion, and lastly, the potential complications related to any type of xenograft with a bovine origin.
![]() Correspondence:
Correspondence:
José María López-Arcas.
Servicio de Cirugía Oral y Maxilofacial.
Hospital Universitario La Paz, Madrid, España
Paseo de la Castellana 261.
28046 Madrid
Email: drlopezarcas@tiscali.es.
Recibido:
17.01.07
Aceptado:
05.06.07
References
1. Schmitz JP. The critical size defect as an experimental model for craniomandibulofacial nonunions. Clin Orthop Relat Res 1986;205: 299-308. [ Links ]
2. Walboomers XF, Jansen JA. Microgrooved subcutaneous implants in the goat. J Biomed Mater Res 1998;42:634-41. [ Links ]
3. Schlegel KA, Wilfang J, Kloss FR. De novo bone formation using bovine collagen and platelet-rich plasma. Biomaterials 2004; 25:5387-93. [ Links ]
4. Li H, Zou X, Woo C, Ding M, Lind M, Bünger C. Experimental anterior lumbar interbody fusion with an osteoinductive bovine bone collagen extract. Spine 2005;30:890-6. [ Links ]
5. Enislidis G, Ewers R, Fock N. Conservative treatment of large cystic lesions of the mandible: a prospective study of the effect of decompression. Br J Oral Maxillofac Surg 2004;42:546-50. [ Links ]
6. Walboomers XF, Jansen JA.Tissue induction, using a COLLOSS-filled titanium fibre mesh-scaffolding material. Biomaterials 2005;26:4779-85. [ Links ]
7. Sader R. Erfolge im Mund- Kiefer- und Gesichtsbereich. En: Horch H, Wilhelm K, Zeilhofer HF, editors. Forschritte in der Beahndlung vone Knochedefekten. Interdisziplinäres Symposium 2001;7:8. [ Links ]
8. Witlfang J, Kloss FR, Schlegel KA.Tierexperimentelle studie zum einsatz von knochenersatzmaterialem und thrombozytenreichem palsma in klinisch relevanten defekten. Dtsch Zahnarztl Z 2005;57:307-11. [ Links ]
9. Strassmair M. Behandlung von Knochendefekten durch Osteoinduktion. Wehrmedizin und Wehrpharmazie 2001;3:59. [ Links ]











 texto em
texto em