Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Neurocirugía
versão impressa ISSN 1130-1473
Neurocirugía vol.17 no.6 Dez. 2006
Time sparing and effective procedure for dural closure in the posterior fossa using a vicryl mesh (Ethisorb®)
Cierre de duramadre en cirugía de fosa posterior con una malla de vicryl (Ethisorb®): un procedimiento simple y efectivo
I. Reyes-Moreno and R. Verheggen
Department of Neurosurgery. University Hospital and School of Medicine. Gottingen. Germany.
SUMMARY
Introduction. Dural defects and cerebrospinal fluid (CSF) leaks are a common problem following posterior fossa surgery. The management includes either nonoperative management (e.g. external lumbar drainage) or surgical re-exploration.
Objectives. We present our surgical, clinical and histopathological experience of dural closure in the posterior fossa. In order to avoid CSF leaks we developed a simple but effective and time-sparing method using a well-cut sheet of a vicryl-poly-pdioxanone mesh (Ethisorb®) covering the whole defect of the craniectomy. Additional fibrin glue or sealant is not necessary. Special attention was focused upon the frequency of postoperative complications, in particular infection rate and CSF leaks.
Patients. 85 patients were treated with vicryl mesh as dural substitute after posterior fossa surgery due to distinct pathologies. An illustrative case is presented.
Results. In none of the patients a postoperative infection was observed. Four patients presented postoperative CSF leakage and were treated by percutaneous lumbar drainage. Three of the patients improved completely, requiring no additional treatment. Only in one case defect covered by a vicryl mesh, a surgical reexploration became necessary.
Conclusion. We consider the vicryl mesh (Ethisorb®) as an ideal dural substitute especially for the dural closure of the posterior fossa.
Key words: CSF leaks. Dural closure. Dural substitutes. Posterior fossa surgery. Vicryl mesh.
RESUMEN
Introducción. Los defectos en el cierre de duramadre y por consiguiente fístulas de líquido cefalorraquídeo son comunes en cirugía de fosa posterior. El tratamiento incluye manejo conservador o no quirúrgico como drenaje lumbar externo de líquido cefalorraquídeo, cuando éstas medidas fallan se requiere de una nueva cirugía.
Objetivos. Con el propósito de evitar fístulas de líquido cefalorraquídeo en cirugía de fosa posterior desarrollamos un método simple, pero efectivo, que permite ahorrar tiempo quirúrgico utilizando una malla de viyril-poly-p-dioxanone (Ethisorb®) para cubrir por completo el defecto de la craniectomía. No se requiere del uso adicional de adhesivo de fibrina. Nuestra experiencia clínica, quirúrgica y hallazgos histopatológicos con ésta técnica de cierre dural se discuten en el presente artículo así como las complicaciones, en particular infección y presencia de fístulas de líquido cefalorraquídeo.
Pacientes. En 85 pacientes sometidos a cirugía de fosa posterior debida a diferentes patologías, se utilizó una malla de vicryl (Ethisorb®) como sustituto de duramadre. Se presenta un caso que ilustra nuestra técnica.
Resultados. En ninguno de los casos se presentó infección postoperatoria. Cuatro casos presentaron fístula de líquido cefalorraquídeo y fueron tratados con drenaje lumbar externo; tres pacientes mejoraron por completo sin requerir otras medidas. Sólo en un caso se requirió de exploración quirúrgica.
Conclusiones. De acuerdo con los resultados y complicaciones, consideramos que la malla de vicryl (Ethisorb®) es un sustituto de duramadre ideal, en particular para cirugías de fosa posterior.
Palabras clave: Cierre dural. Cirugía de fosa posterior. Duramadre. Fístulas de LCR. Malla de vicryl.
Introduction
Postoperative cerebrospinal fluid (CSF) leakages have been a significant problem, particularly in posterior fossa surgery. A watertight dural closure is often impossible in cases with friable dura or in cases where the dura is resected. Therefore, repair of dural defects is imperative to avoid complications such as continuous loss of CSF, infections, cerebellar herniation as well as adhesions between cerebellum and the overlying tissue.
Many different materials have been used as dural substitutes including muscle patch25, fascia lata23,25, pericranium25, freeze-dried cadaveric dura mater5 or porcine lyophilised dura16. Although some of the aforementioned materials have proved to be satisfactory, many of the alloplastic materials remained permanent foreign bodies13 so that the use of these substitutes was often complicated by intense inflammatory responses6, delayed extrusions27, late haemorrhages3,15, and acute or chronic infections6,9,27. Application of a biological dural substitute as freeze-dried human dura is limited due to its reported association with Creutzfeldt- Jacob disease10,18,26. An adequate quantity of ideal substitutes like pericranium, muscle, and temporal fascia may sometimes be difficult to obtain. Furthermore, the use of fascia lata requires another operative procedure with the risk of complications.
Experimental investigations proved vicryl (polyglactin 910) to be easily malleable, relatively inexpensive and absorbable over time eliciting only minimal inflammatory response12. Due to its special features, a vicryl mesh seems to be particularly suitable for the repair of dural defects.
We evolved a simple method to avoid CSF leaks following posterior fossa surgery, facilitating a swift and definite dural closure with a composite mesh (Ethisorb®) consisting of polyglactin 910 (vicryl) and poly-p-dioxanone (PDS).
Patients and methods
Between July 1992 and October 2005, 85 patients sustaining posterior fossa operations (midline or paramedian suboccipital craniectomy) due to distinct pathologies (tumours, metastasis, cerebellar haemorrhages, cerebellar infarctions, microvascular decompressions, developmental anomalies, e.g. Arnold Chiari malformations) were treated with vicryl mesh as dural substitute.
Operative technique
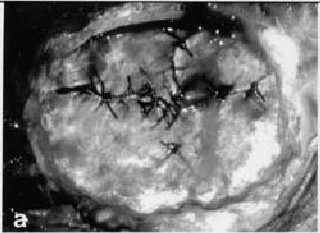
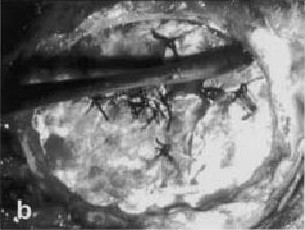
In 85 patients with dural defects after removal of space-occupying processes or tumours, a sheet of a composite mesh consisting of vicryl (polyglactin 910) and polyp-dioxanone (PDS) (Ethisorb®, Ethicon, Norderstedt; Germany) was used to achieve satisfactory dural closure. The dural borders were bluntly dissected, appropriate to the limits of the craniectomy, then a sheet of Ethisorb® was cut to size and fitted into the defect of the craniectomy so that the whole area was completely covered by the vicryl mesh (Fig 1 a-d). Neither fibrin sealant nor any special suture was necessary in order to secure the mesh.
 |  |
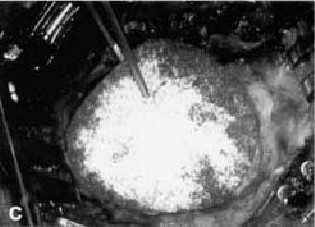 | 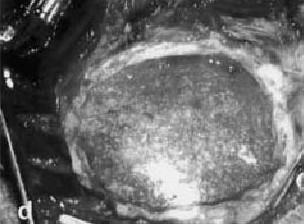 |
Figura 1 a-d. Operative technique. Craniectomy area exposed and dural defects after incomplete closure (a).
The dural borders were bluntly dissected appropriate to the limits of the craniectomy (b).
Then a sheet of Ethisorb® was cut to size (c) and fitted into the defect of the craniectomy
so that the whole area was completely covered by the vicryl mesh (d).
Ilustrative case
On hospital admittance, an 81-year-old woman complained about nausea, vomiting, vertigo, dysmetria, and gait disturbance. Computed tomography (CT) and magnetic resonance (MR) images revealed a tumour in the left cerebellar hemisphere with extensive perifocal oedema. After suboccipital craniectomy and resection of the metastasis, the margins of the dura were roughly stitched together and the whole defect of the craniectomy was covered with a well-fitting sheet of (Ethisorb®) (Fig 2) Follow-up CT scans 11 months after the first operation demonstrated a relapse of the cerebellar metastasis. Intraoperative findings showed the dura formerly covered by a vicryl-mesh, being thicker and more resistant. There were no significant adhesions to the cerebellar cortex. Biopsies were taken from the residue of the dural substitute and ordinary dura to perform histopathological examination.
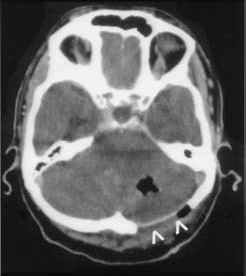
Figura 2. CT scan of a 81-year-old woman (ilustrative case)
arranged within 24 hours after posterior fossa surgery.
The dural substitute (Ethisorb®) can be easily
identified by its hyperdense and
sharply defined configuration (^^).
Histopathological Examination
Histopathological analysis revealed a complete absorption of the vicryl mesh without any evidence of inflammatory reaction. Small vessel proliferation was observed in the dura previously covered by Ethisorb®. Due to a resorption time of more than 180 days, these foreign bodies were probably the remains of poly-p-dioxanone filaments never observed in ordinary dura24.
Results
In 85 patients sustaining posterior fossa surgery, a sufficient dural closure was achieved covering the defect of the craniectomy completely with a suitable sheet of Ethisorb®. In none of the patients a postoperative infection was observed. However, 4 patients presented postoperative CSF leakage and were treated by percutaneous lumbar drainage. 3 of the patients improved completely, requiring no additional treatment. Only in one case of a huge tentorial meningioma with an extensive dural defect covered by a vicryl mesh, a surgical re-exploration became necessary thus covering the defect zone with fascia lata. In two patients re-operated due to relapsing metastasis we o bserved thick layers of fibrous tissues covering the dura, but only insignificant cortical adhesions that were easily removed. We did not find inflammation reaction.
Discussion
Particularly in posterior fossa surgery, dural defects are a significant problem. CSF leakage, once established, is not only difficult to manage in a conservative manner (e.g. external lumbar drainage) but some source of additional morbidity and even a risk of mortality4. A watertight suture seems to be the optimal method of dural repair. However, especially in cases of posterior fossa surgery, a sufficient closure of friable dura is often impracticable necessitating the use of dural substitutes.
Dura mater grafting has been practised since the late 19th century1,2. In between, different types of dural substitutes have been used including metallic foils2,20, nonviable membranes, e.g. amniotic membranes, autologous grafts such as temporal fascia, pericranium, fascia lata22, homologous grafts like freeze-dried and lyophilised dura22, heterologous materials such as porcine dermis16 or silastic coated Dacron3,17. In the late seventies, Vicryl (polyglactin 910) was more often used as suture material7 causing only minimal inflammatory reaction in non-neural tissue. Subsequent progress was the development of a vicryl mesh as a material for dural repair. In 1985, Maurer and McDonald11 experimentally investigated the effectiveness of vicryl meshes as dural substitutes in dogs and described no significant formation of cortical adhesions. In their view, the vicryl mesh seemed to be an ideal dural substitute because of the following characteristics: well tolerated, readily available and inexpensive. In 1989, Nussbaum and co-workers investigated the use of vicryl mesh as a dural substitute and described a limited epidural scar formation after laminectomy14 proving vicryl mesh to be a safer method without evidence of postoperative neural compression. Woven vicryl prosthetic meshes are biodegradable and replaced by connective tissue within 45-60 days11,12 thereby stimulating the process of dural regeneration. However, the mesh alone did not guarantee in all cases a watertight dural closure and seal against CSF leakage24. A vicryl mesh coated with bovine collagen was tested as dural prosthesis12,21. Although these experimental studies were encouraging, Gudmundson and Sagaard8 recently associated postoperative infections with the use of a collagen coated vicryl mesh as dural substitute.
We used pure (without collagen bovine) vicryl meshes and unlike the aforementioned authors, we did not observe any increase in wound infections. Certainly, we endeavour to perform a watertight dural closure with separate or continuous stitches. But when friable dura tears and fissures or gaping dural defects remain, we cover the whole defect of the craniectomy with a properly fitting piece of vicryl mesh. Ethisorb® (vicryl)-mesh can be easily and briefly cut to any size and shape desired. Furthermore, this material is malleable but at the same time sufficiently tough and stiff. Our special technique of dural closure saves time and costs, requiring neither fibrin glue nor suture material to fix the dural substitute. In comparison with Gudmundson and Sogaard8, we exclusively used the pure vicryl mesh. In two patients re-operated due to relapsing metastasis we observed thick layers of fibrous tissues covering the dura, but only insignificant cortical adhesions that were easily removed. We did not find any inflammatory reaction. Therefore we believe that intraoperatives findings using vicryl-collagen dural substitute and higher infection rates can be explained by an inflammatory reaction attributable to bovine collagen and its immune response.
Conclusions
Our method using a well-fitting piece of Ethisorb® permits a rapid and effective dural closure. Due to its remarkable features, the vicryl mesh seems to be an ideal dural substitute, especially in cases of posterior fossa surgery.
References
1. Abbe, R.: Epylepsy from cortical cicatrix: trephining; subdural implantation of rubber tissue. Ann Surg 1897; 25: 95-96. [ Links ]
2. Beach HHA. Gold foil in cerebral surgery. Boston Med Surg J 1897; 136: 281-282. [ Links ]
3. Banerjee, T., Meagher, J.N., Hunt, W.E.: Unusual complications with use of Silastic dura substitute. Am Surg 1983; 40: 434-437. [ Links ]
4. Cain, J.E., Dryer, R.F., Barton, B.R.: Evaluation of dural closure techniques. Suture methods, fibrin adhesive sealant, and cyanoacrylate polymer. Spine 1988; 13: 720-725. [ Links ]
5. Campbell, J.B., Bassett, C.A.L., Robertson, J.W.: Clinical use of freeze-dried human dura mater. J Neurosurg 1958;15: 207-214. [ Links ]
6. Cohen, A.R., Aleksic, S., Ransohoff, J.: Inflammatory reaction to synthetic dura substitute. J Neurosurg 1989; 70: 633-635. [ Links ]
7. Conn, J., Oyasu, R., Welsh, M., Beal, J.M.: Vicral (Polyglactin 910) Synthetic absorbable sutures. Am J Surg 1974; 128: 19-23. [ Links ]
8. Gudmundson, G., Sogaard, I.: Complications to the use of vicryl-collagen dural substitute. Acta Neurochir (Wien) 1995; 132: 145-147. [ Links ]
9.Johnson, M.H., Thompson, E.J.: Freeze-dried cadaveric dural grafts can stimulate a damaging response in the host. Eur Neurol 1981; 20: 445-447. [ Links ]
10. Lane, K.L., Brown, O., Howell, D.N., Crain, B.J., Hulette, C.M., Burger, P.C., et al.: Creutzfeldt-Jacob disease in a pregnant woman with an implanted dura mater graft. Neurosurgery 1994; 34: 737-740. [ Links ]
11. Maurer, P.K., Mc Donald, J.V.: Vicryl (Polyglactin 910) mesh as a dural substitute. J Neurosurg 1985; 63: 448 452. [ Links ]
12. Meddings, N., Scott, R., Bullock, R., French, D.A., Hide, T.A., Gorham, S.D.: Collagen vicryl - a new dural prothesis. Acta Neurochir (Wien) 1992; 117: 53-58. [ Links ]
13. Nussbaum, C.E., Maurer, P.K., McDonald, J.V.: Vicryl (Polyglactin 910) mesh as a dural substitute in the presence of pia aracnoid injury. J Neurosurg 1989; 71: 124-127. [ Links ]
14. Nussbaum, C.E., McDonald, J.V., Baggs, R.B.: Use of Vicryl (polyglactin 910) mesh to limit epidural scar formation after laminectomy. Neurosurg 1990; 26: 649-654. [ Links ]
15. Ohbayashi, N., Inawaga, T., Katoh, Y., Kumano, K., Nagasako, R., Hada, H.: Complication of silastic dural substitute 20 years after dural plasty. Surg Neurol 1994; 41: 338- 341. [ Links ]
16. O'Neill, P., Booth, A.E.: Use of porcine dermis as a dural substitute in 72 patients. J Neurosurg 1984; 61: 351-354. [ Links ]
17. Ongkiko, C.M., Keller, J.T., Mayfield, F.H., Dunsker, S.B.: An unusual complication of dura film as dural substitute. J Neurosurg 1984; 60: 1076-1079. [ Links ]
18. Penar, P.L., Prichard, J.W.: Jacob-Creutzfeldt disease associated with cadaveric dura. J Neurosurg 1987; 67: 149 150. [ Links ]
19. Pudenz, R.H., Odom, G.L.: Meningocerebral adhesions. An experimental study of the effect of human amniotic membrane, amnioplastin, beef allantoic membrane, Cargile membrane, tantalum foil and polyvinyl alcohol films. Surgery 1942; 12: 318-344. [ Links ]
20. Robertson, R.C.L., Peacher, W.G.: The use of tantalum foil in the subdural space. J Neurosurg 1948; 2: 281-284. [ Links ]
21. San-Galli, F., Darrouzet, V., Rivel, J., Baquey, C., Ducassou, D., Guérrin, J.: Experimental evaluation of colla-gen-coated vicryl mesh as a dural substitute. Neurosurgery 1992; 30: 396-401. [ Links ]
22. Sharkey, P.C., Usher, F.C., Robertson, R.C.L., Pollard, C.: Lyophilized human dura mater as a dural substitute. J Neurosurg 1958; 15: 192-198. [ Links ]
23. Thammavaran, K.V., Benzel, E.C., Kesterson, L.: Fascia lata graft as dural substitute in neurosurgery. South Med J 1990; 83: 634-636 [ Links ]
24. Verheggen, R., Schulte-Baumann, J., Hahm, G., Lang, J., Freudenthaler, S., Schaake, Th., Markakis, E.: A new technique of dural closure - experience with a vicryl mesh. Acta Neurochir (Wien) 1997; 139: 1074-1079. [ Links ]
25. Wallace, P.B., Meirowsky, A.M.: The repair of dural defects by graft. An analysis of 540 penetrating wounds of the brain incurred in the Korean War. Ann Surg 1960; 151: 174 -180. [ Links ]
26. Yamada, S., Aiba, T., Endo, Y., Hara, M., Kitamoto, T., Tateishi, J.: Creutzfeldt-Jakob disease transmitted by a cadaveric dura mater graft. Neurosurgery 1994; 34: 740-744. [ Links ]
27. Zeman, A.Z., Maurice-Williams, R.S., Luxton, R., Levene, A., Thompson, E.J., Harvey, P.: Lymphocytic meningitis following insertion of a porcine dermis dural graft. Surg Neurol 1993; 40: 75-80. [ Links ]
None of us has any financial interest or relationship with the manufeacture of "Ethisorb" (Ethicon. Norderstedt, Germany).
![]() Correspondence to:
Correspondence to:
Prof. Dr. Raphaela Verheggen.
Department of Neurosurgery.
University Hospital and School of Medicine.
University of Gottingen. Robert-Koch Str. 40.
37073 Gottingen. Germany
Recibido; 26-01-06.
Aceptado: 19-02-06
Abreviaturas. CSF: cerebrospinal fluid. LCR: líquido cefalorraquídeo.