INTRODUCTION
MASC is a low-grade malignant salivary gland cancer, first described by Alena Skálová in 20101, with various similarities to the secretory carcinoma of the breast including histology, immunohistochemistry and a genetic translocation2.
Epidemiologically, it is usually encountered in adults with a mean age of 46 years-old3 and a slight male predominance3,4. There have been 11 cases described in the paediatric population5.
There are three main differential diagnosis: AciCC which is positive for DOG1, does not have the ETV6-NTRK3 fusion gene and has basophilic granularity in the cytoplasm as an hallmark2,3; mucoepidermoid carcinoma which is positive for p63 and is usually negative for S100 and mammaglobin in addition to having, in most cases, a t(11;19) translocation3 and, low-grade cribriform cystadenocarcinoma which has epithelial structures surrounded by an intact layer of p63 positive myoepithelial cells2.
MASC is usually found in the parotid gland3,4 followed by the oral cavity and submandibular gland3. The most common presentation is of a slowly growing painless nodule2. In most cases it has good prognosis and an indolent course4. High grade transformation followed by an accelerated clinical course with poor prognosis has been described3,4.
CLINICAL CASE
Our case is of a 28-year-old women with no relevant past medical history who presented in the ER with a week old, hard, 5x5mm, adherent and tender nodule in the left parotid region. There was no history of trauma or other symptoms.
Pre-operatory work-up included: blood analysis which showed no relevant alteration; ultrasound which showed a 8x5mm, lobulated, hypoechoic nodule with liquid/cystic content; cytology which described a low grade epithelial / myoepithelial tumour and an MRI describing a bilobulated, 8x5mm, nodule with well-defined borders and a thin wall in the left superficial parotid gland with anterior extension to the masseter muscle.
Thus, we performed a superficial left parotidectomy using a retro-tragal mini-lifting approach. There were no complications during surgery and the facial nerve was preserved.
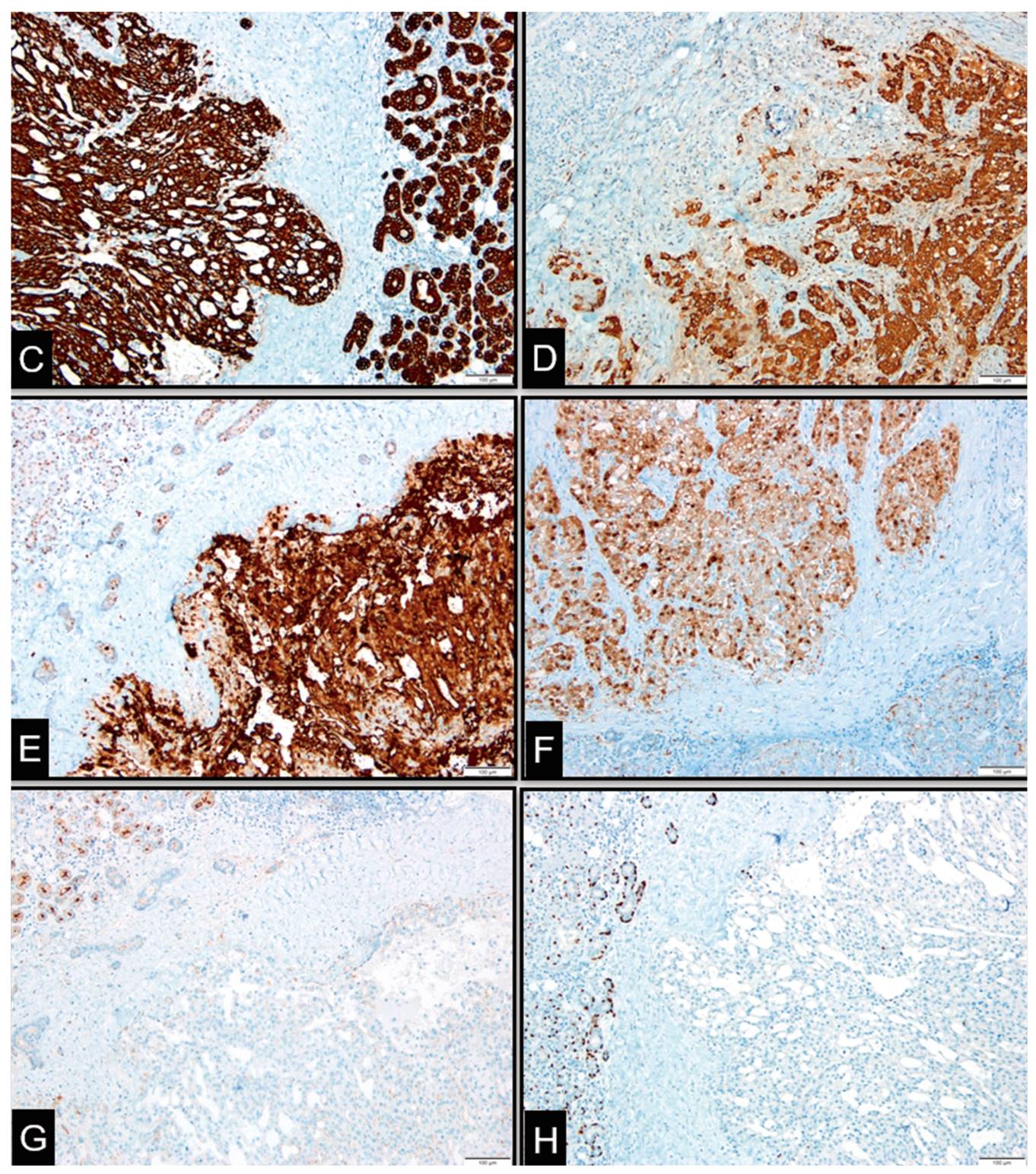
Follow-up included a pathology exam in which the tumour was described as a brownish-yellow well delimitated nodule with a larger diameter of 0.4 cm. Histology (Figure 1) showed an encapsulated neoplasia (A) with a cribriform/microcystic pattern. Neoplastic cells had irregular nuclei, eosinophilic cytoplasm and secretion product in the gland-like spaces (B). Immunohistochemically (Figure 2) the neoplastic cells were positive for CK7 (C), mammaglobin (D), GATA-3 (E) and S100 protein (F) and negative for DOG-1 (G) and P63 (H).
Adjunctive radiotherapy with a total dose of 60Gy was also performed and, to date, the patient remains asymptomatic with no signs of recurrence.
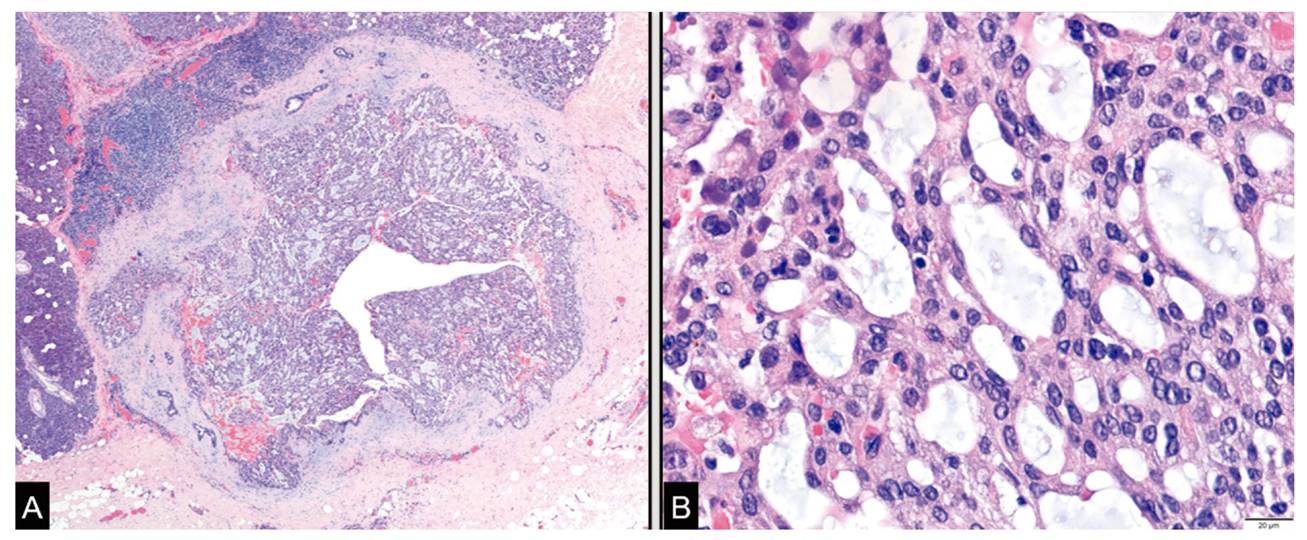
Figure 1. Histology showed an encapsulated neoplasia (A) with a cribriform/microcystic pattern. Neoplastic cells had irregular nuclei, eosinophilic cytoplasm and secretion product in the gland-like spaces (B)
DISCUSSION
MASC is, generally, a solitary2, firm/rubbery mass with a white to grey cut surface3. Fluid-filled cystic spaces may be seen3. Perineural invasion and extension to extra-glandular tissues occurs often but lymphovascular invasion and necrosis are uncommon2,3. Histologically it is a well-defined multilobulated tumor divided into segments by fibrous septa4. Neoplastic cells have uniform and round nuclei3 with centrally located small nucleoli and eosinophilic vacuolated cytoplasm, and can be arranged in microcystic, cribriform, tubular, papillary, follicular or solid nests pattern3,4. Microscopic foci of invasion can be present although atypia is generally mild and mitotic activity is scarse3,4.
Immunohistochemically, it is positive for a wide-spectrum of cytokeratins (AE1-AE3, CAM5.2, CK7, CK8, CK18, CK19), S100 protein, mammaglobin and, in most cases, GCDFP-15, SOX10, GATA-3 and vimentin3,4. Basal cell / myoepithelial markers such as p63, calponin, CK14, SMA, and CK5/6 are virtually always negative. Most cases are negative for DOG-13
Genetically, a t(12;15)(p13;q25) translocation resulting in the ETV6-NTRK3 fusion gene is present4. ETV6 is a transcriptional regulator and NTRK3 is a membrane receptor kinase3. The fusion gene results in a ligand independent activation of the kinase thus promoting cell proliferation and survival2,3. This fusion gene has not been described in other salivary gland tumours3 .
Imagiologic descriptions are lacking in the literature. On MRI the tumour shows hyperintensity relative to muscle in T1 and hypointensity relative to the parotid gland in T22.
The treatment of choice in MASC is complete surgical resection (standard care for low grade salivary carcinomas) 2,3. Locoregional radiation is sometimes considered, mostly in cases with positive margins or perineural invasion3, although the impact on prognosis is not established2. Systemic chemotherapy can be implemented if distant metastases are present3. Response to tyrosine kinase inhibitors has been described in other tumours with the ETV6 translocation but not in MASC3.