Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.31 no.4 Madrid Jul./Ago. 2009
Submental flap to reconstruct oncologic head and neck defects
Colgajo submental para reconstrucción de defectos oncológicos en cabeza y cuello
J. Brunsó Casellas1, J.C. Martín Rodríguez2, L. Barbier Herrero2, E. Ortiz de Zárate Román2, A. Bidaguren Urbieta1, J. Santamaría Zuazua3
1 Médico residente
2 Médico adjunto
3 Jefe de servicio
Servicio de Cirugía Oral y Maxilofacial. Hospital de Cruces. Barakaldo, España
ABSTRACT
The submental flap is an effective option for the reconstruction in the maxillofacial territory. Characterized by its thinness, versatility, excellent colour and texture and minimum morbidity in the donor zone, its use in malignant injuries is controverted by the risk of transferring cervical metastasic disease to the receiving zone.
Material and methods: we present 3 clinical cases in which it has been used in patients affected by an squamous cell carcinoma of head and neck. In addition, the anatomical particularities are described, and a revision of the surgical technique is made.
Results: They were optimal in relation to covering of the defect, aesthetics and function except for a partial necrosis in one of them. In all the cases the morbidity in the donor zone was minimum.
Conclusions: The submental flap is an option to consider in oncologic patients, mainly in those whom by advanced age or by the existence of comorbidity advice against the use of more aggressive procedures.
Key words: Submental flap; Head and neck reconstruction; Oral and maxillofacial defects.
RESUMEN
El colgajo submental es un procedimiento eficaz para la reconstrucción en el territorio maxilofacial. Caracterizado por su delgadez, versatilidad, excelente color y textura y mínima morbilidad en la zona donante, su utilización en lesiones malignas es controvertida, por el riesgo de trasladar enfermedad metastásica cervical a la zona receptora.
Material y métodos: Se presentan 3 casos clínicos en los que se ha aplicado en pacientes afectos de un carcinoma epidermoide de cabeza y cuello. Describimos las particularidades anatómicas, y se realiza una revisión de la técnica quirúrgica.
Resultados: Fueron óptimos en cuanto a cobertura del defecto, estética y función salvo por una necrosis parcial en uno de ellos. En todos los casos la morbilidad en la zona donante fue mínima.
Conclusiones: El colgajo submental es una opción a considerar incluso en pacientes oncológicos sobre todo en los que, por edad avanzada o presentar patología asociada no están indicados procedimientos más agresivos.
Palabras clave: Colgajo Submental; Reconstrucción cabeza y cuello; defectos orales y maxilofaciales.
Introduction
Removing large lesions from the maxillofacial zone involves the need for reconstruction. In serious defects free microvascularized flaps would be the choice. Thin and versatile flaps like the radial fasciocutaneaous and ALT have proven to be more than effective. They offer indubitable advantages, but also inconveniences for example: prolonged surgery time, morbidity in donor zone, aesthetic problems, and a high failure rate. Despite not having absolute contradictions these flaps would not be used on high risk surgery patients, whether it's because of comorbidity or old age. In these cases we opt to use pedicle flaps or alternative treatments like radio or chemo therapy.
The Submental Flap is an axial flap described by Martin et al.1 in 1993 after successfully using it on 8 patients. During that time the indications for medium size lesions in the maxillofacial region had been thoroughly described. They were characterized by their thinness, versatility, mimicry with facial skin and minimal morbidity in the donor zone. Nevertheless, their use in malign lesions is controversial because of the risk of infecting the receiving neck area with cervical metastasic disease.
We present 3 clinical cases in which we used a submental flap on patients affected by squamous cell carcinoma of the maxillofacial region and we also review of anatomy and surgical technique.
Anatomy
The submental artery is a branch of the facial artery. It starts deep in the sub maxilla gland and continues along the inferior border of the mandible body, above the mylohyoid muscle until the symphysis. Its diameter measures 1.0-1.5 mm with a pedicle measuring 8cm. It circulates under the anterior abdomen muscle where the majority of perforating skin are emitted, although it can go over the surface .2,3 The number of perforates varies from 1-4.2,4 It also emits branches for the periosteum of the mandible bone, the mylohyoid latissimus colli muscle, and even with the mandible symphysis, inferior lip branch and the sublingual gland.3,5 Through the sub dermis plexus the submental artery ends up contacting the contra lateral branch allowing its extension as a random flap in the contra lateral neck. This allows the a large angle flap to be raised to the mandible angle. The vein drainage depends on the submental vain that circulates along with the submental artery and then ends up draining into the facial vein (Fig. 1).
Surgical Technique
With the patient in a hyper extended position we draw the superior limit of the flap just below the mandible arch in order to disguise the scar. The length of the cutaneous palette can extend from one mandible angle to the other. The inferior limit is drawn after comparing the direct closing with the small sample. The cutaneous palette is divided by an incision that separates the skin and the subcutaneous tissue until the latissimus coli muscle and starts to subplatismally raise the flap from the distal until the digastric muscle and sub maxilla gland are exposed (Fig. 2) Shortly after the ipsilateral sub maxilla gland is separated from the flap attaching the vessels that come towards it. The next step is to approach the superior polo of the flap dividing the latissimus coli muscle and identifying the marginal branch of the facial nerve and artery. The facial artery is carefully dissected until it is lost under the gland. At this point traction of the gland identifying the submental artery; however, it is not necessary to dissect the submental artery so that the flap reaches the majority of the most habitual receptor layers. Obviously that depends on the quantity of pedicle needed.
Afterwards the contra lateral side is raised from underneath the latissimus coli muscle of lateral to medial maintaining the facial artery and anterior digastric abdominal muscle intact. Even with the mid line, the flap is inserted into the anterior abdomen of the ipsilateral digastric muscle, removing it from the symphysis and dividing it even with the polea. In the opposite case the perforants should be located and dissected. Patel et al.6) describe a variable that consists of incorporating the mylohyoid muscle on the ipsilateral side to the flap as well as the anterior abdomen of the digastric muscle. In this way the pedicle is protected and the procedure is much simpler and faster, although the thickness of the flap is increased.
The facial artery is tortuous and large enough to allow for good arch rotation. If the longitude of the pedicle is sufficient the surgery ends up freeing the whole palette. If it is insufficient, the artery and the facial vein are distally attached to the origin of the submental artery and it is increased by 2 cm. Sterne et al.7 used CS for the first time with an inverse flow design attaching the facial artery close to the origin of the submental artery, achieving considerable increase of the pedicle. Kim et al.4 also successfully used it but with variations. Pistre et al.8 thought the inverse design should only be used when the normal flow is not possible, either because the pedicle is too short or because of an artery injury, since there is a high risk of injuring the facial nerve when distally dissecting the pedicle.
We can also increase the length of the venous pedicle by dissecting a communicative branch between the facial vein and the external jugular. Attaching the facial vein, the Y vascular becomes a V vascular allowing for a 5 cm gain.9
The use of the submental flap does not interfere with a radical cervical dissection. Nevertheless it makes it necessary to modify the incision design that depends on the size of the flap and the pedicle side. It is recommended to start by first raising the flap to protect the pedicle. With large flaps the incision is bigger from lateral extreme of the ellipse until the mastoid region, carrying out a vertical incision of 2 cm behind the mandible angle until the clavicle, all the while avoiding sharp angles (Fig. 3). For the small flaps it is possible to carry out a design with a superior base that ensures better irrigation.6
Finally we comment that the internal facial bone of the mandible symphysis has been described as a free flap and also a compound flap; In which case it should be associated to the portion of the mylohyoid muscle.8,11
Clinical Cases
Case 1: Male 80 years old with indurate T4 lesion, diagnosed as a squamous cell carcinoma of the anterior half of the tongue, the belly of the tongue and the floor of the mouth provokes the displacement of the tongue which makes diction and swallowing difficult. The image tests didn't show evidence of metastasic at the regional level nor at a distance (T4N0M0). The patients are in a generally acceptable state that, even though aggressive intervention is not advised because of his age, the prognostic suggests a more radical option: excision with margins, reconstruction with CS and expectant cervical conduct. A 17 x 8 flap was obtained. Because the cutaneous palette was excessive we depithelize the ipsilateral lateral extreme until we achieved the adequate size at the limits of the defect to be reconstructed (Fig. 4). After this we tunneled the flap between the geniohyoideus muscles dividing the mylohyoid muscle along the mid line. In post op there was vein congestion in the flap that started to relax after 4 days (Fig. 5). A cervical bruise also appeared but reabsorbed spontaneously. The patient showed favorable progress and was discharged after 8 days and did not present signs of illness at that time. Defect of the donor zone was minimal.
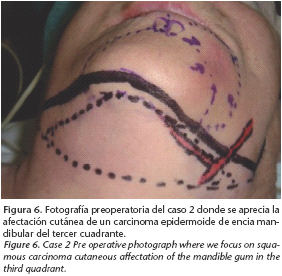
Case 2: Female 81 years old with Squamous Cell Carcinoma of the 3rd quadrant mandible gum with infiltrated inferior labial muscles (Fig. 6). No evidence of metastatic disease at the cervical level during the physical exam and image tests. We decided to excise the lesion of gum and lip with mandibulectomy segmented margins, cervical supraomohyoid ipsilateral dissection and reconstruction of the submental flap of the contra lateral pedicle and ipsilateral buccinators (Fig. 7). In the post op she showed favorable progress. The patient specified a thinning of the buccinator flap and after one year showed no sign of disease. The after effect of the donor zone was minimal.
Case 3: Woman 83 years old with Squamous Cell Carcinoma on the buccal floor 10 months after having excision, mandibulectomy, supraomohyoid cervical dissection and reconstruction of the osteosynthetic plate. The patient did not show signs of cervical metastasic even at a distance in the image tests. We decided to excise the relapse with margins and reconstruct the defect with a submental flap with contra lateral pedicle. The flap was tunnelized via the mylohyoid muscle (Fig 8). In post op the patient showed critical necrosis in a third of the submental flap. Nevertheless this did not need any further reconstruction. At the time the patient showed no signs of remote metastasis.
Discussion
Baudet et al.12 showed in his 2003 work that the majority of reconstructive processes of the head and next were resolved with satisfaction by using conventional surgical procedures. This indicates that free microvascularized flaps for the first ones are not sufficient. The submental flap has shown is versatility in lesions of the inferior half of the case of trauma, tumors, burns,2,7,8,13,14 and noma disease.8,15 In order to improve the facial contour in hemi facial microsomia and facial paralysis (160, hard palate reconstruction and buccal floor lesions,6,10,18,19 Kim et al.4 used a submental flap of inversed flow to reconstruct the nose. Pistre et al.8 used it as a compound flap and incorporated mandible bone. Kitazawa et al.20 used the bipedicle flap to reconstruct a superior labial lesion. Therefore, the submental flap can be a valid alternative to free microvascularized flaps.2,7,13,14,16,18,19 Other regional flaps like the platismal21, supraclavicular22, infrahyoid23, and random type local flaps can have similar characteristics but generally offer less mobility, less reliability, increased consequences in the donor zone and cutaneous palettes smaller in size. After using it on 31 patients, Pistre et al.8 considered the submental flap as the best method to reconstruct facial defects.
In oncology cases, some authors do not recommend its use when there is level I metastatic disease. We think that in cases where there are positive cervical ganglion it would be convenient to evaluate other reconstructive options since, like Shah et al.24 showed in 1990, the incidence of positive ganglions in the first level after elective dissection is 20% compared to 48% after a therapeutic dissection of squamous cell carcinoma of the oral cavity. It would be suggested, therefore, for oncology cases that show no cervical metastatic carcinoma and also for patients that because of their age of serious comorbidity are not candidates for more aggressive procedures. Included in these would be cases of palliative surgery. Nevertheless it is convenient to evaluate each case in particular and the patients that specify cervical lymphadenectomy would definitely need a meticulous surgical technique in order to minimize risks.
The results we obtained coincide with those described in the bibliography. The submental flap satisfactorily covered the defects. None of the cases had a failed flap but some had partial necrosis in the critical third zone upon reconstruction, possibly because of the tunnelization that took place in order to improve the reconstruction zone. The flap also showed a high tolerance to radiation and there were no complications after complimentary radiotherapy treatment. There also were no indicators of having transferred the disease from the cervical receptor zone, maintaining the receptor layer free from disease. Nevertheless, the patient in case 3 showed metastasic 7 months after intervention. In terms of the size of the palette, even though Martin et al.1 recommended a maximum size of 15X7, in our case #1 we had a palette measuring 17x8 cm due to the laxity of the cervical skin of the patient. In all of the cases we chose to incorporate the anterior belly of the digastric muscle to assure perfusion and flap drainage. None of the cases specified techniques to increase the length of the pedicle. In terms of the lesion of the marginal branch of the facial nerve, it only appeared in case 2 after excision because of oncological indication; in general it is low in the majority of cases even though in others the complication occurs in up to 16%7.
The oral cavity managed to notably preserve its oral functions of feeding and expression. The pedicle is long enough so that it reaches the entire oral cavity, allowing the lesions to be reconstructed on the tongue and buccal floor including dental patients. In the case where the submental flap should be tunnelized through the muscular floor of the mouth in the majority of cases, venous congestion appears that usually does not risk the viability of the flap. In our case #1 it was resolved in a few days.
Conclusions
The submental flat is a reconstructive option that should be considered when dealing with head and neck oncology patients that need a decent size flap. This flap is especially useful in elderly patients or patients that have other diseases that require them to have less invasive surgical treatments. This flap is a good alternative to the microvascularized flaps.
![]() Correspondence:
Correspondence:
Joan Brunsó Casellas
C/ Larrinaga, nº1. 2º interior izquierda
48003 Bilbao. Vizcaya, España
Email: jbrunso@gmail.com
Recibido: 01.09.2008
Aceptado: 11.05.2009
References
1. Martin D, Pascal JF, Baudet J, Mondie JM, Farhat JB, Athoum A, et al. The submental island flap: A new donor site. Anatomy and clinical applications as a free or pedicled flap. Plast Reconst Surg 1993;92:867-73. [ Links ]
2. Curran AJ., Neligan P, Gullane PJ. Submental artery island flap. Laringoscope 1997;107:1545-9. [ Links ]
3. Martin D, Baudet J, Mondie J, Peri G. The submental island skin flap: A surgical protocol. Prospects of use. Ann Chir Plast Esthet 1990; 35:480-4. [ Links ]
4. Kim JT, Kim SK, Koshima I, Moriguchi T. An anatomic study and clinical applications of the reversed submental perforator-based island flap. Plast Reconst Surg 2002; 109:2204-10. [ Links ]
5. Whetzel TP, Mathers SJ. Arterial anatomy of the face: An analysis of vascular territories and perforating cutaneous vessels. Plast Reconst Surg 1992;89:591-603. [ Links ]
6. Patel U, Bayles SW, Hayden R. The submental flap: A modified technique for resident training. Laryngoscope 2007; 117:186-9. [ Links ]
7. Sterne GD, Januszkiewicz JS, Hall PN, Bardley AF. The submental island flap. Br J Plast Reconst Surg 1996;49:85-9. [ Links ]
8. Pistre V, Pellissier P, Martin D, Lim A. Baudet J. Ten years of experience with the submental flap. Plast Reconst Surg 2001;108:1576-81. [ Links ]
9. Martin D, Legaillard P, Bakhach J, Hu W, Baudet J. L' allongement pediculaire en YV a flux retrograde: un moyen pour doubler l arc de rotation d'un lambeau sous certaines conditions. Ann Chir Plast Esthet 1994;39:403-14. [ Links ]
10. Pistre D, Pelissier P, Martin D, Baudet J. The submental flap: Its uses as a pedicled or free flap for facial reconstruction. Clin Plast Surg 2001;28:303-9. [ Links ]
11. Yilmaz M, Menderes A, Barutcu A. Submental artery island flap for reconstruction of the lower and mid face. Ann Plast Surg 1997;39:30-5. [ Links ]
12. Baudet J, Casoli V, Pinsolle R, Tessier R, Pelissier P, Martin D. Conventional surgery in head and neck reconstruction. Is it out of date? ANZ J of Surg 2003;73:196. [ Links ]
13. Abouchadi A, Capot-Degardin N, Patenotre P, Martinot-Duquennoy V, Pellerin P. The submental flap in facial reconstruction: Advantatges and limitations. J Oral Maxillofac Surg 2007;65:863-9. [ Links ]
14. Demir Z, Kurtay A, Sahin U, Velidedeoglu H, Celebioglu S. Hair-bearing submental artery island flap for reconstruction of mustache and beard. Plast Reconstr Surg 2003;112:423-429. [ Links ]
15. Barthelemy I, Martin D, Sannajust JP, Marck K, Pistre V, Mondié JM. Prefabricated superficial temporal fascia flap combined with a submental flap in noma surgery. Plast Reconstruct Surg 2002;109:941-2. [ Links ]
16. Tan Onder, Atik Bekir, Parmaksizoglu Duygu. Soft-tissue augmentation of the middle and lower face using the deepithelialized submental flap. Plast Reconstruct Surg 2007;119: 873-9. [ Links ]
17. Genden EM, Buchbinder D, Urken ML. The submental island flap for palatal reconstruction: A novel technique. J Oral Maxillofac Surg 2004; 62:387-90. [ Links ]
18. Chow TL, Chan TT, Chow TK, Fung SC, Lam SH. Reconstruction with submental flap for aggressive orofacial cancer. Plast Reconstruct Surg 2007;120:431-6. [ Links ]
19. Merten SL, Jiang RP, Caminer D. The submental artery island flap for heard and neck Reconstruction. ANZ J of Surg 2002; 72: 121-124. [ Links ]
20. Kitazawa T, Harashina T, Taira H, Takamatsu A. Bipedicled submental island flap for upper lip reconstruction. Ann Plast Surg 1990; 42:83-6. [ Links ]
21. Hurwitz DJ, Rabson JA, Futrell JW. The anatomic basis for the platysma skin flap. Plast Reconst Surg 1983;72:302-14. [ Links ]
22. Hartman EH, Van Damme PA, Sauter H, Suominen SH. The use of the pedicled supraclavicular flap in noma reconstructive surgery. J Plast Reconstr Aesthet Surg 2006;59:337-42. [ Links ]
23. Wang H, Shen JW, Ma DB, Wang JD, Tian AL. The infrahyoid myocutaneous flap for reconstruction after resection of head and neck cancer. Cancer 1983;57:663. [ Links ]
24. Shah JP, Candela FC, Poddar AK. The patterns of cervical lymph node metastases from squamous carcinoma of the oral cavity. Cancer 1990; 66:109-13. [ Links ]











 texto em
texto em