INTRODUCTION
Cleft lip palate is most common congenital anomalies in the craniofacial region, with higher prevalence of births than neural tube defects or Down syndrome, according to WHO. Although causal factors are unknown, multifactorial etiology with genetic predisposition and environmental influence is currently accepted1,2. Multidisciplinary management of patients with cleft lip palate is of most importance their future psychosocial development. Inability communicates affects psychological and emotional well-being children and their families3. However, patients with cleft palate present anatomical alterations due to lack of fusion of palatal processes during pregnancy, therefore, there is a risk distortion of resonance and articulation of sounds, interfering speech same4.
Crying of newborns and infants is functional expression of fundamental biological interest, such as hunger, cold, pain, loneliness, and even joy5,6. Characteristics of crying reflect development and possibly integrity of central nervous system, is complex phenomenon that involves the production of sound the vocal cords and occurs fundamentally during expiratory phase of breathing; requires functioning of respiratory, laryngeal and supralaryngeal muscles, therefore, is under control of neurovegetative regulation systems of brain stem, especially vagal complex includes the cranial nerves IX to XII7. Therefore, analysis of infant crying is suitable complementary tools detecting certain pathologies such as neonatal hypoxia8.
Due advancement of technology, software has been created for acoustic analysis of voice and crying, functioning as an objective, non-invasive, quick and simple tool vocal exploration, analyzing acoustic signals obtained from a sound emission or crying9. The most widely used program is PRAAT software, originally designed for instrumental phonetics, but has great capabilities for acoustic signal analysis and spectrography. This software has been used for acoustic analysis of pathological voices10.
PRAAT is computer program analyzing, synthesizing, and manipulating vocal sounds, record a sound with any other audio input device, or audio file. It was developed since 1992 by Paul Boersma and David Weenink at Institute of Phonetic Sciences at University of Amsterdam. There are versions for most common operating systems: Macintosh, Windows, Linux11. It has been possible identify irregularities present during crying episode, such as abrupt variations in tone12.
Acoustic analysis of crying, can analyze fundamental frequency (F0), it is frequency with which vocal cords vibrate during production of sounds originating from vocal cords and measured in Hz13. It has been suggested fundamental frequency (F0) crying in 4-month-old infants can predict F0 speech expressions after 5 years of age14. However, acoustic characteristics of crying are directly influenced by child's physical and psychological state or by external factors. Differences in F0 of crying have been determined in patients with brain damage, cleft palate, hydrocephalus, sudden infant death syndrome and many other diseases15.
Due to anatomical alterations in vocal tract presented by patient with a cleft palate, pronunciation of the first words can be produced at 2 years of age. Due crying emissions can be obtained in accessible way during preoperative evaluation, following objective is proposed: to determine fundamental frequency (F0) of spontaneous crying in patients with pre and postoperative cleft palate, and compare results with healthy control group with PRAAT software.
MATERIALS AND METHODS
A population of 21 patients with cleft palate was obtained, who attended Oral and Maxillofacial Surgery Service "Dr. Atilio Perdomo" of University Hospital "Dr. Ángel Larralde" in Valencia-Venezuela, in period between January 2017 November 2019; study was approved by University of Carabobo and "Dr. Ángel Larralde" University Hospital, all representatives of patients signed an informed consent agreement (Approval of Committee on Bioethics and Human Research No. 16-1225).
A sample 16 patients was obtained, who met following inclusion criteria:
Patient with a diagnosis of cleft palate with a history of cheiloplasty.
Patients with isolated secondary cleft palate.
Age between 18 months to 30 months.
nformed consent.
Patient without associated systemic changes.
Study of normal audiometry.
Compliance with postoperative controls.
The type of cleft palate was determined by Veau's classification. Patients who did not meet aforementioned criteria were excluded. Control group from 10 patients, grouped by gender. Study protocol to be carried out was explained to representatives, informing is of voluntary participation complying with informed consent, as well as a clinical evaluation to rule out present pathologies or systemic alterations.
In the study, representatives of patient and control group were in a room without sonic contamination; study was explained, to filled the medical record, where recording of participant's spontaneous cry was approximately 60 seconds, recorded digitally on a VIT M2400 laptop with Realtek High Definition audio 6.0.1.6029 microphone. Distance from mouth microphone was 10 cm, spontaneous crying emissions were analyzed with PRAAT Software Voice Report version 4.6.06. Audios with background noise were excluded.
Patients with cleft palate, complementary studies were carried out with preoperative protocol, later, underwent surgical intervention where primary palatoplasty was performed, patients underwent surgery by same surgeon, and postoperative control was verified, which was maintained without complications. Recordings were made in 3 stages in the patients: preoperative and late postoperative in 6 months, and then results are compared with control group (Figure 1 and Figure 2).
SPSS version 19.0 (IBM SPSS Statistics) was used perform all statistical analyzes. Through, dependent variants, F0 of spontaneous crying changes in patients with cleft palate are evaluated with their preoperative and postoperative control at 6 months, and are subsequently compared with control group. Independent variant tests were performed to assess relationship F0 to gender.

Figure 1. Acoustic analysis of spontaneous crying in patients with cleft palate in preoperative control.
RESULTS
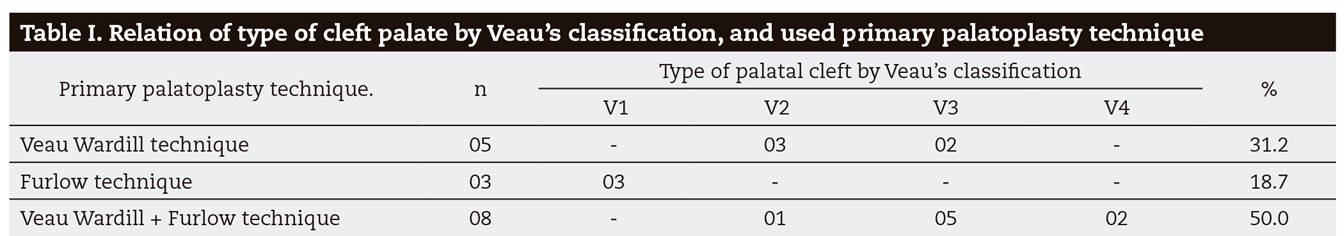
A 56.3 % (n = 9) was obtained in female and 43.8 % (n = 7) for male, representing an average age of 25.8 months (DV = 3.98). Regarding primary palatoplasty surgical procedure, using Veau Wadrill technique (n = 5), Furlow technique (n = 3), and combination of both primary palatopasty techniques (n = 8), being the most frequent with 50 %, no sequelae were observed during postoperative control. Table 1 shows relationship of type of cleft palate by Veau's classification with surgical technique used.
A total of 52 spontaneous crying recordings were analyzed, divided by preoperative, postoperative and control group audio. Used PRAAT software, it was determined duration of spontaneous crying episode was 2.13 seconds in patients with cleft palate (DV = 0.76), compared to control group, was 2,7 seconds (DV = 0.66). Regarding fundamental frequency (F0) of spontaneous crying, preoperative average Pitch value of 349.125 Hz (DV = 35,335) was obtained. Subsequently, in postoperative control average Pitch 369.775 Hz (DV = 41,387) was obtained, evidencing significant results with an increase in F0 postoperative control of spontaneous crying, reporting more acute type crying emissions (p < 0.000) represented in Table 2. Compared with control group, average F0 of spontaneous crying Pitch value of 437.103 Hz (DV = 38,170) was obtained, presenting similar values with postoperative group (p < 0.000), represented Table 3. In addition, no significant differences were reported between F0 and gender (p > 0.383).
DISCUSSION
In this study, fundamental frequency (F0) of spontaneous crying in patients with cleft palate was determined through acoustic analysis. From results of study, a comparison was made with control group, determining difference between them. Statistical analyzes were performed to compare significant difference between clinical group and the control group.
Regarding results, there were no differences in results of F0 of crying with respect to gender, presenting similar values in the investigations carried out by Reby et al.16, Lee et al17. Furthermore, gender patterns of F0 appear from 11 years of age17. Therefore, data for both genders were pooled in study.
Regarding surgical procedure, Gart & Gosain recommends an evaluation at 3 months after surgical procedure in patients to rule out velopharyngeal insufficiency18; Because alteration can occur in 5 % to 35 % after a primary palatoplasty, reported by Yamaguchi19. However, there are acoustic findings in patients with velopharyngeal insufficiency, which may have low F0 values, established in evaluation of the voice20. In the study, no late postoperative sequelae were evidenced; this may be related early and timely surgical resolution in patients.
Fundamental frequency (F0) was also analyzed, showing more acute spontaneous crying emissions in postoperative control. These data are in agreement with results established by Wermker et al, reporting differences in spontaneous crying parameters (FO and PPQ (Tone Disturbance Ratio) between patients with cleft lip palate and healthy control group21. F0 medians of healthy control group of the study presented the ranges established in previous publications22. Research normal range of F0 during crying is reported, this depends on situations such as pain, hunger, irritation, among others23,24. But, Rothgänger in 2003 suggests that range decreases as the infant grows25.
Few studies have been found report use of acoustic analysis of crying in patients with cleft palate, compared pre and postoperative control through primary palatoplasty. With these data, early detection of alterations present in vocal tract can be carried out in patients with cleft palate in the postoperative period, avoiding the abnormal development of language and speech. Updating these data will help the scientific community to guide future research. Therefore, informing about changes present in F0 of pre and postoperative crying, will help choose treatment in a timely manner in patients with cleft palate. It is important to highlight, to results obtained in this study are predictive data regarding vocal development of patient. For this reason, we recommend long-term follow-up of the patients, once the vocal language has been established in them, to evaluate verbal and progressive development of same; through studies such as acoustic analysis of voice. If vocal changes appear during follow-up, a careful examination should be performed to rule out abnormalities such as velopharyngeal insufficiency.
CONCLUSION
Fundamental frequency (F0) of spontaneous crying in patients with cleft palate presented an increase of 15.5 % in postoperative controls, compared to control group. In addition, there were no significant differences with respect surgical technique used; therefore, performing an early and timely surgical resolution would avoid sequelae during development of speech. It should be noted acoustic analysis of crying is quick, simple and non-invasive procedure; being a complementary tool for evaluation of postoperative control of primary palatoplasty. The evaluation of patients with cleft palate must be carried out in a multidisciplinary way, returning function not only of swallowing but also of speech.