Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Cirugía Oral y Maxilofacial
versão On-line ISSN 2173-9161versão impressa ISSN 1130-0558
Rev Esp Cirug Oral y Maxilofac vol.44 no.1 Madrid Jan./Mar. 2022 Epub 25-Abr-2022
https://dx.doi.org/10.20986/recom.2022.1353/2022
EDITORIAL
Operative arthroscopy and mouth opening in TMJ internal derangement
1M.D., Ph.D., FEBOMFS. Director de la Revista Española de Cirugía Oral y Maxilofacial. Miembro activo de la European Society of Temporomandibular Joint Surgeons (ESTMJS), Miembro internacional de la American the Society of Temporomandibular Joint Surgeons (ASTMJS), Miembro Facultativo de TMJ S.O.R.G. Revista Española de Cirugía Oral y Maxilofacial. España
Some still insufficient attempts have been made in the literature to try to elucidate the effectiveness and even superiority of operative arthroscopy (OA) (also called arthroscopic surgery, AS) over the simpler arthroscopic lysis and lavage (ALL). One of most serious tries is the meta-analysis by Al-Moraissi1, from Thamar University (Yemen) in 2015, in which the author performed a quantitative evaluation of the existing most relevant published series concerning the clinical outcomes of three surgical methods for treating internal derangement (ID) of the temporomandibular joint (TMJ), including arthroscopic lysis and lavage (ALL), arthroscopic surgery (AS) and open surgery.
Regarding comparison of AS versus ALL, the authors reported in their abstract and conclusion sections that "ALL provides greater improvement in maximal interincisal opening (MIO) and comparable pain reduction when compared to AS". When specifically dealing with mandibular function evaluated by MIO, this statement needs to be clarified. When analyzing the results section of the meta-analysis, the author states that "there was a significant difference in favor of patients treated by AS with regard to improvement in MIO". This asseveration was also confirmed in their forest plot comparing ALL versus AS for ID of the TMJ in terms of MIO in millimeters, showing some advantage for AS over ALL in terms of mouth opening. Trying to go deeper into this idea, in the discussion section the author stated that "concerning AS versus ALL, there was a significant improvement in joint movement for patients managed with AS (p = 0.0001)". It is imperative to congratulate the author for his exhaustive work in carrying out this meta-analysis, but also to alert the reader to this discrepancy, which can be misleading if only the summary or conclusion sections are taken into account, in a shallow approach. In short, a careful reading of the results of this meta-analysis shows that, statistically, the use of AO is more effective in increasing MAO than ALL, even though the latter achieves a great improvement in oral opening and a comparable reduction in pain.
Several arthroscopic techniques for the management of TMJ ID has been reported, from the simpler ALL to the more complex OA. In most of cases ALL is performed by a single-puncture in the fossa puncture site together with an outflow needle placed anteriorly until a continuous irrigation with lactated Ringer´s solution is obtained. Here, lysis of adhesions is directly performed with the arthroscope by means of sweeping maneouvres2. When performing the more advanced and complex OA, a second and/or third cannula ("working cannulas") are inserted by triangulation technique, as described by McCain3, to allow the introduction of instrumentation into the joint to perform several procedures, such as: 1) anterior release of the disc by myotomy of the upper belly of the lateral pterygoid muscle (Figure 1)4; 2) electrocoagulation (electrocautery or radiofrequency) of areas of synovitis, fibrillation (adherences, pseudowalls), and also over the swelled bilaminar zone (electrocoagulation of the posterior ligament) (Figure 2); 3) functional suture discopexy or disc rigid fixation with resorbable pins; 4) motor debridement; and 5) removal of loose bodies or clots; among others. All these procedures can be complemented by subsinovial infiltration of corticoids or plate rich plasma, and intraluminal instillation of hyaluronic acid, among others.
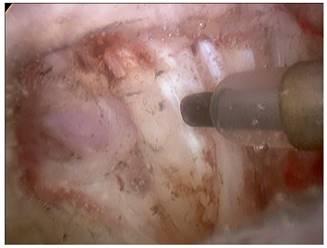
Figure 1. Disc anterior release by myotomy of the lateral pterygoid muscle using a radiofrequency probe.

Figure 2. Electrocautery of synovitis of the retrodiscal tissues of the posterior ligament using a radiofrequency probe.
In general, the main advantage obtained by carrying out meta-analyses is the possibility of obtaining new information that may be absent from individual clinical series, such as those studied here, in which significant good results in terms of pain reduction and mandibular function were observed for both ALL and OA5,6. As it is concluded from this meta-analysis1, with the caution of studies with a moderate risk of bias being included and also because of the scarce number of available studies, we should have to focus our attention on the finding that OA may be great value when treating patients with ID and restricted mandibular motion as better results in terms of MIO should be expected over ALL.
Of course, more controlled clinical trials should be desirable to explore these specific findings. Also, since the learning curve for TMJ arthroscopy is long and even more for OA, training programs for residents have to stress the importance of minimally-invasive techniques for treating TMJ disease due to their proven effectiveness and minimal morbidity in comparison to open surgery
BIBLIOGRAFÍA
1. Al-Moraissi EA. Open versus arthroscopic surgery for the management of internal derangement of the temporomandibular joint: a meta-analysis of the literature. Int J Oral Maxillofac Surg. 2015;44(6):763-70. DOI: 10.1016/j.ijom.2015.01.024. [ Links ]
2. González-García R, Gil-Díez-Usandizaga JL, Rodríguez-Campo FJ. Arthroscopic anatomy and lysis and lavage of the temporomandibular joint. Atlas Oral Maxillofac Surg Clin N Am. 2011;19(2):131-44. DOI: 10.1016/j.cxom.2011.05.002. [ Links ]
3. McCain JP. Arthroscopy of the human temporomandibular joint. J Oral Maxillofac Surg. 1988;46(8):648-55. DOI: 10.1016/0278-2391(88)90107-3. [ Links ]
4. González-García R. Arthroscopic myotomy of the lateral pterygoid muscle with coblation for the treatment of temporomandibular joint anterior disc displacement without reduction. J Oral Maxillofac Surg. 2009;67(12):2699-701. DOI: 10.1016/j.joms.2009.07.089. [ Links ]
5. González-García R, Rodríguez-Campo FJ, Monje F, Sastre-Pérez J, Sastre-Pérez J, Gil-Díez-Usandizaga JL. Operative versus simple arthroscopic surgery for chronic closed lock of the temporomandibular joint: a clinical study of 344 arthroscopic procedures. Int J Oral Maxillofac Surg. 2008;37(9):790-6. DOI: 10.1016/j.ijom.2008.04.022. [ Links ]
6. González-García R, Rodríguez-Campo FJ. Arthroscopic lysis and lavage versus operative arthroscopy in the outcome of temporomandibular joint internal derangement: a comparative study based on Wilkes stages. J Oral Maxillofac Surg. 2011;69(10):2513-24. DOI: 10.1016/j.joms.2011.05.027. [ Links ]











 texto em
texto em 


