INTRODUCTION
Dingman and Grabb were the first to describe the dislocation of the mandibular condyle into the middle cranial fossa (DMCCF) in 1963 as a very unusual1. The latest sistematic review and meta-analysis about this kind of fractures, made by Diez-Suarez et all and published in 2021, described 72 cases reported in the English literature of DMCCF1,2. Most of the events took place in the young and female population, and this was more frequently associated with motor vehicle accidents (> 50 %) or bicycle injuries3.
Clinically, DMCCF includes anterior open bite with posterior early contact, limited mouth opening normally with less than 20 mm and restriction of mandibular movements4. Compurerized tomography scans possess an increased sensitivity and specifivity. Magnetic resonance imaging could be useful to diagnose injured soft tissues5.
Treatment of these injuries requires an interdisciplinary approach to evaluate the possible neurological injuries caused by the reduction of the intruded condyle from the middle cranial fossa. This reduction could be done by open reduction with preauricular approach, or closed reduction. Although there are case reports and reviews in the literature, none have documented a definitive clinical evaluation and treatment algorithm6.
CASE REPORT
A 17-year-old patient came to the emergency room due to pain in both temporomandibular joints, anterior open bite with bilateral posterior premature contact and impossibility of mouth opening after suffering a car crash.
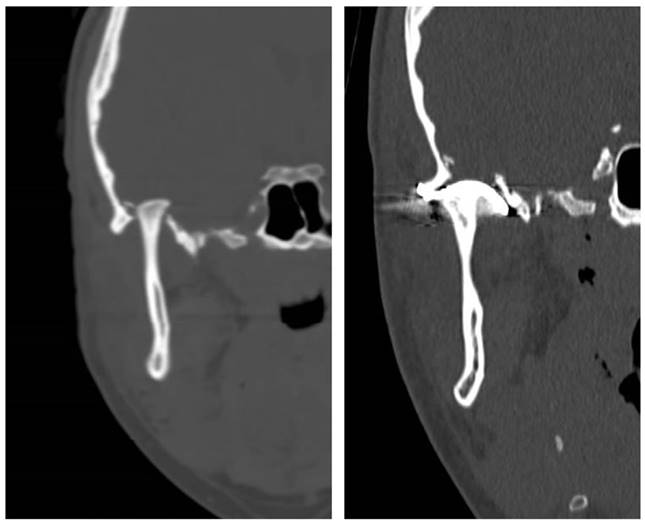
After making a CT SCAN, fracture of the right mandibular glenoid cavity with intracranial displacement of the right mandibular condyle located in the middle cranial fossa was described (Figure 1). Therefore, we decided to perform urgent surgery in the first 24 hours.
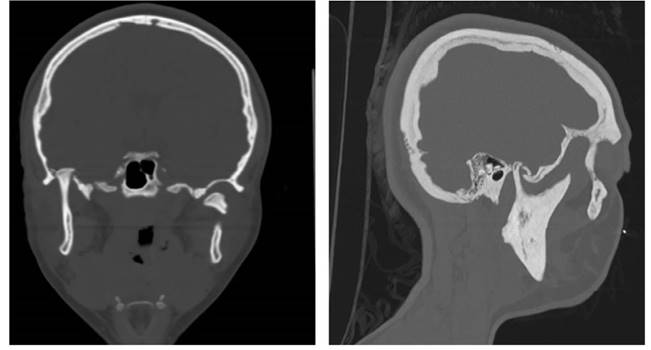
Figure 1. CT scan with coronal and sagittal cut. A fracture of the right glenoid fossa with impaction of the condyle in the middle cranial fossa and a fracture of the neck of the left condyle with posteriomedial displacement is observed.
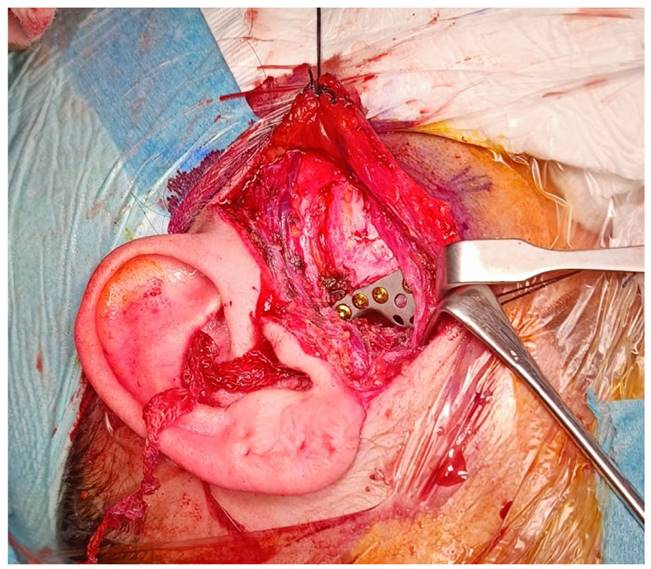
Under general anesthesia and nasotracheal intubation. First, a right preauricular approach was performed to reach the superior joint space, observing the impacted condyle in the middle cranial fossa with a fracture of the glenoid cavity. Using intraoral pressure in lower right molars, condyle disimpaction of the temporal fossa was achieved, observing the integrity of the dura mater and the absence of cerebrospinal fluid outflow. As the bone defect in the glenoyd fossa was from 12 to 15mm, the reconstruction was performed with a stock Christensen TARMA n.º 11 glenoid fossa prosthesis of stock and fixation with six 5mm screws, with correct reconstruction and reduction of the condyle to a neofossa (Figure 2). In a second stage, a left preauricular and transparotid approach was performed with reduction and fixation with a delta-shaped plate and four 5 mm screws was performed.
After a 12-month follow-up, the patient presents a 35 mm oral opening with correct occlusion like before the fracture. The posterior premature contact and anterior open bite were resolved after both fracture reduction. She has not presented infectious clinic in any fracture. She presented paresis of the frontal branch of the left facial nerve due to the surgical approach, resolved in 4 months with exercises and corticosteroids (Figure 3).
DISCUSSION
To date 72 cases have been reported in the English literature in the latest sistematic review. Most of the patients were female with an average age of 23.4 years. The main etiology of DMCCF was a motor vehicle accident. However, in more tan half of the patients aged 18 years or younger, the etiology was attributed to falls or bicycle accidents1,2. In the case described in this article, the patient was female with 17 years old and suffered an accident while traveling in the back of a car without seat belt, suffering direct trauma to the mental area.
There is no adequate consensus for the treatment of this type of fracture. Arya V et all in 2016 after a literature review, indicate that closed reduction is the chosen treatment option when the injury is recognized early, usually within 2 weeks after trauma, in younger children (< 12 years old) and in patients with no evidence of ipsilateral condylar fracture3,7. On the other hand, open reduction could be chosen when there is a comminution of the temporal bone with associated cerebral injuries that require a neurosurgical intervention, in cases of failed closed reduction, in patients with late diagnosis (> 2 to 4 weeks after trauma), the presence ot coexisting ipsilateral condylar fracute, gross vertical inestability, bony interference between the condyle and the fractured fossa, or high risk of hemorrhage from middle meningeal artery that can be caused by sharp bone fragments during manipulation. Another described options to close de glenoid fossa defect would be the temporoparietal fascia and the temporalis muscle flap8,9.
In the published 72 cases, reconstruction was performed in 28 cases. Only two of them (Rikhotso and Bobat in 2016 and Lindell and Thor in 2017) were reconstructed using a TMJ prothesis, and both were total alloplastic reconstruction, using a condyle and glenoyd fossa prosthesis with good results in a long term follow up. Our case is the first to use a partial TMJ prosthesis, reconstructing only the glenoid fossa and maintaining the condyle that had not been fractured, with good results in a follow up of 12 months10,11.
In some other cases in which open treatment was performed, condyle reduction was not possible, and arthroplasty procedures were performed by means of condylectomy, condylotomy or ankylotic bloc removal. Bone grafts alone were used to reconstruct the glenoyd fosa defect in two cases, in association with a temporalis muscle flap in four, with a titanium plate in one, and with a titanium mesh in one case. Other materials used alone were fascia lata, Gelfoam(®), Duragen(®), Gore-tex(®), and ear cartilage12 (Figure 4).
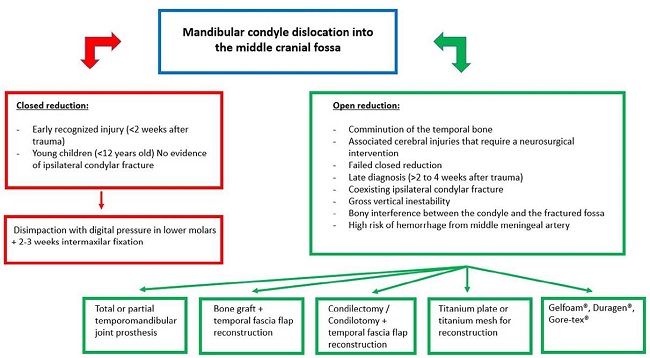
Figure 4. Diagram with a summary of the indications for open or closed reduction, as well as the different therapeutic options.
We opted for open reduction because, through the preauricular approach and directly observing the disimpaction of the fracture, we could see if there was a cerebrospinal fluid fistula and injury to the dura mater. After disimpacting the condyle of the cranial middle fossa, the complete integrity of the dura mater and the absence of a cerebrospinal fluid fistula were observed, so it was decided to reconstruct the glenoid cavity with a glenoid fossa prosthesis, because of the future possibility of a new displacement of the condyle into the middle cranial fossa, as well as the big diameter (12-15 mm) of the cranial base defect. We opted for a stock prosthesis due to the inmediate need of the material to reduce the fracture in the first 24 h. A customized prosthesis could be used but it would delay the surgery until the plannification is made and the costs would increment. Subsequently, the correct oral opening of the patient with correct occlusion and proper functioning of both temporomandibular joints was verified.
CONCLUSION
The election of a glenoid fossa prosthesis to treat a glenoid fossa fracture with dislocation of the condyle to the middle cranial fossa and thus avoid its recurrence is a valid option, with satisfactory results and no complications in a 12-month follow-up. However, new studies should be carried out with a larger number of patients.